Transcription
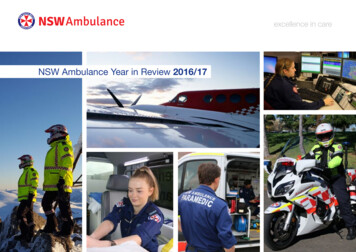
excellence in careNSW Ambulance Year in Review 2016/17
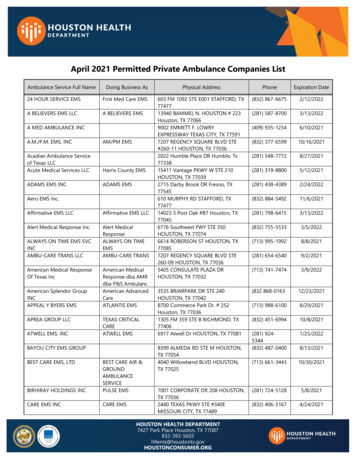
IntroductionEmergency Careinto the RAIR program fold, with threenew sites set to undergo completerefurbishment, upgrade or be replacedby a brand new facility.On a clinical front, integrated carecontinues to be a strong focus for ourorganisation with alternative treatmentand referral pathways forming a key partof an ongoing strategy.2016/2017 represented an extraordinaryperiod of change, progress, opportunityand challenge for NSW Ambulance asan organisation.NSW Ambulance has seen great resultsfrom staff, stakeholder and Unioncollaboration and hard work, whichhas helped us to set our focus throughopen and difficult conversations and theimplementation of initiatives designed tobetter support the workforce.The importance of the continuation ofthis work has been recognised by theNSW Government in 2017 with the NSWPremier Gladys Berejiklian and NSWHealth Minister Brad Hazzard pledgingan additional 48-million in funding formental health and wellbeing support toNSW Ambulance.This significant investment will ensurethat NSW Ambulance can continue toassist and support our staff from the firstto the last day of their NSW Ambulancecareer, with a comprehensive range ofNSW Ambulance Year in Review 2016/17integrated physical and mental healthand wellbeing strategies.Building the future for NSW Ambulancealso took great strides this year withthe Sydney Ambulance MetropolitanInfrastructure Strategy (SAMIS)program enabling the carefully plannedimplementation of the ParamedicResponse Network (PRN) to commence.The transition saw the delivery andopening of superstations at Bankstown,Kogarah, Blacktown and Liverpool withPenrith due to commence operations inlate 2017.Although this change is significant, it isalready clear that NSW Ambulance staffand our patients will greatly benefit fromthis new way of doing our everyday corebusiness – delivering timely, high qualityemergency care to patients.The 122 million Rural AmbulanceInfrastructure Reconfiguration (RAIR)has gone from strength to strengthin 2017, bringing even more stationsA key highlight for the organisation wasthe launch of the first Staff Wellbeingand Resilience Summit in July 2016,introducing a range of other services tosupport staff.These include the establishment ofWellness Wednesdays, the launch ofthe mental health literacy online andmindfulness program, establishmentof NSW Ambulance Supporting ourFamilies information sessions.This year, we haveset our focusthrough open anddifficult conversationsand the implementation ofinitiatives designed to bettersupport the workforce.”This year also saw the introduction ofincreased Chaplaincy support, FirstContact Coordinators introduced,a Buddy program established andimproved Recover at Work support.A key framework which was introducedto provide a robust support network forstaff was the Staff Support Activationand Significant Events Support Registerand Worker Injury Screening and EarlyIntervention (WISE) program, which issupported by an increase in our numberof Peer Support Officers.As part of NSW Ambulance’scommitment to providing enduringsupport for existing and retiredstaff, NSW Ambulance Legacy wasannounced, designed to promotewellbeing and support during retirementfor all NSW Ambulance staff.DELIVERING CARETHROUGHOUT THE STATENSW Ambulance has reached new heightsin 2016 and 2017 with the official launchof aeromedical bases and helicopterfleets throughout the state as part ofthe implementation phase of the NSWGovernment’s 151.2 million state-wideHelicopter Retrieval Network.The network was developed and informedby the Aeromedical Reform Plan, whichprovided a new operational model fordelivering high quality medical care to awider variety of patients from a greaterrange of areas, incorporating the latestin aeromedical technology to improveresponse times, patient treatment andsafety in transit.patient centredThe NSW Helicopter Retrieval Network isseparated into the southern