Transcription
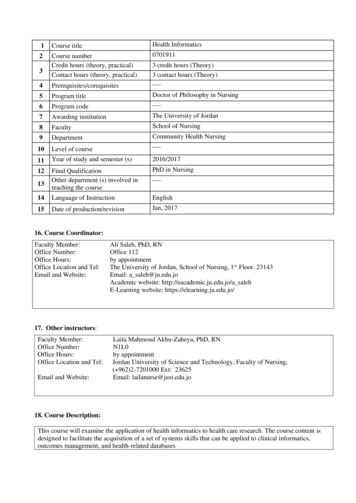
InformaticsChallenges with Health Information Technology in Nursing1.1 Introduction to Health Informatics and NursingNotes:Published by Articulate Storylinewww.articulate.com
1.2 IntroductionNotes:Welcome to the module on challenges with health information technology in nursing. In theEmerging Trends and Technology in Healthcare module you learned about how mobile technologyand social media is being used in healthcare. You also learned about the use of emergingtechnologies such as RFID, nanotechnology, wireless, and gaming in healthcare. In this module youwill learn about some additional challenges with the use of Health Information Technologies.Specifically documentation in EHRs, the impact of standardized nursing terminology, and somepotential changes to nursing workflow and practice. Let’s begin with challenges related todocumentation in an Electronic Health Record.Published by Articulate Storylinewww.articulate.com
1.3 Note BloatNotes:In the Electronic Health Record module you learned that large amounts of data are being recordedand captured. This information can be used to feed reports and populate notes. This has created aphenomenon termed note bloat. Remember that note bloat is the addition of large amounts ofinformation making it difficult for a clinician to identify the most relevant and important information.Information can be automatically inserted into a note. In some cases, the inclusion of this informationis due to billing or compliance needs. However this can make it more difficult for a clinician todecipher what information is relevant or new. This decreases efficiency and can cause relevant clinicalinformation to be missed. For example, links can be inserted into a note that will automatically pull inlarge amount of laboratory data. Critical changes in lab results could be lost within the large amountof less relevant or irrelevant data in the note if not specifically highlighted by the author.Published by Articulate Storylinewww.articulate.com
1.4 RedundancyNotes:The challenge of note bloat highlights another issue with EHR documentation which is redundancy. Agoal of an EHR is to reduce or eliminate the need for repeat documentation, and to have all therelevant information documented once and available for viewing. However, in the current healthcareculture this is often not the case. Many healthcare institutions and insurance companies require thatcertain elements be present in a note. These elements are already present in other parts of the system.This information is being aggregated for billing or compliance purposes, not necessarily for clinicalpurposes. The redundant use of this information contributes to note bloat and inefficiency.Information can be aggregated and displayed in more effective ways such as through dashboards.The use and displaying of data will be covered in another module.Published by Articulate Storylinewww.articulate.com
1.5 Entry ErrorsNotes:In addition to note bloat, the information that is entered into an EHR can be inaccurate. Inaccuraciescan occur from entry errors.Unless information is directly fed into a healthcare information system, such as through a direct feedfrom a patient monitor, there is still the need for humans to enter data. Even with direct feeds, dataverification and editing is necessary. The human factor introduces errors which can have a profoundimpact on patient care. Errors can result from:„Transcription errors - such as entering in a verbal order incorrectly„Not updating/removing old or expired information - such as medications that a patient is nolonger taking from the active medication list„Entering information on the wrong patient or at the wrong time - such as documenting anursing assessment on the wrong patientPublished by Articulate Storylinewww.articulate.com
1.6 Entry ErrorsNotes:Earlier in the year, Jack was misdiagnosed with Asthma which was entered into an Electronic HealthRecord. Jack is now to receive the flu vaccine and his mother requests that he receive the flu mist. Thedoctor review's Jack's Health Records and advises that Jack should not receive the flu mist because of apre-existing condition. The misdiagnosis of Asthma was never removed from Jack’s record and is nowthe basis for the doctor's decision. This is an example of how entry errors can influence patient care.Entry errors, such as inaccurate diagnoses, have the potential to influence Decision Support Systems,and will also be copied to patients’ Personnel Health Records.Inaccurate information within an EHR can lead to patient safety concerns, reporting errors, andcompliance errors. The erroneous information could be acted upon by other clinicians not realizingthat the information may be inaccurate. This could lead to potential patient safety risks. As the use ofanalytics increases with increased use of EHRs, outliers or false information contained within reportscould present a very different picture than what was intended. These reports are used by clinicians,administrators, and compliance officers - thus potentially leading to wrong actions at many differentlevels within a clinical organization.Published by Articulate Storylinewww.articulate.com
