Transcription
RESPIRATORYTHERAPISTSRaha Mirshahi, Myuri Manogaran & Brenda GambleIntroduction to the Health Workforce in Canada Respiratory Therapists1
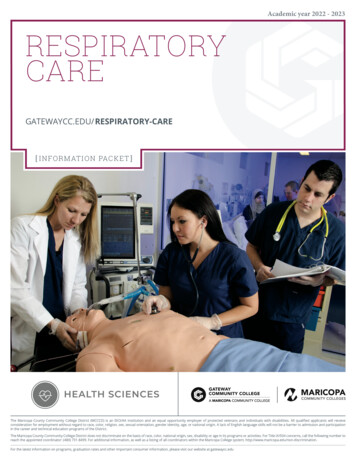
Respiratory TherapistsINTRODUCTIONRespiratory therapists (RTs) are healthcare professionalswho assess, treat, manage, control, diagnose, educateand care for patients with acute or chronic cardiopulmonary (heart and lung) disabilities or illnesses (CanadianSociety of Respiratory Therapists [CSRT], 2020b;Clark, 2012). In other words, RTs provide the carerequired to help keep patients of all ages breathing.RTs often work in collaboration with other healthcareprofessionals and can be found in a variety of settings,including intensive care units, emergency departments, operating rooms, neonatal nurseries, generalwards, outpatient clinics, specialized medical centres(e.g., sleep labs) and patients’ homes (CSRT, 2020b).When necessary, RTs also provide advanced lifesupport for extremely ill patients in institutionaland community settings.HISTORY OF THE PROFESSIONRespiratory technologies and procedures were firstintroduced to Canada following the Second World War(West, 2013; Andrews, 2006). At the end of the war,numerous army-trained surgeons’ assistants returnedto Montreal’s Queen Mary Veterans Hospital topractise. However, these men were not allowed towork as operating room nurses because, at the time,the province of Quebec allowed only women to holdsuch positions (Andrews, 2006). As a result, they wereassigned other more technical tasks, such as lookingafter oxygen tents, tank ventilators (iron lungs) andoxygen tanks, and maintaining the anesthetic equipment used in operating theatres (Andrews, 2006).Their work became known as inhalation therapy.2The need for trained individuals to support these newtechnologies and therapeutic procedures grew exponentially in the wake of multiple respiratory-relateddisease outbreaks (West, 2013). One such crisis wasthe polio epidemic in Canada. By 1953, during themost devastating wave of the epidemic, there wasan unprecedented increase in respiratory paralysis,making it a critical time for respiratory therapy. By 1960,hospitals in Montreal, Toronto, Winnipeg, Calgary,Edmonton and Vancouver all had some form of inhalation therapy department, which provided on-the-jobtraining augmented with lectures from anesthetists,nurses and technical staff (Andrews, 2006).Introduction to the Health Workforce in Canada Respiratory Therapists
Physicians played an important role in the continueddevelopment of inhalation therapy. On June 22, 1961,the case for creating a Canadian society representinginhalation therapists was successfully argued to theCanadian Medical Association (CMA) (Andrews,2006). In response, the CMA and the CanadianAnesthesiologists’ Society formed the Joint Committeeon Inhalation Therapy. It was tasked with studyingthe status of inhalation therapists, recommendingeducational qualifications for entry and establishingstandards for training programs (Andrews, 2006).Shortly thereafter, in 1964, the Canadian Societyof Inhalation Therapy Technicians was established.Education and training proved to be key issues forthe profession. A formal six-week course in inhalationtherapy started at the Hospital for Sick Children inToronto in 1962 and remained the only formal coursein Ontario until 1967 (Andrews, 2006). The schoolat the Royal Victoria Hospital in Montreal offered theonly two-year program in the country in the early1960s (Andrews, 2006).The results of the first set of examinations in 1964,which saw failure rates of approximately 20%, eventually led to the establishment of formal training programsaffiliated with community colleges. The first was set upin 1967 between a training program in Edmonton andthe Northern Alberta Institute of Technology.The role of the inhalation therapist varied across theprovinces throughout the 1960s (Andrews, 2006).In British Columbia, the role was limited to servicinganesthesia and related equipment and delivering oxygentanks to the wards. In Edmonton, technicians couldassist surgeons in performing bedside tracheotomies.By the 1970s, the role of the RT became more clinicaland began to focus on providing therapeutic servicesto patients rather than providing technical