Transcription
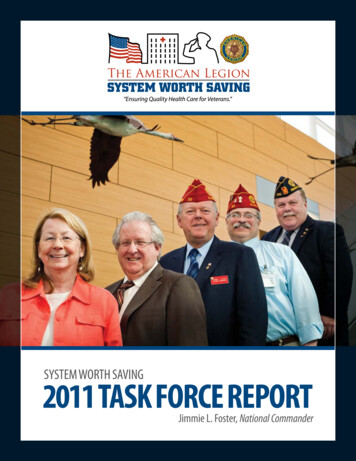
SyStem Worth Saving2011 Task Force reporTJimmie L. Foster, National Commander
Dear Fellow Legionnaires:In 2003, one of my predecessors as National Commander, and friend, Ron Conley, made it his priority toensure that veterans received the quality healthcare care they earned through service to our country, andfound that the Department of Veterans Affairs (VA) was indeed a “System Worth Saving.” Since 2003, TheAmerican Legion’s System Worth Saving Task Force has conducted site visits to VA Medical Centers to assess the quality and timeliness of VA healthcare, after which they reported to the President, Congress, SeniorVA Officials and American Legion members on the status of veterans’ healthcare.This year, the task force visited 46 VA Medical Centers, focusing on three critical areas affecting veterans’health care; the transition from Department of Defense (DoD) into VA Polytrauma System of Care, Traumatic Brain Injury (TBI) and Post Traumatic Stress Disorder (PTSD).In our findings, we discovered that service members still continue to navigate through a maze of differentDoD and VA benefit programs when they are transitioning out of service; they are not given a transitionchecklist or map to help guide them. The System Worth Saving Task Force and VA officials worked togetheron a transition flowchart, provided in this guide, to help explain the process to service members and informthem of the benefits to which they are entitled. In addition, the System Worth Saving Task Force discussedwith VA facilities about their TBI and PTSD programs, as well as research, screening, diagnosis, and currentchallenges and improvements needed in these areas.Many of the facilities visited this year were grateful to The American Legion for our lobbying efforts withCongress on passing Advance Appropriations, which provides VA with sufficient, timely and predictablefunding, a full fiscal year in advance. During the proposed government shutdown, facilities were confidentthat their budgets and staff would not be affected, and that The American Legion will continue to advocatefor improvements within the VA Healthcare System.I encourage you to review our findings and recommendations of the 46 VA Medical Centers visited thisyear. We hope that the information and data provided in the following reports will help Congress and VAunderstand what challenges our nation’s returning service members face with present transition, TBI andPTSD programs.The System Worth Saving Task Force’s goal has been to assist the VA in helping veterans and be an advocatefor improvement, while collaborating with senior VA officials or Congress whether it be a problem withfunding, staffing or program support. Our nation has an obligation to provide the best possible health careand treatment to the men and women upon their return home, after having gallantly served our country.Respectfully,Jimmie L. FosterNational CommanderThe American Legion
iiThe American Legion SyStem Worth Saving
sYsTeM WOrTH sAVING PrOGrAMTAsK fOrCe MeMBersMichael d. HelmChairmanVeterans Affairs andRehabilitation Commissionr. Michael suterVice ChairmanVeterans Affairs andRehabilitation Commissionronald f. ConleyPast National CommanderVeteran Affairs andRehabilitation CommissionPaul A. MorinPast National CommanderVeteran Affairs andRehabilitation CommissionTodd e. WhitePast National Vice CommanderVeterans Affairs andRehabilitation CommissionWilliam r. (Bob) WallaceVeteran Affairs andRehabilitation CommissionPhillip L. driskilVeteran Affairs andRehabilitation CommissionJohn W. HickeyVeteran Affairs andRehabilitation CommissionJeanette raeVeteran Affairs andRehabilitation CommissionThomas P. MullonVeteran Affairs andRehabilitation Commissiondon e. MathisVeteran Affairs andRehabilitation CommissionNATIONAL HeAdquArTers sTAffVerna L. JonesDirector, VA&R DivisionJacob B. GaddDeputy Director, Health Caredenise A. WilliamsAssistant Director,Health Policydenise L. BullockSenior Field ServiceRepresentativeJames M. Woodson, IVField Service RepresentativeBrian J. BertgesField Service RepresentativeWarren J. GoldsteinField Service RepresentativeFor additional information, please contact:Jacob Gadd, Deputy Director for Health CareVeteran Affairs and Rehabilitation Division202-263-2998jgadd@legion.orgThe American Legion SyStem Worth Saving1