1.7 Copy ForwardNotes:Along with data entry errors, copying information forward through notes also may lead to inaccurateinformation in a patient’s medical record. Most EHRs have a feature that allows a clinician to copy aprevious note or flowsheet forward to save on time. However, some of the information containedwithin these notes or flowsheets may no longer be completely accurate at the time of the copy. Herewe have a nurse, a clinician and an administrator who all have experience with errors generated fromcopying forward. Click on each individual to hear his or her story."I made an error on Mrs. Johnson's record. It was the end of my shift and I was completing my shiftassessment. I quickly reviewed the assessment from the previous shift and nothing seemed to havechanged. However, I overlooked the fact that in the previous assessment it stated that Mrs. Johnson'sabdomen was NOT distended. Had I taken the time to read the assessment more carefully I wouldhave indicated that her abdomen was now distended. ""In updating Mr. Allen's record, I copied a note which was created earlier in the admission process.Unfortunately it contained a differential diagnosis which had already been ruled out. My error wasperpetuated as it continued to be copied over by the next clinician. ""When entry errors are brought to my attention, I have been asked why is it that we administratorscontinue to allow the use of these tools. In response, I emphasize that when clinicians are trainedproperly and the tools are utilized correctly, these tools significantly improve efficiency. They do thisby shifting the time spent on documentation to time spent with the patient."Published by Articulate Storylinewww.articulate.com
1.8 Lack of Standardized TerminologyNotes:With the emergence of health information technology and interoperability, the need forstandardization has increased. Nursing has traditionally described or documented nursing care interms that are not always clear to other health team members or standardized. Standardization ofnursing terminology is part of a broader topic within nursing, however, there are specific implicationsconcerning Health Information Technology.A standardized nursing language would be a “common language, readily understood by all nurses, todescribe care” (Keenan, 1999, p.12). Without such a standard language some critical elements toimprove nursing cannot be performed, such as comparisons. The comparison of data within andacross institutions is needed to establish best practices, evaluate and generate new nursinginterventions, and perform quality assurance.However, without a common language these actions cannot be performed. Comparisons betweeninstitutions cannot be made easily. For example, in reference to sputum production, small, moderate,and large are used as descriptors for volume. But how much is small, moderate, and large in terms ofvolume? Without precise definitions, there is inconsistency, which reduces the quality of comparisonsmade using this information. The National Quality Forum, a nonprofit organization committed tohealthcare improvement, has stated that “given the importance of nursing care, the absence ofstandardized nursing care performance measures is a major void in healthcare quality assurance andwork system performance"(NQF, May 2003, p. 1). Health Information Technology is enablinginstitutions, states, and nations to share, aggregate, and analyze large amounts of data. Without theconsistency of a standardized nursing language, it becomes more difficult to quantify nursing’scontribution to outcomes.Published by Articulate Storylinewww.articulate.com
1.9 Benefits of StandardizationNotes:The use of standardized nursing terminology will become a necessity in the increasingly technologicalnursing world. The use of standardized terminology will allow for many benefits including:„Consistent use of terminology across clinical settings and specialties„Communication between health information systems can more easily be achieved„Reporting and evaluation of data„Assess nursing competencyStandardization of nursing documentation will be critical to realizing the goal of interoperability. Theability of sharing comparable data across healthcare organizations will enable comparisons forbenchmarking, research, quality improvement, quality assurance, and patient safety. Performingthese comparison will be essential to improving patient outcomes and patient care.For more information on standardization of nursing terminology visit the International Classificationof Nursing Practice lished by Articulate Storylinewww.articulate.com
1.10 Impact of Health Information Technology on Nursing WorkflowNotes:Several different types of health information technology have been discussed so far, includingElectronic Health Care, Decision Support Systems, barcode scanning, mobile technology and socialmedia. The integration of these systems and technology into nursing practice can have a significantimpact on nurses and their workflow. Careful consideration of how nurses work, barriers nurses facein practice, and nursing values is needed to properly integrate health information technology.Unfortunately this is not always the case. The implementation of Health Information Technology canimpact nursing workflow and practice negatively by reducing productivity and increasing frustration.Published by Articulate Storylinewww.articulate.com