support.Introduction to the Health Workforce in Canada Respiratory TherapistsCANADIAN SOCIETYOF RESPIRATORY THERAPISTSOriginally established in 1964 as the Canadian Societyof Inhalation Therapy Technicians, the organizationlater changed its name to the Canadian Society ofRespiratory Therapists (CSRT) (West, 2013; CSRT,2020a). Since its founding, CSRT has worked tospread its vision of “empowering respiratory therapiststo provide exemplary leadership and care” and to carryout its mission to provide “leadership that advances theprofession, practice and understanding of respiratorytherapy nationally and internationally by supportingenvironments that foster innovation and knowledgetranslation, and by promoting excellence in evidence-based care” (CSRT, 2020a). Its work includes: Representing the profession on medical,government, education and advisory bodies Maintaining a national professional standardof practice Supporting and empowering RTs (personally,professionally and academically) in Canadaand around the world Working with a variety of health organizationsdealing with asthma, emphysema, smokingand more Awarding the international recognized credentialof Registered Respiratory Therapist (RRT) innon-regulated Canadian jurisdictions Publishing the Canadian Journal of RespiratoryTherapy, a peer-reviewed academic journalThe CSRT received the 2019 Award of Excellencefrom the Canadian Society of Association Executives(CSAE) (Figure 1) for demonstrating “outstandingachievement in association leadership, structure andgovernance; and/or the planning and execution ofinternal, external and integrated programs that serveyour members and/or engage external stakeholdersand volunteers” (CSAE, 2019).3
Figure 1: CSRT 2019 Award of Excellence from CSAECAREEREMPOWERINGBENEFITSNETWORKING &MENTORSHIPOPPORTUNITIES9 WINNER201LEVERAGINGTHE COMBINEDVOICE OF RTsAWARD OF CTICELOCAL ANDNATIONALADVOCACYSUPPORTSFOR PERSONALWELL BEINGSource: CSRT, 2020a https://www.csrt.com/about/As of March 31, 2020, the CSRT had 4,862 membersacross Canada, including 93 international members,642 student members and 489 members who are alsocertified clinical anesthesia assistants (CSRT, 2020a).EDUCATION AND TRAININGThe majority of RTs in Canada have graduated fromrecognized educational programs specializing in theprofession. Colleges and institutes of technology usuallyoffer diplomas or advanced diplomas after three yearsof study, while university programs are typically fouryears long. To be recognized for entry-to-practice,respiratory therapy educational programs must becertified by an approved accreditation body (CSRT,42020c). Until 2019, the Council on Accreditation forRespiratory Therapy (CoARTE), a CSRT committee,was responsible for assessing all entry-level programsfor national accreditation (CoARTE, 2015). Beginningin 2019, that role was assumed by AccreditationCanada, Canada’s leading healthcare accreditationbody (Health Standards Organization, 2020).In respiratory therapy programs, students learntheoretical subjects and undergo extensive clinicaltraining in hospital and other practice settings(e.g., community and primary care settings). Allprograms emphasize clinical education, as it isrecognized as essential in enabling students to “gainthe competencies required to provide sage, ethicalIntroduction to the Health Workforce in Canada Respiratory Therapists
and effective care in the wide variety of practicesetting in which RTs are employed” (Blais, 2008).To ensure practice readiness across a range of settings,schools typically require students to undertake clinicalrotations in the following areas: Neonatal care Paediatric critical care Adult critical care General respiratory therapeutics Cardiopulmonary diagnostics Sleep diagnostics Anaesthesia Community and primary care Chronic/long-term care Intensive careThere are currently 24 approved respiratory therapyprograms in Canada and one program in Qatar(a campus of a Canadian college) that has receivedCanadian accreditation. Table 1 lists the institutionsthat offer respiratory therapy programs, theirdepartments and their durations.TABLE 1: Canadian respiratory therapy programsLocationEducational aThompson Rivers Universitytru.ca Fast-track stream (for those who alreadyhave a Bachelor of Science)2 years