Transcription
Provider and PharmacyDirectory 2021UnitedHealthcare Dual Complete ONE (HMO D-SNP)New Jersey - Atlantic, Burlington, Camden, Cumberland, Gloucester, Ocean and SalemcountiesFor more information, contact Customer Service at:Toll-free 1-800-514-4911, TTY 7118am-8pm: 7 Days Oct-Mar; M-F Apr-Septwww.myuhc.com/CommunityPlanH3113 005 000 PD 2021 CThis directory is current as of May 10, 2021.
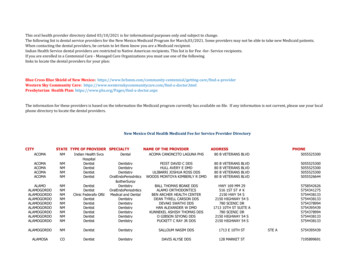
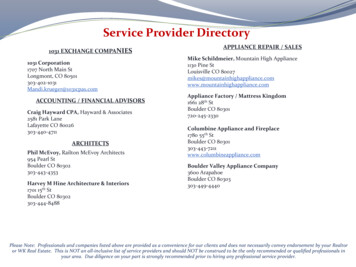
3UnitedHealthcare Dual Complete ONE (HMO D-SNP) 2021 PROVIDERAND PHARMACY DIRECTORYThis Provider and Pharmacy Directory includes information about the provider and pharmacy typesin UnitedHealthcare Dual Complete ONE (HMO D-SNP) and lists all the plan’s providers andpharmacies as of the date of this Directory. The listings contain provider and pharmacy addressand contact information as well as other details, as applicable, such as days and hours ofoperation, specialties, and skills. Key terms and their definitions appear in alphabetical order in thelast chapter of the Evidence of Coverage.Table of ContentsA. Disclaimers . 4B. Background Information about UnitedHealthcare Dual Complete ONE Network Providers . 5B1. Key Terms . 5B2. How to choose a Primary Care Provider . 6B3. How to get Managed Long Term Services and Supports (MLTSS) . 6B4. How to access UnitedHealthcare Dual Complete ONE network providers . 7B5. How to find UnitedHealthcare Dual Complete ONE providers in your area . 7C. UnitedHealthcare Dual Complete ONE List of Network Providers . 10D. Background Information about UnitedHealthcare Dual Complete ONE Network Pharmacies . 11D1. Types of pharmacies in UnitedHealthcare Dual Complete ONE . 11D2. Long-term supplies of prescriptions . 12E. UnitedHealthcare Dual Complete ONE List of Network Pharmacies . 13F1. Provider Type National Vendors . 17 Primary Care Providers . 29 Specialists . 257F2. Facility or Facility based Provider Type Skilled Nursing Facilities . 883 Hospitals . 889 Urgent Care/Surgicenters . 893 Ancillary . 897F3. Support Providers – Managed Long Term Services and Supports (MLTSS) . 1005G1. Retail and chain pharmacies . 1009G2. Home infusion pharmacies . 1033G3. Long-term care pharmacies . 1035H. Areas of Expertise . 1037I. Index of Providers . 1059J. Index of Pharmacies . 1097If you have questions, call UnitedHealthcare Dual Complete ONE at 1-800-514-4911, TTY 711,8am-8pm: 7 Days Oct-Mar; M-F Apr-Sept. The call is free. For more information, visitwww.myuhc.com/CommunityPlan.
4A. Disclaimers· UnitedHealthcare Dual Complete ONE (HMO D-SNP) is a Medicare Advantage Dual EligibleSpecial Needs Plan (D-SNP) with a Medicare contract and a contract with the New JerseyMedicaid program. Enrollment in UnitedHealthcare Dual Complete ONE (HMO D-SNP)depends on contract renewal.· The pharmacy network, and/or provider network may change at any time. You will receivenotice when necessary.· This Directory lists health care professionals (such as doctors, nurse practitioners, andpsychologists) and facilities (such as hospitals or clinics) that you may see as aUnitedHealthcare Dual Complete ONE member. This Directory also lists Managed Long-TermServices and Supports (MLTSS) providers (such as Adult Day Health and Home Healthproviders) that you may see as a UnitedHealthcare Dual Complete ONE member. We also listpharmacies that you may use to get your prescription drugs.· We will refer to these groups as “network providers” in this Directory. These providers signed acontract with us to provide you services. This is a list of UnitedHealthcare Dual Complete ONEnetwork providers for New Jersey - Atlantic, Burlington, Camden, Cumberland, Gloucester,Ocean and Salem counties.·You can get this document for free in other formats, such aslarge print, braille, or audio. Call Customer Service at thenumber at the bottom of this page.· You can call Customer Service and ask us to make a note in our system that you would likematerials in Spanish, large print, braille, or audio now and in the future.· The list is up-to-date as of the date listed on the cover, but you need to know that: Some UnitedHealthcare Dual Complete ONE network providers may have been added orremoved from our network after this Directory was published. Some UnitedHealthcare Dual Complete ONE providers in our network may no longer beaccepting new members. If you are having trouble finding a provider who will accept newmembers, call Customer Service at the number at the bottom of this page and we will helpyou. To get the most up-to-date information about UnitedHealthcare Dual Complete ONE‘s networkproviders in your area, visit www.myuhc.com/CommunityPlan or call Customer Service at thenumber at the bottom of this page. Doctors and other health care professionals inUnitedHealthcare Dual Complete ONE‘s network are listed in the sections following thisintroduction. Pharmacies in our network are listed in the sections following this introduction.You can use the Index in the back of the Directory to find the page where a provider orpharmacy is listed.If you have questions, call UnitedHealthcare Dual Complete ONE at 1-800-514-4911, TTY 711,8am-8pm: 7 Days Oct-Mar; M-F Apr-Sept. The call is free. For more information, visitwww.myuhc.com/CommunityPlan.