1.11 Reducing ProductivityNotes:Implementation of Health Information Technology without thoughtful consideration can decreaseproductivity. Many institutions see the Electronic Health Record as an opportunity to incorporateadditional documentation, such as additional assessments, risk screens, and discharge documentation.Compliance, regulatory, and quality improvement often are the motivators behind this increase indocumentation. The burden of this additional documentation often falls to the nurse. The additionaldocumentation requires additional time to complete. This can add a significant amount of time to thenurses workday and shift time away from spending with the patient. For example, a shift assessmentthat once took 2 minutes to complete on paper can take over 7 minutes in an EHR. The increaseddocumentation time can reduce productivity in terms of direct patient care and other nursing tasks.Published by Articulate Storylinewww.articulate.com
1.12 Increased FrustrationNotes:With this increased documentation comes increased frustration among nurses. The additionaldocumentation increases the nurses work load, contributing to feelings of frustration. Workaroundsand other unsafe practices may develop to increase efficiency as a result of this frustration. Forexample, a nurse may simply copy a previous assessment without reviewing its content in order toreduce the time spent on documentation. This could lead to an inaccurate assessment of a patient,which could have a much broader impact than realized.Published by Articulate Storylinewww.articulate.com
1.13 Potential Change to Nursing Workflow or PracticeNotes:The concerns that have been outlined in the module have caused some institutions and healthcaresystems to examine their practices concerning the use of healthcare information technology in orderto address these emerging issues. These potential changes can have an impact on nursing practice.One change that is being considered is the APSO note, where APSO refers to Assessment, Plan,Subjective and Objective. Current practice in both nursing and medical education is to teach studentsto construct progress notes using the SOAP (Subjective, Objective, Assessment, and Plan) format. Inthis format, the Subjective and Objective sections often contain information from other parts of thechart, such as vitals, medications, imaging results, diagnoses, etc., and are also pulled into the note forbilling and regulatory compliance. Bloated notes are generated from additional information beingadded to these two sections. However, clinicians find the Assessment and Plan sections to be the mostclinically relevant. Clinicians therefore have to scroll through a large amount of information to reachthe assessment and plan. To address this issue, some institutions and practices have changed the SOAPformat to an APSO format. Utilizing this format would place those sections that may be of more valueto clinicians, Assessment and Plan, at the beginning of the note saving them from scrolling to reachthe important information. A recent provider satisfaction evaluation in 13 practices was completed onthe use of the APSO format. 73% of the providers were either satisfied or very satisfied with using theAPSO format and 82% of providers were satisfied or very satisfied with reading APSO formatted notes(Lin, McKenzi, Pell, & Caplan, 2013).Published by Articulate Storylinewww.articulate.com
1.14 Knowledge Check1.15 The implementation of Health Information Technology cannegatively impact nursing workflow and practice by reducing productivity.Which of the following activities result in a reduction in productivity?(Select the best answer.)Feedback when correct:That's right!Feedback when incorrect:You did not select the correct response.Published by Articulate Storylinewww.articulate.com
Correct Response: Entering additional documentation required by compliance.Notes:1.16 Which of the following are benefits of standardization? (Select allthat apply)Feedback when correct:That's right!Feedback when incorrect:You did not select the correct response.The benefits are:i) Consistent use of terminology across clinical settings and specialties.ii)Communication between health information systems.Published by Articulate Storylinewww.articulate.com
1.17 SummaryNotes:In Summary: Issues with documentation in an Electronic Health Record include note bloat, redundancy, entryerrors, and copying forward The lack of a standardized nursing terminology is a problem due to inconsistency in comparison ofnursing interventions, processes, and contributions A standardized nursing terminology would enable cross institutional comparisons, communicationbetween health information systems, reporting and evaluation of data, and assessing nursingcompetencies Implementation of Health Information Technology can impact nursing workflow negatively throughdecreased productivity and increased nursing frustration Potential changes to nursing practice as a result of emerging Health Information Technologyincludes the APSO note formatPublished by Articulate Storylinewww.articulate.com
1.18 Curriculum Integration1.19 Curriculum IntegrationNotes:The issues that the use of Health Information Technology generate can be integrated into curriculum:„Discuss how progress notes can written in the APSO format instead of the SOAP format andthe pros and cons of using this format„Discuss how the issues presented in the module could lead to further practice changes, such asrequired note elements for providers or staff nursing documentationPublished by Articulate Storylinewww.articulate.com
1.20 References1.21 End of PresentationNotes:Published by Articulate Storylinewww.articulate.com
The use of standardized nursing terminology will become a necessity in the increasingly technological nursing world. The use of standardized terminology will allow for many benefits including: „ Consistent use of terminology across clinical settings and specialties „ Communication between health information systems can more easily be achieved