Respiratory Therapy Diploma3 years Dual-credential: Respiratory TherapyDiploma and Bachelor of Health Science4 yearsNorthern Alberta Institute of Technologynait.ca Respiratory Therapy Diploma3 yearsSouthern Alberta Institute of Technologysait.ca Respiratory Therapy Diploma3 yearsManitobaUniversity of Manitobaumanitoba.ca Bachelor of Respiratory Therapy4 yearsOntarioMichener Institute of Education at UHNmichener.ca Respiratory Therapy Program –Advanced Diploma3 yearsSt. Clair College of Applied Arts and Technologystclaircollege.ca Respiratory Therapy Program –Advanced Diploma3 yearsAlgonquin College of Applied Artsand Technologyalgonquincollege.com Advanced Diploma in Respiratory Therapy3 yearsCanadore College of Applied Arts and Technologycanadorecollege.ca Advanced Diploma in Respiratory Therapy3 yearsLa Cité collégiale – Collège d’arts appliquéset de technologiecollegelacite.ca Thérapie respiratoire3 yearsFanshawe College of Applied Arts and Technologyfanshawec.ca Advanced Diploma in Respiratory Therapy100weeksConestoga College Institute of Technologyand Advanced Learningconestogac.on.ca Advanced Diploma in Respiratory Therapy3 yearsAlbertaIntroduction to the Health Workforce in Canada Respiratory Therapists5
TABLE 1: Canadian respiratory therapy programsQuebecVanier Collegevaniercollege.qc.ca Diploma in Respiratory& Anaesthesia Technology3 yearsCEGEP de Ste-Foycegep-ste-foy.qc.ca Techniques d’inhalothérapie3 yearsCEGEP de Sherbrookecegepsherbrooke.qc.ca Techniques d’inhalothérapie3 yearsCollège de Rosemontcrosemont.qc.ca Techniques d’inhalothérapie3 yearsCEGEP de Chicoutimicchic.ca Techniques d’inhalothérapie3 yearsCollège Ellis – Campus de Trois-Rivièresellis.qc.ca Techniques d’inhalothérapie et anesthésie3 yearsCollège Ellis – Campus de Longueuilellis.qc.ca Techniques d’inhalothérapie et anesthésie3 yearsCEGEP de l’Outaouaiscegepoutaouais.qc.ca Techniques d’inhalothérapie3 yearsCollège de Valleyfieldcolval.qc.ca Techniques d’inhalothérapie3 yearsNew Brunswick Community College – SaintJohnnbcc.ca Respiratory Therapy Diploma3 yearsCollège communautaire duNouveau-Brunswickccnb.ca Thérapie respiratoire120weeksQEII/Dalhousie Universitydal.ca Diploma in Respiratory Therapy3 years Bachelor of Health Science witha specialization in Respiratory Therapy4 yearsNewfoundlandand LabradorCollege of the North Atlanticcna.nl.ca Respiratory Therapy Diploma3 yearsInternationalCollege of the North Atlantic (Qatar)cna-qatar.com Respiratory Therapy Diploma3 yearsNew BrunswickNova ScotiaTo complete a respiratory therapy program,students must meet the requirements of theNational Competency Framework for theProfession of Respiratory Therapy (2016–2021).This framework outlines the required competencies6for RTs looking to enter practice, which will berequired throughout their career.The components of the framework are summarizedin Table 2.Introduction to the Health Workforce in Canada Respiratory Therapists
Figure 2: National Competency Framework for the Profession of Respiratory TherapyClinicCompetenciesAttitudes& ValuesCore CompetenciesAttitudes& ValuesPerformanceof competenciespopulationsFoundation ScienceAttitudes& ValuesSource: National Alliance of Respiratory Therapy Regulatory Bodies [NARTRB], 2016TABLE 2: National Competency Framework for the Profession of Respiratory TherapyAttitudes and values Duty to patients Duty to others Performance within competence Confidentiality Participation in continuous professional development Independence and impartiality Honesty and integrity Supervision of others Compliance with codes of conduct and practice Professional liability insurance Conflicts with moral or religious beliefs Environment and sustainability Obligation to report unsafe or inappropriate practices BehaviourIntroduction to the Health Workforce in Canada Respiratory Therapists7