5B. Background Information about UnitedHealthcare Dual Complete ONE’sNetwork ProvidersB1. Key TermsYour Care Team may include doctors, nurses, counselors, or other health professionals who arethere to help you get the care you need. Your care team will also help you make a Plan of Care.This section explains key terms you’ll see in our Provider and Pharmacy Directory.· Providers are health care professionals and support providers such as doctors, nurses,pharmacists, therapists, and other people who provide care and services. Services includemedical care, Managed Long Term Services and Supports (MLTSS), supplies, prescriptiondrugs, equipment, and other services. The term providers also includes facilities such as hospitals, clinics, and other places thatprovide medical services, medical equipment, and MLTSS. Providers that are a part of our plan's network are called network providers.· Network providers have contracted with us to deliver services to members of our plan.Network providers participate in our plan. That means they accept members of our plan andprovide services our plan covers. The providers in our network generally bill us directly for carethey give you. When you see a network provider, you pay nothing for covered services.· A Primary Care Provider (PCP) is a healthcare professional who gives you routine health care.Your Primary Care Provider/PCP will keep your medical records and get to know your healthneeds over time.· Specialists are doctors who provide health care services for a specific disease or part of thebody. There are many kinds of specialists. Here are a few examples: Oncologists care for patients with cancer. Cardiologists care for patients with heart conditions. Orthopedists care for patients with certain bone, joint, or muscle conditions.· You also have access to a Care Manager and a Care Team that you choose. A Care Manager helps you manage your medical providers and services. Your Care Team may include doctors, nurses, counselors, or other health professionals whoare there to help you get the care you need. Your care team will also help you make a Plan ofCare. Everyone on your care team works together to make sure your care is coordinated. Thismeans that they make sure tests and labs are done once and the results are shared with theappropriate providers. It also means that your Primary Care Provider/PCP should know allmedicines you take so that he or she can reduce any negative effects. Your Primary CareProvider/PCP will always get your permission before sharing your medical information withother providers.If you have questions, call UnitedHealthcare Dual Complete ONE at 1-800-514-4911, TTY 711,8am-8pm: 7 Days Oct-Mar; M-F Apr-Sept. The call is free. For more information, visitwww.myuhc.com/CommunityPlan.
6B2. How to choose a Primary Care Provider/PCPYou can get services from any provider who is in our network and accepting new members.When you become a member of our plan, you will choose a Primary Care Provider/PCP who is partof our plan network. This provider will be your Primary Care Provider/PCP. You may be able tohave a specialist act as your Primary Care Provider/PCP. If you would like to use a specialist asyour PCP, call Customer Service at 1-800-514-4911, TTY 711, 8am-8pm: 7 Days Oct-Mar; M-F AprSept.If you did not choose a Primary Care Provider/PCP or would like to make a change to your PrimaryCare Provider/PCP, go to the list of providers after this introduction and choose a provider:· that you use now or· who has been recommended by someone you trust, or· whose offices are easy for you to get to.If you want help in choosing a PCP, call Customer Service at the number at the bottom of thispage.If you have questions about whether we will pay for any medical service or care that you want orneed, call Customer Service and ask before you get the service or care.B3. How to get Managed Long Term Services and Supports (MLTSS)You may be able to get MLTSS as a UnitedHealthcare Dual Complete ONE member. MLTSS ishelp for people who need assistance to do everyday tasks like taking a bath, getting dressed,making food, and taking medicine. Often, these services are provided at your home or in yourcommunity, but they can also be provided in a nursing home or hospital when necessary. MLTSS isavailable to members who meet certain clinical and financial requirements.You can talk to your Care Manager or call Customer Service (their number is listed at the bottom ofthis page) to find out if you are eligible for MLTSS.MLTSS providers are listed in this Provider and Pharmacy Directory. To find out more about theseservices, see your Evidence of Coverage. Call Customer Service at the number at the bottom of thispage to get more information on how to access these services.If you have questions, call UnitedHealthcare Dual Complete ONE at 1-800-514-4911, TTY 711,8am-8pm: 7 Days Oct-Mar; M-F Apr-Sept. The call is free. For more information, visitwww.myuhc.com/CommunityPlan.
7B4. How to Access UnitedHealthcare Dual Complete ONE’s networkprovidersYou must get all of your covered services from providers within our network. If you go to providerswho are not in UnitedHealthcare Dual Complete ONE’s network (without prior authorization), youmay have to pay for those services.Prior AuthorizationA prior authorization is an approval from UnitedHealthcare Dual Complete ONE beforeyou can get a specific service, drug, or see an out-of-network provider. UnitedHealthcareDual Complete ONE may not cover the service or drug if you don’t get approval.The exceptions to this rule are when you need urgent or emergency care or dialysis and cannot getto a provider in the plan, such as when you are away from home. You can also go outside the planfor other non-emergency services if UnitedHealthcare Dual Complete ONE gives you permissionfirst.· You may change providers within the network at any time during the year. If you have beengoing to one network provider, you do not have to keep going to that same provider. You maychange your PCP for any reason at any time. If you want to change your PCP, call CustomerService. The change will become effective on the first day of the following month.· UnitedHealthcare Dual Complete ONE works with all the providers in our network toaccommodate the needs of people with disabilities. If you need to see a provider and are notsure if they offer the accommodations you need, UnitedHealthcare Dual Complete ONE canhelp you. Talk to your Care Manager for assistance.B5. How
10.04.2021 · Provider and Pharmacy Directory 2021 UnitedHealthcare Dual Complete ONE (HMO D-SNP) New Jersey - Atlantic, Burlington, Camden, Cumberland, Gloucester, Ocean and Salem