Transcription
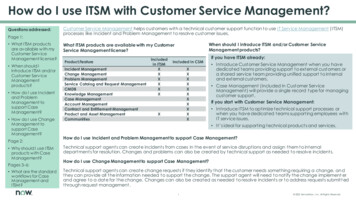
Case StudyImproving Customer Service at Health Share of OregonIntroductionThere are many ways to evaluate the delivery ofcustomer service in a health plan. Chief amongthese strategies is the assessment of enrollees’experiences with customer service staff. TheAgency for Healthcare Research and Quality’sCAHPS Health Plan Survey offers health plans astandardized way to assess whether they aredelivering the information and support thatmembers need and interacting with themappropriately. By analyzing the survey results,comparing scores to relevant comparators, andcollecting related information, health planmanagers can identify their strengths as well asareas in need of improvement. The challenge isfiguring out what changes to make to improveservice to members.This case study discusses the strategiesimplemented by Health Share of Oregon, acoordinated care organization (CCO) servingMedicaid recipients, to ensure that its customerservice staff understand and meet the needs ofits members. Health Share of Oregon wasselected for this case study because of its highscores on the “Health Plan Customer Service”composite measure in the CAHPS Health PlanSurvey as well as its improvement in one of thetwo survey items. (Survey questions are listed inthe box below.)The CAHPS Health Plan Survey’scomposite measure for Health PlanCustomer Service combines the resultsof two survey questions: In the last six months, how often did yourhealth plan’s customer service staff treatyou with courtesy and respect? In the last six months, how often did yourhealth plan’s customer service give youthe information or help that you needed?Looking at changes in CAHPS Health Plan Surveyscores from 2013 to 2014, Health Share saw amodest improvement in its already strongperformance on the survey question abouttreating members with courtesy and respect,from 92 to 94 percent. What was more strikingwas the 24 percentage point jump inperformance on the second question aboutgetting needed help and information fromcustomer service.Health Share’s 2013 and 2014 Scores onGetting Needed Help and Information FromCustomer ServiceInformation or Help Needed?88%100%80%60%64%40%20%0%20132014Challenges Facing Health Share andits MembersThe strategies that Health Share implementedto improve customer service were prompted bymultiple challenges in the local environment.First, the new coordinated care model inOregon was proving to be promising butcomplex (see box on the next page); itcombined several new systems that wereunfamiliar to both members as well as theparticipating health plans and providersassociated with those plans. This complexitywas compounded by the expansion of Medicaidin 2014 under the Affordable Care Act (whichposed its own issues, including a substantialadministrative backlog and long wait times for1
Improving Customer Service at Health Share of Oregonindividuals seeking coverage through theOregon Health Authority) and an influx of highneed members who had not been insuredbefore—all of which underscored theinsufficiency of the answers and informationavailable to members. Finally, as a coordinatedcare organization, Health Share was also dealingwith changes to benefits and new benefits,including new vendors for services such asmedical transportation and dental care. HealthShare recognized that it needed to take steps toreduce the complexity for members duringwhat had become a chaotic time.What Health Share Did to ImproveCustomer ServiceHealth Share attributes its performance on theCAHPS measure of patient experience withcustomer service to a combination of thefollowing strategies: Bringing customer service in-houseHiring to support a culture of serviceMeeting the needs of the whole person Training and coaching on an ongoing basisSetting standards and measuringperformanceDiffusing a member and service-orientedapproach throughout the organizationThese strategies are consistent with tworecommendations presented in the CAHPSAmbulatory Care Improvement Guide in thecontext of setting standards for customerservice.1 Develop an understanding of high-qualityservice from the perspective of membersand patients.Establish service standards so that staff areclear on what is expected of them and howthey should be interacting with membersand patients.1Standards for Customer Service, CAHPS AmbulatoryCare Improvement ealth Share of Oregon, a Coordinated Care OrganizationCreated in 2012, Health Share is one of 16 coordinated care organizations (CCOs) in Oregon. TheseCCOs represent a new model for integrated, coordinated care that is unique to the State’s Medicaidprogram. Each CCO is responsible for coordinating the efforts of health plans and providers to addressthe physical, mental, and dental health needs of the Medicaid population in a defined geographicregion. They are also expected to improve their members’ health by collaborating with organizationssuch as early learning hubs, housing groups, public health departments, and groups working withmarginalized populations.With 240,000 enrollees in the Portland tri-county region, Health Share is the largest coordinated careorganization in Oregon. While Health Share does not function as a health plan, it has many of thesame responsibilities vis-à-vis communicating with members to ensure they understand their benefitsand can get the services they need.Read about Health Share of Oregon at http://www.healthshareoregon.org/.Read about the coordinated care model in Oregon at /ccos.aspx.2