TABLE 2: National Competency Framework for the Profession of Respiratory TherapyFoundation science Apply knowledge of anatomy and physiology Apply knowledge of chemistry and biochemistry Apply knowledge of physics Apply knowledge of pharmacological principles Apply knowledge of microbiology Apply knowledge of pulmonary pathophysiology Apply knowledge of cardiovascular pathophysiology Apply knowledge of other diseases and disordersCore competencies Provide evidence-informed, patient-centred respiratory care Demonstrate professional behaviour Communicate effectively Collaborate in the interdisciplinary healthcare team Optimize cardio-respiratory health and wellness of the community Demonstrate critical thinking and reasoning skills Perform administrative duties Implement preventative measures to ensure health and safety Demonstrate accountability appropriate to role in the healthcare teamClinical competencies Assess patient cardiorespiratory status Optimize patient safety Administer medication and substances Manage airway Perform anaesthesia assistance Provide optimal ventilation assistance Execute resuscitation Administer cardio-pulmonary diagnostic tests Perform adjunct therapies Perform invasive vascular proceduresDetailed descriptions of each of the featuredcompetencies, as well as the expectations to meetthese requirements according to career stage(entry-to-practice, experienced professional,senior professional, expert), can be found onthe CSRT website.CERTIFICATIONUpon graduating from an accredited respiratorytherapy program, graduates are eligible to write thenational registration examination, administered by theCanadian Board for Respiratory Care (CBRC). TheCBRC is a third-party, not-for-profit organizationthat produces and administers examinations that8evaluate candidates “for defined [RT] competenciesthat are aligned with professional competencyframeworks” (CBRC, 2020). The CBRC NationalRespiratory Therapy Examination consists of approximately 200 multiple-choice questions divided intoknowledge-based and case-based questions, whichare regularly updated to reflect the latest professionalcompetency frameworks (CBRC, 2020).To register for the exam, a candidate must have theireducational background and credentials approved bythe regulatory authority in their jurisdiction (CBRC,2020). This process is more straightforward for thosewho have graduated from and intend to practise withinIntroduction to the Health Workforce in Canada Respiratory Therapists
the same regulated jurisdiction; however, thoseeducated or aspiring to practise in non-regulatedjurisdictions can also qualify for the CBRC exam. TheCSRT acts as the credentialing body for RTs innon-regulated jurisdictions, which means anyone whohas received an education in respiratory therapy inCanada or elsewhere is eligible to present theircandidacy to the CSRT to qualify for the exam.Unsuccessful candidates and those still waiting towrite the exam hold Graduate Respiratory Therapist(GRT) status and are limited in the ways they canpractise. For example, they may not be permitted toconsult patients privately or independently, initiatecertain practices (e.g., oxygen therapy) or administercertain substances (College of Respiratory Therapistsof Ontario [CRTO], 2020). GRT status also typicallyexpires within two years. The specifics of GRT statuscan vary by jurisdiction, so it is highly advised toresearch the regulatory authority in the jurisdiction ofpractice.Upon successful completion of the CBRC exam,candidates are granted the restricted title ofRegistered Respiratory Therapist (RRT) and areeligible for CSRT membership (CSRT, 2020c). Anadditional benefit of certification is that the commonentry-to-practice standards across Canada ensureRTs can work across the country in a relativelyseamless manner. The Government of Canada has alsobeen actively working to remove barriers that wouldotherwise prevent certified RTs from practising inother regions of the country. As of July 1, 2017, theCanadian Free Trade Agreement enables certified RTs“to work anywhere in Canada without having toundergo significant additional training, experience,examinations or assessment” (Labour Mobility, 2020).Introduction to the Health Workforce in Canada Respiratory TherapistsINTERNATIONALLY EDUCATEDRESPIRATORY THERAPISTSMost of the accredited schools in Canada takeindividual requests from internationally educatedrespiratory therapists (IERTs) or regulators to providethese applicants with credentials or prior learningassessment of the respiratory therapy educationprograms they have completed. This process is anattempt to determine how applicants’ educationcompares to the competencies required in Canada, aswell as what additional