TABLe Of CONTeNTsexecutive reportTransition of Care4Traumatic Brain Injury (TBI)15Post Traumatic Stress Disorder (PTSD)16Overlap and Differences between TBI and PTSD17VIsN 1VA Boston Healthcare System (Brockton/Jamaica Plain/West Roxbury, MA)19White River Junction VA Medical Center (White River Junction, VT)22VA Maine Healthcare System-Togus (Augusta, ME)25VIsN 2Syracuse VA Medical Center (Syracuse, NY)29VIsN 3VA New Jersey Healthcare System-East Orange Campus (East Orange, NJ)33James J. Peters VA Medical Center (Bronx, NY)35Northport VA Medical Center (Northport, NY)39VIsN 4Philadelphia VA Medical Center (Philadelphia, PA)43VA Pittsburgh Healthcare System (Pittsburgh, PA)46VIsN 5Martinsburg VA Medical Center (Martinsburg, WV)50VIsN 6Fayetteville VA Medical Center (Fayetteville, NC)55Asheville VA Medical Center (Asheville, NC)58Salem VA Medical Center (Salem, VA)61Hunter Holmes McGuire VA Medical Center (Richmond, VA)64VIsN 7Atlanta VA Medical Center (Decatur, GA)67Charlie Norwood VA Medical Center (Augusta, GA)69VIsN 8Bay Pines VA Healthcare System (Bay Pines, FL)73Orlando VA Medical Center (Orlando, FL)76James A. Haley Veterans’ Hospital (Tampa, FL)79VA Caribbean Healthcare System (San Juan, PR)82Malcolm Randall VA Medical Center (Gainesville, FL)85VIsN 92Lexington VA Medical Center (Lexington, KY)91Robley Rex VA Medical Center (Louisville, KY)94The American Legion SyStem Worth Saving
“Ensuring the Best Health Care for Veterans”VIsN 10Louis Stokes VA Medical Center (Cleveland, OH)Dayton VA Medical Center (Dayton, OH)98102VIsN 11Richard L. Roudebush VA Medical Center (Indianapolis, IN)106VIsN 12Edward Hines, Jr. VA Hospital (Hines, IL)110VIsN 15St. Louis VA Medical Center (St. Louis, MO)114VIsN 16Central Arkansas Veterans Healthcare System (Little Rock, AZ)118Michael E. DeBakey VA Medical Center (Houston, TX)121Oklahoma City VA Medical Center (Oklahoma City, OK)123VIsN 17South Texas Veterans Healthcare System (San Antonio, TX)128VA North Texas Healthcare System: Dallas VA Medical Center (Dallas, TX)130VIsN 18Phoenix VA Healthcare System (Phoenix, AZ)134Southern Arizona VA Healthcare System (Tucson, AZ)137VIsN 19VA Eastern Colorado Healthcare System (Denver, CO)141VA Salt Lake City Healthcare System (Salt Lake City, UT)144VIsN 20Alaska VA Healthcare System (Anchorage, AK)149VA Puget Sound Healthcare System-Seattle Division (Seattle, WA)153Portland VA Medical Center (Portland, OR)156VIsN 21VA Palo Alto Healthcare System (Palo Alto, CA)159San Francisco VA Medical Center (San Francisco, CA)161VIsN 22VA Greater Los Angeles Healthcare System (Los Angeles, CA)164VIsN 23Minneapolis VA Healthcare System (Minneapolis, MN)I AM NOT A NuMBer168170Testimonials171The American Legion SyStem Worth Saving3
The American LegionSyStem Worth SavingexeCuTIVe rePOrT a SyStem Worth Saving: 2011By Michael D. HelmChairmanThe American Legion Veterans Affairs & Rehabilitation CommissionIntroduction and BackgroundOver the past several years, the Department of Veterans Affairs’ Veterans Health Administration (VHA) has evolved interms of their delivery of resources to maximize the quality ofcare that is afforded to our nations’ veterans. Despite theseadvancements, the current conflicts in Iraq and Afghanistancontinues to create overwhelming challenges for the Department of Defense (DoD) and Department of Veterans Affairs(VA). Service Members are returning in unprecedentednumbers with Traumatic Brain Injury (TBI) and Post Traumatic Stress Disorder (PTSD) among other injuries such asburns, visual impairments, spinal cord injury and amputation. In addition to the numerous injuries and illnesses thatare plaguing our returning service members, they are facedwith the challenge of navigating their way through a transition process that is oftentimes fragmented and confusing.The American Legion has been instrumental in the establishment of the Department of Veterans Affairs, and an unrelenting supporter of veterans having access to the healthcarethat they have earned and rightfully deserve. VA is the largest integrated health care system in the country and has beenlauded as the organization that provides the best health care.In an effort to ensure that this is maintained, The AmericanLegion’s System Worth Saving