Improving Customer Service at Health Share of OregonBringing customer service in-houseFor its first year and a half, Health Share’scustomer service was handled by an externalvendor that was knowledgeable about theneeds of Medicaid members and the localhealth care system. However, Health Sharefound that having a vendor in this roledistanced the CCO from its members and madeit difficult to understand the members’ needs.They concluded that the organization and itsmembers would benefit from a tighterrelationship between the managerial hub of theorganization and the staff who were dealingwith members daily. In July 2014, they broughtthis function in-house by hiring a team of 10individuals who were trained on the specificcircumstances and challenges of Health Share’smembership.Hiring to create a culture of serviceFrom the beginning, Health Share wascommitted to hiring a professional staff thatwould strive to understand what good servicemeans to members and contribute to a serviceoriented team culture. In addition to identifyingstaff with some background or experience inthe medical or dental field, the manager of thecustomer service team was committed tofinding people with the ability to empathize andconnect with members and a passion forserving the community. The manager notedthat several people on the team have personalexperience as enrollees in the Oregon HealthPlan or the Medicaid program in another State,which gives them insight and sensitivity tomembers’ needs and the environment in whichthey are seeking care.An Interview Question to Assess theFit to the CultureDuring interviews, the customer servicemanager asks candidates a key question:“Tell us about an unsuccessful phone call.In retrospect, how would you do itdifferently?” By asking this question, themanager is looking for the ability toidentify the experience of an unsuccessfulphone call, understand the causes,acknowledge faults and challenges, andthink critically about how to do better.She is explicitly seeking people whoexhibit the capacity for growth as theylearn about Health Share, thecomplexities of the local health caresystem, and the needs of its members.Meeting the full spectrum of members’needsA health plan’s customer service staff are on thefront line with regards to helping membersunderstand and navigate through thecomplexity and jargon of the health caresystem. Health Share also recognizes that whilea member may call with one need that is clearlyexplained, they often have additional needs andquestions that are not expressed, such as howto access a specialist or enroll family members,children, or partners. Staff are trained toanticipate this situation by always askingmembers about other questions or concernsthey may have. They also try to help membersfeel comfortable by personalizing theconversation—for example, by confirming themember’s name and using it during the call.3
Improving Customer Service at Health Share of Oregon“Is there anything else I can helpyou with?”Another key aspect of Health Share’s serviceoriented philosophy is that they empowercustomer service representatives (CSRs) to givethe member time to speak and to solve themember’s problem in the moment. The CSRshave ready access to a library of resources theycan use to find the answers to questions.Perhaps more importantly, the CSRs can makechanges on the member’s behalf rather thanwork through the bureaucracy of getting inputfrom a supervisor. The CSRs are expected tobring their manager proposed solutions ratherthan problems. This culture is also reflected inHealth Share’s expectations regardingmembers’ voicemails, which are returned dailyand take priority over paperwork.Sometimes members call with questions orneeds that Health Share cannot address. Inthose cases, the staff have to transfer themembers to another system—such as themember’s health plan or the State agency thatmanages Medicaid enrollment. Beforetransferring the call, the Health Share CSRscoach members on the questions they shouldask about the problem they have presented,which helps to overcome some of the barriersthey might experience.Finally, Health Share’s staff includes a membernavigator, who deals with complex calls thatrequire a greater understanding of new benefitsor a higher level of intervention with providers,health plans, or the State agency. This person isavailable as a resource to all of the CSRs tohandle exceptional needs and carecoordination. Over time, the person serving asthe member navigator has also played a role inproviding ground-level supervision in the callcenter, helping to inform and train staff, andsupporting the education of new members,many of whom have never had insurancebefore.Training and coaching on an ongoingbasisThe initial training of the original customerservice team emphasized classroom instructionon communication skills, how to use thecustomer service software, and how to workwith interpreters. Medical and dental careproviders discussed how to explain members’benefits, and members of the executive teamshared information about the Medicaidpopulation. New hires are trained “at theelbow” so that they can learn from theircolleagues. However, all CSRs come togetherevery 2 weeks for updates and continuedtraining, with additional meetings arranged asneeded to explain new or changed benefits andtheir impact on members.One of Health Share’s strategic goals from theoutset, driven in part by input from itscommunity advisory council, was to betterunderstand and meet the diverse linguistic andspecial health care needs of the Medicaidpopulation in the Portland area. As part of thateffort, Health Share has invested a number ofresources and a fair amount of time in trainingCSRs to understand, anticipate, andappropriately respond to culturalconsiderations that can arise when they areinteracting with members. The goal is todevelop an understanding of the sum total ofexperiences that members carry with them intointeractions with their health plans, providers,and customer service.4