education they may require orhow they may be integrated into existing RT positionsor education programs (Blais, 2008). For example,Thompson Rivers University in British Columbiareports receiving several applications every year fromIERTs to enter its respiratory therapy program. Theuniversity assesses each applicant’s credentials,knowledge and skills to integrate them into theappropriate level of the program.This assessment and integration process is particularlyimportant because not every country recognizesrespiratory therapy as its own specialization orprofession. In fact, only a handful of countriesconsider the role of RTs as a full-time commitment.According to the Global Knowledge ExchangeNetwork (GKEN), respiratory care, in most countries,is provided by physiotherapists, nurses and physiciansthat have chosen to specialize this area (GKEN,2009). The choice of practitioners to specialize incardiopulmonary function and care results in “significant crossover in curriculum” that necessitates theassessment and integration process (GKEN, 2009).SCOPE OF PRACTICEFrom newborns to the elderly, any person can findthemselves in need of respiratory therapy, which iswhy RTs are trained to address all manners of acuteand chronic cardiopulmonary issues in a variety ofsettings. Table 3 highlights some examples of theconditions RTs treat, the common responsibilities ofRTs and the settings in which they often work.9
TABLE 3: Respiratory therapist scope, responsibilities and practice settingsConditions treatedResponsibilitiesPractice settings Asthma Critical care (including emergency,intensive care and trauma services) Hospitals Heart failure Chronic obstructivepulmonary disease Intubation and mechanical ventilation Anesthesia support Chronic bronchitis andemphysema Non-critical patient assessmentand treatments Underdeveloped lungs(in premature infants) In-home patient or client support Drowning Pneumonia Car accidents Respiratory distress Spinal cord injuredindividuals Croup Strokes Chest trauma(e.g., broken ribs) Head injuries Diagnostic testing services including:– Analysis of blood for oxygen and carbondioxide levels (arterial blood gas analysis)and various other blood values– Analysis of pulmonary function (volumesin/out of lungs, amount of oxygen andcarbon dioxide moving between the lungsand the blood, ability to quickly movevolumes in/out of lungs)– Analysis of the body’s responseto stress (exercise)– Cardiac electrical activity(electrocardiogram) Neonatal intensive care units Operating rooms Intensive care units General wards Coronary care units Emergency departments Continuing care facilities Community health clinics Pulmonary function laboratories Diagnostic clinics Sleep disorder laboratories Asthma, emphysema, cystic fibrosisand other specialized respiratory clinics Home care Teaching facilities Research units– Sleep studies (polysomnography) Patient transportation to hospitalor between hospitals Cardiopulmonary resuscitation (CPR) Rehabilitation units Hyperbaric oxygen treatment centres Medical equipment sales and service Control and supply of medical gases Patient/family/caregiver education Health promotionWithin any of the above areas, some of theprocedures an RT may perform include: Intubation (creating artificial airways byputting a tube through the mouth or noseinto the trachea) Suctioning (applying suction to keep thetrachea or lungs clear of mucous) Mechanical ventilation (life support systemmonitoring, and assessing and caring forpatients who need assistance with breathing) Medication delivery (using a mask andnebulizer or a “puffer”) Ensuring a warm environment fora newborn who is unable to maintaintheir own temperature.Source: HealthForce Ontario’s Health Human Resources Toolkit (2007)10Introduction to the Health Workforce in Canada Respiratory Therapists