program continues its missionof evaluating the VA healthcare facilities that are expectedto provide veterans with timely, quality and accessible care.The prevalence of the stated injuries and illnesses that ourservice members are sustaining has led the VA to establishthe Polytrauma System of Care. This system is speciallyequipped to provide veterans with comprehensive specialized rehabilitation and care led by a team of professionalsand consultants from all specialties related to their injuries. In addition, several programs and other systems wereimplemented or enhanced to assist service members andveterans as they transition through the DoD and VA fromrecovery through rehabilitation to community reintegration. Some of the programs and systems that were initiatedinclude the Federal Recovery Care Coordination Program,Integrated Disability Evaluation System, the VA LiaisonProgram, the Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), Operation New Dawn (OND)Care Management Program and VA’s Seven Touches of4Outreach program. Despite the creation of these services,there is a significant need for policies and practices to limitconfusion and provide clarity on how to fully utilize theseresources in a seamless manner.Other challenges noted during the System Worth Saving sitevisits in 2010 included: the limited budget for 2012, beneficiary travel program, decline in the numbers of Departmentof Veterans Affairs Voluntary Service (VAVS) volunteers andhours, hiring of specialty providers and the increase of compensation and pension (C&P) claims for Agent Orange. Aconsiderable number of VA Medical Center Directors havevoiced their concerns about their facilities ability to adequately fund certain programs. Several VA Medical Centers expressed that they are having serious issues with theBeneficiary Travel Program as some veterans have resortedto frivolous actions such as providing incorrect addresseswhich results in increased mileage, driving/riding togetherand making separate claims, taking no cost transportation,and making claims. This has resulted in a significant strainon the facilities budget. The Department of Veterans AffairsVoluntary Services (VAVS) Program reported that there hasbeen a decrease in the number of volunteers. This is due tothe rising gas prices and the current economical state of thecountry. The VAVS program also expressed that there needsto be a renewed initiative and effort to recruit younger volunteers in the program. With the growing number of veterans using VA as their primary medical provider, the facilitiescontinue to struggle with providing adequate parking spacesfor their patients. In addition, the Medical Center Directorsare faced with difficulties in filling certain positions due tothe competitive salaries being offered in the private sectorand a high turnover rate in certain specialty areas.In conclusion, as The American Legion embarks on its ninthpublication of the System Worth Saving report, we hope toconvey the message that the Department of Veterans Affairsis indeed a system worth saving. Included in this report aresections on Transition of Care, TBI, PTSD and Overlap ofTBI/PTSD as well as our site visit reports from 46 VA Medical Centers. The information gathered through these sitevisits can be utilized as a guide and a resource for those whoserve our veterans.The American Legion SyStem Worth Saving
“Ensuring the Best Health Care for Veterans”TrANsITION Of CAre Combat inJured veteran, Combat veteran and veteranSOne of the focuses of The American Legion’s System Worth Saving Program for 2010-2011 was Service Member’s Transition ofCare from the Department of Defense (DoD) into the Department of Veterans Affairs (VA). The American Legion definedthree types of transitioning service members in this report:Combat Injured Veteran, Combat Veteran and Veteran.Once a service member sustains an injury in theater, their treatment process is initiated there. This is where combat lifesavercare is performed by a combat medic or corpsman. The combat medic or corpsman gives the injured soldier a Military AcuteConcussion Evaluation (MACE). According to the Defense andVeterans Brain Injury Center (DVBIC), the MACE screeningtest was designed for the acute evaluation of concussion. Thismethod is currently the only standardized