and northernzones, with the southern zone consisting ofbases in Sydney-Bankstown, Wollongongand Orange which is serviced by the Toll &NSW Ambulance Rescue Helicopter fleet.The northern zone, includes bases atNewcastle (Belmont), Tamworth andLismore and commenced operations onMarch 7, 2017 marking the continuation ofthe collaborative delivery of aeromedicalservices by NSW Ambulance and theWestpac Rescue team from the Hunter tothe Queensland border.NSW Ambulance’s aeromedical staff onboard both the northern and southernzone aircraft, provide exemplary serviceto patients in all corners of the state,completing around 3000 patient missionsstate-wide each year.Following on the conversations andactions of the Staff Wellbeing andResilience Summit, NSW Ambulancebegan the planning and development ofthe 2017 Safety & Culture Summit.Due to be held in the second half of2017, The NSW Ambulance Safety& Culture Summit was built on theconversation started in 2016, focusingon providing a forum of discussionon workplace safety issues andempowering staff to make an immediatecommitment to changing and improvingour safety behaviours and culture.All in all 2016/17 has been a highlyproductive and progressive year, witheven more planned for the next twelvemonths ahead in order to position NSWAmbulance to be best placed to meetcurrent and future patient demand.Dominic Morgan ASMChief Executive2NSW Ambulance Year in Review 2016/173
Emergency Carepatient centredEmergency Carepatient centredNORTHERN ZONENSW Ambulance and the Westpac RescueHelicopter Service partnered in 2017to deliver rescue, retrieval and patienttreatment from a fleet of brand newAgusta Westland 139 (AW139) aircraft.For the first time in the history of theorganisations partnership, the NSWAmbulance roundel, logo and checkeredcandy stripe are now emblazoned on theiconic Westpac Rescue Helicopter.The NSW Ambulance and RescueHelicopter fleet have a NSW AmbulanceCritical Care Paramedic and a LocalHealth District (HNELHD) doctor on boardevery flight.The fleet is made up of four bigger,safer and more clinically capable AgustaWestland 139 (AW139) helicopters, whichwill assist NSW Ambulance to reachpatients even further away from NSWAmbulance bases, quicker than everbefore.SOUTHERN ZONEThese helicopters have the capability tofly to any area of the state from their homebase effectively, allowing the continuum ofcritical care from the scene to the hospital,with the aircraft virtually Intensive CareUnit (ICU) capable.To support the new fleet, new andrefurbished helicopter bases werecompleted and officially opened byCommissioner Morgan and local staffat Newcastle (Belmont), Lismore andTamworth.NSW Ambulance Year in Review 2016/17The southern zone contract for NSWAmbulance aeromedical services, operatedby Toll Group was officially launched onJanuary 10.a helicopter into a flying ICU deliveringcritical care to patients. The new, largerfleet is white, with the NSW Ambulanceroundel and Toll logo, not red and whiteas NSW Ambulance helicopters had beenpreviously.Under the new contract, a NSW Ambulancedoctor and critical care paramedic respondon every flight. Bases at Wollongong andOrange now operate 24/7 to deliver fasteremergency care to the regions.The southern zone’s Sydney-BankstownBase commenced operations in 2017 andall bases including Wollongong and Orangeare due to be officially opened in early2018.The Toll & NSW Ambulance RescueHelicopter fleet is made up of eight AgustaWestland 139 (AW139) helicopters.This partnership enables NSW Ambulance’shighly-qualified NSW Ambulance helicopterdoctors and paramedics to continue todeliver exceptional out-of-hospital criticalcare to patients across the state.The medical fit-out on board these aircraftis second to none; virtually transforming4NSW Ambulance Year in Review 2016/175