REGULATION OF THE PROFESSIONIn 1981, Manitoba became the first province in Canadato form a regulatory authority for the RT profession(Blais, 2008). Since then, eight more provincialregulatory authorities have emerged in Alberta, BritishColumbia, Ontario, Nova Scotia, New Brunswick,Newfoundland and Labrador, Saskatchewan, andQuebec (National Alliance of Respiratory TherapyRegulatory Bodies [NARTRB], 2019). Table 4 lists theregulatory authority for each jurisdiction.TABLE 4: Respiratory therapy regulatory authorities for each jurisdiction in CanadaJurisdictionRegulatory AuthorityREGULATEDAlbertaCollege and Association of Respiratory Therapists of AlbertaSaskatchewanSaskatchewan College of Respiratory TherapistsManitobaManitoba Association of Registered Respiratory TherapistsOntarioCollege of Respiratory Therapists of OntarioQuebecOrdre professionnel des inhalothéraoeutes du QuébecNew BrunswickNew Brunswick Association of Respiratory TherapistsNova ScotiaNova Scotia College of Respiratory TherapistsNewfoundland and LabradorNewfoundland and Labrador College of Respiratory TherapistsNON-REGULATEDBritish ColumbiaPrince Edward IslandYukonCanadian Society of Respiratory Therapists (credentialling body)Northwest TerritoriesNunavutFor more information, visit nartrb.ca (regulated) or csrt.com (non-regulated).Provincial statutes delegated authority to the aboveentities to regulate the profession and protect thepublic. This authority includes setting registrationrequirements for the profession, setting and enforcingpractice standards and competency requirements,and undertaking disciplinary action if members fail tomaintain the RT standards of practice (Blais, 2008).The restricted professional title of RRT is protected byeach jurisdiction through its own regulatory authority.For example, Ontario protects the RRT title underSection 9 (“Restricted Titles”) of the RespiratoryTherapy Act (CRTO, 2020).Introduction to the Health Workforce in Canada Respiratory TherapistsTo ensure that the requirements to become anRRT are up to standard across the country, entitiessuch as the CSRT and NARTRB (an organizationthat brings together the nine regulatory authorities)work very closely with each other. Through collaboration and consultation, the CSRT and NARTRBare able to publish and update a well-informedNational Competency Framework for RTs inCanada. As a result, while there are some minorcontext-based differences from province to province,most requirements are extremely similar. Table 5highlights the basic requirements for provincialregistration as an RRT. (For more information onnational entry-to-practice requirements andrestricted titles, see Education and Training.)11
TABLE 5: Requirements for provincial registration as a registered respiratory therapistRequirementDetailsEducationMust have completed an approved respiratory therapy program, an equivalent or comparablerespiratory therapy program, or demonstrate competencies equivalent to those acquired insuch a program.ExaminationMust have completed an approved respiratory therapy licensure/registration examination.Eligibility for registrationMust be registered in good standing or eligible for registration as an RT in anotherCanadian jurisdiction or country.Language proficiencyMust provide evidence of fluency in English and/or French.CurrencyMust have graduated recently from an approved respiratory therapy program or workedas an RRT recently.Eligibility to work in CanadaMust have legal authorization to work in Canada.Good conduct/suitabilityto practiseMust provide evidence of good conduct and suitability to practise the profession.Source: NARTRB, Access issues regarding internationally educated health professionals and the respiratory therapy profession in Canada (2017)DEMOGRAPHICS OFRESPIRATORY THERAPISTSCIHI has published numerous reports showing anincreasing number of RTs in Canada since it first begancollecting data on the specialization in 1988 (CIHI,2020b). The data from the most recent reportingperiod (2014–2018, Figure 3) shows that the numberof practising RTs, on average, has been growing in everyprovince and territory in Canada, with the exceptionof a slight decrease in 2017–2018 in certain regions,most noticeably Quebec.CIHI’s most recent data report included a sectiondedicated to the number of healthcare workers per100,000 population, as this number is more meaningful than a basic “count” of RTs due to the varyingpopulations within each province and territory.Distribution is an extremely important factor inachieving balance in the health workforce. Table 7shows that the per-population ratio of RTs rosein each year of the reporting period.12Like much of the health workforce in Canada,respiratory therapy is predominantly