and most widely usedprocess for evaluation of acute mild TBI (otherwise known asconcussion) in military operational settings. The MACE can beadministered by any level of medical provider (medic/corpsmanto physician) when there is suspicion of concussion. This test isadministered within the first 48 to72 hours following injury.The service member is then transported by ground ambulanceor helicopter to the next level of care, such as 332d Air ForceTheater Hospital at Balad Air Base Iraq where life-saving treatment is provided. The service member is then transported byaeromedical evacuation flight to Ramstein, Germany, wherecare will continue at Landstuhl Regional Medical Center. Following their treatment at Landstuhl Regional Medical Center,the service member is transported to the states where they areadmitted to a Military Treatment Facility.Combat injured veterans are those wounded, ill and injuredservice members that were injured in Operation EnduringFreedom (OEF), Operation Iraqi Freedom (OIF) or OperationNew Dawn (OND) on the battlefield and were treated at a Military Treatment Facility. Combat veterans are service memberswho served in theater during Operation Enduring Freedom(OEF), Operation Iraqi Freedom (OIF) or Operation NewDawn (OND) who can receive cost-free medical care for anycondition related to their service in theater for five years afterthe date of their discharge or release. In order to take advantage of these benefits, OEF/OIF/OND veterans need to enrollin VA’s health care system. Veterans are those service memberswho did not deploy to a combat theater and go through theregular transition process from DoD to VA.CoMBat InjureD Veteran (See Chart A)Medical evaluation Board (MeB)The MEB is the initial phase of the IDES that is convened to determine a service member’s medical and duty status. A servicemember is referred to a MEB by a unit commander or a physician when it is believed that he or she may possess one or moremedical conditions that cause him or her to fail to meet retention standards. A service member does not “apply” or self-referhimself or herself for evaluation by a MEB.MEBs are generally located at a service member’s treating military treatment facility (MTF). An exception to this might be ifa service member is at another military installation for medicaltreatment. In that instance, the installation providing medicaltreatment might conduct the service member’s IDES processing, rather than at his or her home station. Currently, DoDdoes not have a central website to provide additional information about the MEB program.Physical evaluation Board (PeB)The PEB, which is an administrative board, determines if theproposed unfitting medical condition(s) renders the servicemember inability to continue further service based on his or hermilitary grade, rank, or rating. A PEB will determine whethera service member will be retained in the armed forces. Eachbranch of service has its own criteria governing fitness for duty.For example, the Navy might require deployability, whereas theArmy does not require deployability as factor for retention. Ifthe PEB determines unfitness for duty, it will assign a disabilityrating based on the severity of the injury.The PEB, with a number of exceptions, uses the Department ofVeterans Affairs Schedule for Ratings of Disabilities (VASRD) asa guideline to determine disability ratings for unfitting medicalconditions. There are two types of PEBs— the informal and theformal PEB. The PEB, whether formal or informal, is composedof three people—a Board president, a personnel managementofficer, and a physician. When a reservist is being evaluated, aboard member must be a member of the Reserve Component.Currently, DoD does not have a central website to provide additional information about the PEB program.The American Legion has three MEB/PEB representatives at Walter ReedArmy Medical Center (Washington, DC), Brooke Army Medical Center (San Antonio, TX) and Fort Lewis (Tacoma, WA).The American Legion SyStem Worth Saving5