Improving Customer Service at Health Share of OregonHealth Share recognizes this focus on equity isnew for most people and that it will take timeto build awareness of the issues and bringabout a shift in the culture. To that end, theyhave developed a series of trainings on culturalcompetence and health equity. Each quarter,they focus on a specific issue, with one 2-hour,mandatory “lunch-and-learn” meeting for allstaff in 1 month and optional trainings thatsupport that topic in the other 2 months. Issuescovered in these meetings have included racism(specifically, how disparities affect health),disabilities due to mental health, traumainformed care and adverse childhoodexperiences, poverty and classism, and powerand implicit bias. The CSRs typically attend boththe mandatory and optional trainings to betterunderstand not just the issues that membersface but also what changes they can make tobenefit the members—from the tone of theirvoices to the extra effort to make theirexperience on the phone as positive as it canbe.Diversity Training OffersAdditional BenefitsIn addition to helping the CSRs betterunderstand the Health Share members,this training—and the investment itrepresents—is perceived as demonstratingthe company’s appreciation for the frontline role of the CSR. Moreover, because thediversity of the members is reflected in theCSRs themselves, some see the training asvalidating their experiences at a person,family, or community level and offeringthem the opportunity to contribute in ameaningful way.Setting standards and measuringperformanceHealth Share prides itself on the high standardsit has set for interactions with members. Onekey example is “one-call resolution:” they aimto resolve the member’s question or problemsatisfactorily without having to get off the line,even if they have to transfer the person to aprovider or heath plan. As of Spring 2016,Health Share had an 83-percent one-callresolution rate.Health Share also sets service-oriented targetfor CSRs; for example, they aim for— 80 percent of calls to be answered withinthe first 30 seconds.An abandonment rate of less than 3 percent(defined as the members who call andneither leave a voicemail nor have theircalls picked up).Warm transfers for all of their transfers.The manager of customer service tracks boththe quality and quantity of interactions withmembers. In addition to coaching the CSRs tobecome more efficient, the manager auditsabout 20 calls each month to ensure that thestaff are answering calls appropriately,documenting the conversation accurately, andconfirming that the members’ needs have beenmet. In the interest of visibility and teamcohesion, the manager also reviews theseperformance measures with staff andcelebrates successes (such as exceeding goals)monthly. The performance measures and dataare also shared with the executive team atHealth Share quarterly.Finally, the customer service staff and managerwork together to catalog what they are hearingfrom members and analyze trends so that theycan identify issues (e.g., confusion aroundbenefits) that need to be resolved more broadly5
Improving Customer Service at Health Share of Oregonand/or shared with Health Share’s executivemanagement. Health Share has benefited fromthe ability to collect qualitative data on thefront end and then pull it out at the back endand roll it into meaningful information.Diffusing a member and serviceoriented approach throughout theorganizationHealth Share makes a concerted effort toensure that the entire organization is aware ofmembers’ needs and the essential role playedby the customer service team in identifying andmeeting those needs. In addition to sharingperformance data with the executive team, thecustomer service team collects brief storieseach week that showcase complex cases wherecustomer service—in terms of information,navigation, and other support—was essential.These stories (edited to preserve members’privacy) highlight particular experiences thatmembers have had, some of the challengesthey have faced, and the ways in whichcustomer service was able to overcome thosebarriers. That message is shared throughout thecompany—to the CEO, quality assurancedepartment, information technology staff, andothers—so that they can connect to that onthe-ground experience.Another tactic that has helped to reinforce thecritical role of customer service throughout theorganization is the use of “ride-alongs” for newstaff. When they join Health Share, new staffspend about 90 minutes with customer service,listening to calls in order to gain a deeperunderstanding of members’ challenges.Health Share’s approach to customer servicecould be applied to other settings. Enrollees’experiences with customer service can beenhanced when staff are encouraged to seemembers as multidimensional people, not justspecific questions; empowered to seethemselves as problem solvers; and valued fortheir critical role in the organization.Questions? Contact the free CAHPS Help Lineat 1-800-492-9261 or cahps1@westat.com.AcknowledgmentsThis case study expands on a presentation givenby Graham Bouldin, M.S.W., the manager ofData Analytics & Quality Improvement at HealthShare of Oregon, during an April 2016 Webcasthosted by the Agency for Healthcare Researchand Quality. This Webcast highlighted theCAHPS Ambulatory Improvement Guide and thestrategies that health plans can use to improvetheir enrollees’ experiences. The CAHPS teamwould like to thank Mr. Bouldin and hiscolleagues—Deborah Friedman, ChiefOperating Officer; Florence Hurita, CustomerService Manager; and Michael Anderson-Nathe,Chief Equity and Engagement Officer—forsharing their experiences and achievements atHealth Share.Learn more about the Webcast webinar-041316.html.Read the CAHPS Ambulatory ImprovementGuide at vementguide/improvement-guide.html.ConclusionWhile most health plans do not have theopportunity to completely rebuild theircustomer service team, the values that shapedAHRQ Pub. No. 16-CAHPS003-EFSeptember 2016www.ahrq.gov6
customer service. Health Share's 20. 13 . and 201. 4 . Scores on Getting Needed Help and Informatio. n . From Customer Service. 64% 88% . 0% 20% 40% 60% 80% 100% 2013 2014. Information or Help Needed? Challenges Facing Health Share and its Members . The strategies that Health Share implemented to improve customer service were prompted by