female.Across Canada the proportion is 75% female froma low of 65% in Manitoba to a high of 84% inNew Brunswick and Quebec. This has changedlittle since 2018.REMUNERATIONMost RTs earn between 23.13 and 47.00 per hour,with the median wage at 34.95 per hour (Governmentof Canada, 2020). RT salaries are usually determinedby factors such as experience, education, credentials,employer and geographic location. For example, RTswho work at large hospitals in major cities are morelikely to earn higher wages than those who work atsmaller facilities in less populated areas. In addition toa salary, full-time RTs usually receive benefits such aspaid vacations, dental coverage, and contributions toinsurance and pension plans. More information on RTwages in each province and territory can be found inthe Respiratory Therapist in Canada section of theGovernment of Canada’s Job Bank website.Introduction to the Health Workforce in Canada Respiratory Therapists
Figure 3: Number of Respiratory Therapists by Province, B2,000SKAB1,500BCYK / NWT1,000500020142015201620172018Sources: Health Workforce Database, Canadian Institute for Health Information; Statistics Canada, Demography DivisionFigure 4: Respiratory Therapists, per 100,000 population by Province, 2014-201860NFLDPEI50NSNB40QCONMB30SKAB20BCYK / NWT10020142015201620172018Sources: Health Workforce Database, Canadian Institute for Health Information; Statistics Canada, Demography DivisionIntroduction to the Health Workforce in Canada Respiratory Therapists13
CURRENT ISSUES FORRESPIRATORY THERAPISTSA SHORTAGE OF RESPIRATORY THERAPISTSRespiratory disease is one of the primary causes ofdeath in Canada (West, 2013). Even before theCOVID-19 pandemic there were RT shortages in someparts of the country, and the Government of Canadawas already predicting a nation-wide shortage from2019 to 2028 (Brohman, 2020; Government ofCanada, 2019). Because RTs are on the front line of theCOVID-19 response, as they often are in public healthemergencies, shortage concerns about both RTs andequipment have been heightened throughout 2020.FUNDING FOR NEW EQUIPMENTRespiratory care technology is constantly evolving,presenting additional challenges of providing patientswith access to the best possible treatment and, at theinstitutional level, securing funding to replace outdated equipment on a yearly basis. Extra training forRTs is also required to remain up to date with all thenew equipment and deliver the best patient care.THE CHALLENGES OF COMMUNITY CAREAlthough RTs mostly work in hospitals, many also workin a variety of other settings, such as patients and/orclients’ homes, physicians’ offices, schools, assistedliving facilities and other non-traditional sites (CRTO,2018). As the elderly population continues to grow,community becomes increasingly important. Treatingclients in these settings comes with its own set ofchallenges. In addition to upholding their regularstandards of practice, RTs must be: self-driven asthey set their own schedules, maintain professionalboundaries with their clients and others involved intheir care, have strong organizational skills, and beflexible enough to “employ a holistic approach thatallows for the tailoring of services to meet the clientsand their families’ unique personal situations, needsand goals.” (CRTO, 2018).14CONCLUSIONRTs play an integral role in the Canadian healthcaresystem, using their specialized knowledge of cardiopulmonary functions to support Canadians of all ages,in a large variety of settings. They work collaborativelywith many different healthcare professionals toaddress a wide range of cases. In recent years, theirprevalence and integration in the Canadian healthworkforce has been growing, reflecting the importanceof their services to changing population demographicsand health needs.ACRONYMSCBRCCanadian Board for Respiratory CareCIHICanadian Institute forHealth InformationCMACanadian Medical AssociationCoARTECouncil on Accreditation forR
nentially in the wake of multiple respiratory-related disease outbreaks (West, 2013). One such crisis was the polio epidemic in Canada. By 1953, during the most devastating wave of the epidemic, there was an unprecedented increase in respiratory paralysis, making it a critical time for respiratory therapy. By 1960,