The American LegionSyStem Worth SavingFor more information or if you have questions regarding theMEB/PEB process, please contact the National Security/ForeignRelations division at nsfr@legion.org.Integrated Disability evaluation System (IDeS)In November 2007, DOD and VA began piloting the IDES, a jointdisability evaluation system, to eliminate duplication in their separate systems and expedite receipt of VA benefits for wounded, ill,and injured service members. The pilot program for disabilitycases originated at the three major military treatment facilities inthe National Capital Region, (Walter Reed Army Medical Center, National Naval Medical Center Bethesda, and Malcolm Grow(Andrews) Air Force Medical Center). The IDES merges DODand VA evaluation processes, so that service members begin theirVA disability claim while they undergo their DOD disabilityevaluation, rather than sequentially, making it possible for themto receive VA disability benefits shortly after leaving military service. The IDES merges DOD and VA’s separate exam processesinto a single exam process that is conducted to VA standards. Italso consolidates DOD and VA’s separate rating phases into oneVA rating phase. In addition, the IDES provides VA case managers to perform outreach and nonclinical case management andexplain VA results and processes to service members.VA and DoD worked together to increase the number of sites forthe IDES program from 21 to 27 in 2010. The six new sites areFort Riley, Fort Benning, Fort Lewis, Fort Hood, Fort Bragg, andPortsmouth Naval Hospital. The IDES simplifies the process fordisabled Service members transitioning to veteran status, improvesthe consistency of disability ratings, and improves customer satisfaction. Currently, both DoD and VA do not have a central websiteto provide additional information about the IDES program.The American Legion has MEB/PEB Representatives at WalterReed Army Medical Center, Brooke Army Medical Center and FortLewis to assist transitioning service members with the MEB/PEBprocess. For more information, contact The American Legion National Security Foreign Relation Commission at nsfr@legion.org.Benefits Delivery at Discharge (BDD)The Benefits Delivery at Discharge (BDD) Program allows aservice member to apply for disability compensation benefitsfrom the Department of Veterans Affairs (VA) prior to retirement or separation from military service. BDD is offered toaccelerate receipt of VA disability benefits, with a goal of providing benefits within 55 days after release or discharge fromactive duty. BDD allows a service member with at least 60 days,but not more than 180 days, remaining on active duty to file aVA disability claim prior to separation. BDD requires a minimum of 60 days to allow sufficient time to complete the medi-6cal examination process (which may involve multiple specialtyclinics) prior to separation from service. To fully participatein the BDD Program, you must submit VA Form 21-526, alongwith a copy of your service treatment records (or original), andbe available to attend and complete all phases of the VA/DoDmedical separation examination prior to leaving the area.According to the American Legion’s national BDD staff, thereare several challenges that they encounter with this program.There is a significant need for additional resources, funding andstaff to meet the 55-day standard and maintain the timelinessof processing claims. The rating Regional Office (RO) has torely on the proper development of the BDD claim at the variousintake sites. If the intake site fails to properly develop the claimthe BDD rating RO has to complete the development, whichcould delay the rating. Another challenge is service membersleaving the area prior to all examinations being completed. Ifthey do, it requires the rating RO to reschedule the exams, delaying the final rating. The staff further noted that a better effort needs to be made to let the Reserve service members awareof the BDD program. Oftentimes the active duty members areable to utilize the services right away and the Reserve servicemembers have to wait and go through the long process.In terms of case completion, the BDD national staff reports thatbetween October 2009 and September 2010, the Salt Lake City,UT office completed 10,511 BDD claims and Winston/Salem,NC office completed 12,072 claims. Between October 2010and May 2011, the Salt Lake City, UT office has completed 6,671BDD claims and Winston/Salem has completed 6,919 claims.Salt Lake City has a current inventory of 4,056 BDD claimsand Winston/Salem has 5,869. In addition, the national staffexpressed the concern that the lack of an integrated medical record between DoD and VA have resulted in serious setbacks inthe claims process.For more information about the BDD program, please visit VA’swebsite at: ral/bdd brochure.pdf. To reach The American LegionBDD Representatives in the Winston Salem, NC and Salt LakeCity, UT office for assistance, please contact the VA&R divisionat var@legion.org.Va Liaison ProgramThe VA Liaison Program now has 33 liaisons serving at 18 military treatment facilities. The VA Liaisons are integrated withstaff at the Military Treatment Facility (MTF) sites to coordinatecare and provide onsite consultation about VA resources andtreatment options, and a majority of them are co-located withthe military’s own case managers. A standardized referral formthat outlines the patient’s medical needs is provided by the MTFThe American Legion SyStem Worth Saving
“Ensuring the Best Health Care for Veterans”case manager to the VA Liaison with attached medical records,so the service member can be registered into VA’s ComputerizedPatient Record System.The program helps injured Active Duty, National Guard orReserve Service members receive care that VA uniquely specializes in, and also aids service members who are separatingfrom the military in the transition process to VA. For less severely injured service members, VA also has Liaisons co-locatedwith Army Warrior Transition Units (WTUs), which supportwounded Soldiers requiring rehabilitative care at some MTFsites. The VA Liaison offers care where appropriate, or if servicemembers are transitioning out of the military, the Liaison willmake contact with their local hometown VA, enroll them, helpschedule appointments or inpatient beds, and have a contactnumber ready for when they leave the MTF. Each VA Liaison isbased out of the Veterans Affairs Medical Center (VAMC) thatis located nearest to each participating MTF, and the partnership is outlined in a local Memorandum of Agreement.VA Liaisons participate in video teleconferencing between MTFand VA staff, and coordinate referrals with the OEF/OIF/ONDProgram Manager at the receiving VAMC. Each VA Medical Center has an OEF/OIF/OND Care Management Team, inwhich a program manager serves as the contact point for referrals from the MTF and coordinates the transition of care, and acase manager provides further services to help manage the careof severely ill or injured patients.For more information on the VA Liaison program, please visitVA’s website at: http://www.oefoif.va.gov/valiaisons.asp.operation enduring Freedom/operation IraqiFreedom/operation new Dawn (oeF/oIF/onD) Care Management ProgramIn October 2007, the Department of Veterans Affairs (VA) established the OEF/OIF (Operation Enduring Freedom/Operation Iraqi Freedom) Care Management Program in the Officeof Patient Care Services located in VA Central Office. The program addresses the needs of wounded and ill service membersand veterans as they return from deployment and transitionfrom the DoD health care system to the VA system of care. In2010, VHA expanded the OEF/OIF program to include Operation New Dawn (OND) veterans. Under VHA’s OEF/OIF/OND Care Management Program, each VA Medical Center hasan OEF/OIF/OND Care Management team in place to coordinate patient care activities and ensure that service membersand veterans are receiving patient-centered, integrated care andbenefits. Severely injured OEF/OIF/OND veterans are provided with a case manager and any other OEF/OIF/OND veteranmay be assigned a case manager upon request or as indicated bya positive screening assessment. For more information, pleasevisit VA’s website: http://www.oefoif.va.gov/.Federal recovery Care Coordination ProgramThe Federal Recovery Care Coordination is a process that assesses, plans, implements, coordinates, monitors, and evaluatesthe benefits and services required to meet the client’s goals regardless of client location, health status and types of injuries orillness. The FRC program includes advocacy, communication,assets and information management. The program also promotes an integrated approach to effectively manage medical andsocial conditions for wounded, ill or injured service members,veterans, and their families across transitions.In order to be eligible for this program, the service member hasto be in an acute care setting within a military treatment facility; considered at risk for psychosocial complication or self orcommand referred based on perceived ability to benefit from arecovery plan. The service member may also if eligible if theyhave been diagnosed or referred with Spinal Cord Injury, Burns,Amputation, Visual Impairment, Traumatic Brain Injury (TBI)or Post Traumatic Stress Disorder (PTSD).An assigned Federal Recovery Coordinator will develop a Federal Individualized Recovery Plan with input from the multidisciplinary health care team, the service member or veteran, andtheir family or caregiver. They track the care, management andtransition of a recovering service member or veteran throughrecovery, rehabilitation and reintegration.For more information about the Federal Recovery Care Coordinator Program, please go to: a System of CareThe Polytrauma System of Care (PSC) is an extensive medicalsystem that provides medical rehabilitation, coordination ofsupport, and also information tool for active duty, veterans andtheir family members. This specialized treatment of rehabilitation consists of Traumatic Brain Injury (TBI) and Polytraumacase management. There are currently four lead PolytraumaRehabilitation Centers (PRC) located in Richmond, Virginia;Tampa, Florida; Minneapolis, Minneapolis and Palo Alto, California and a fifth being established in San Antonio, Texas. Thereare also twenty-two (22) Polytrauma Network Sites (PNS),eighty (80) Polytrauma Support Clinic Teams (PSCT) and fifty(50) Polytrauma Points of Contact (PPOC) located at VA Medical Centers across the U.S. providing a continuum of integratedcare for soldiers and veterans. The PRC’s receives referrals fromthe Medical Treatment facilities (MTF) Walter Reed, BethesdaNaval, Brooke Army Medical Center.The American Legion SyStem Worth Saving7
The American LegionSyStem Worth SavingReferrals from Military Treatment Facility Provided by: Senior Social Workers Nurse Case Manager PhysicianOutreach to the Veterans Affairs (VA) Facilities Provided by: Social Work Services (SWS) Nationwide sharing National teleconferences (education, dissemination, policesand new initiatives) Community Colleges, local Army Reserve, National GuardUnits Community Organizations Post Deployment Health Reassessment (PDHR’s) InactiveReady Reserve (IRR) Muster, Yellow RibbonMedical Records Shared through: DOD sends electronic filesVideo-teleconferencingDirect access from the SWSElectronic Bi-directional Health Information ExchangeOutreach to the Veterans/Families Provided by: Transition Patient Advocate (Liaison between veterans, theirfamilies and staff) OEF/OIF/OND ManagerCase Management/Seamless Transition to Veterans AffairsMedical Center (VAMC) Tracking of non-severely injured, severely injured throughthe Case Management Referral and Tracking Application(CMTRA) database Military liaison embedded to support active duty patients One case manager for individual veteran Phone conferences, video teleconferencing, direct telephone,scheduling appointments, assignment of case-manger Life Long case management as long as PMR needs continue(monthly, quarterly, semi-annually or annual basis Individualized follow-up plan for all veteransCoMBat Veteran (See Chart B)Military veterans, including Reservists and National Guard members, who served in combat theater after November 11, 1998, including veterans of Iraq and Afghanistan, are eligible to receive fiveyears of enhanced enrollment eligibility for VA health care services,which provides cost-free health care from VA for conditions thatare potentially related to their service in the theater of operations.VA has a number of programs, services and outreach for combatveterans including: Health Resource Center, Health EligibilityCenter and the Seven Touches of VA Outreach program.8the Health resource CenterIn 2002, VA established the Health Resource Center (HRC) as anational contact
Salem VA Medical Center (Salem, VA) 61 Hunter Holmes McGuire VA Medical Center (Richmond, VA) 64 VIsN 7 Atlanta VA Medical Center (Decatur, GA) 67 Charlie Norwood VA Medical Center (Augusta, GA) 69 VIsN 8 Bay Pines VA Healthcare System (Bay Pines, FL) 73 Orlando VA Medical Center (Orlando, FL) 76 James A. Haley Veterans' Hospital (Tampa, FL) 79