Emergency Carepatient centred50 YEARS OF EMERGENCYAIR CAREMarch 2017 represented a significantmilestone for NSW Ambulance, marking 50years since the first Beechcraft Queen AirB80 took flight, beginning the organisationsenduring legacy of providing criticalemergency medical care throughout thestate.The delivery of emergency medical careacross the entirety of NSW over the yearshas always presented a challenge for theorganisation due to expanse of the state.As far back as the 1920s, it was noted thatill and injured people in remote areas ofNSW were dying because of their isolationfrom medical care.NSW Ambulance Year in Review 2016/17On 29 March 1966, the Governmentapproved the purchase of an aircraft,a twin-engine, multi-berth aircraft, aBeechcraft Queen Air B80, to be operatedby East-West Airlines.Described as an “intensive care wardwith wings”, the US-built plane was fittedout with navigational aids to permit flyingat night, together with piped oxygen, amaternity kit, humidicrib, blood transfusionand tracheotomy gear, drugs, intravenoustherapy, burns and resuscitationequipment.It carried four stretcher cases and twoseated patients, while the operating crew,comprised of a pilot and flight nurse andthree nursing sisters, were engaged.The NSW AirAmbulance Servicehas developedsignificantly over the yearsto keep pace with the everchanging demands in bothaviation and patient care.”The NSW Air Ambulance Service hasdeveloped significantly over the years tokeep pace with the ever changing demandsin both aviation and patient care. Medicalequipment that was once only thought tobe accessed in a hospital now routinelycarried on flights Flies an average 7021hours a year Conducts more than2800 missions a year Transported 5200patients in 2016NSW Ambulance has a history ofdelivering a high standard of emergencymedical care and November 2016marked the 40th anniversary sinceIntensive Care Paramedics (ICP), orAdvanced Life Support Officers as theywere known, completed their first courseand were introduced to NSW Ambulance.39 flight nurses 25 pilots 13 engineer Six ground handlersNevertheless, the change in practice wasmassive and ICPs progressed from asystem of basically having no technologyand being limited to what they couldsee and do to suddenly having accessto sphygmomanometers, stethoscopes,defibrillators, morphine and adrenaline.Fast forward 40years and NSWAmbulance taughtits 79th ICP course inSeptember 2016.”The need for emergency serviceresponders with specialised skills in thedelivery of intensive medical care wasfirst identified in 1975 by the Director ofIntensive Care Services at St Vincent’sHospital.To date there arecurrently 442 ICPsoperating in theorganisation with theirskills constantly advancingand developing, benefitingmembers of the communityon a daily basis.”On Board: This came into effect on 1 January 1977and the newly minted ICPs were held offfrom utilising their skills unsuperviseduntil then.A legacy of care and skillToday the fleet providesspecialist critical carethroughout the state.Includes five aircraft three BeechcraftKingAir 200C and two350Cpatient centredIN A SNAPSHOT:Medical equipmentthat was onceonly thought to beaccessed in a hospital is nowroutinely carried on flights.” Emergency CareFollowing intense lobbying, support andcollaboration, the first Intensive CareParamedic course began and was initiallymet with nervousness by the medicalcommunity.6NSW Ambulance Year in Review 2016/17NSW Ambulance ICP’s were the firstnon-doctors in NSW to go into theatres,do intubations and cannulations. The firstICPs were launched in 1977 and regardedby many as ‘cowboys’ because they weredelivering care that only doctors could do.Graduating at a time of immense change,ICPs arrived when NSW Ambulance wasbeing transferred from the NSW AmbulanceTransport Service Board to the NSWGovernment under the Health Commission.The first ICPswere regarded ascowboys becausethey were delivering carethat only doctors coulddo, were the first nondoctors in NSW to go intotheatres, do intubations andcannulations.”Initially known as Advanced Life SupportOfficers, although the term “paramedic”was later adopted, this being morepublicly identifiable due to a UStelevision series, ‘Emergency’, which waspopular at the time.7
Emergency Carepatient centredMeeting DemandURGENCY OR EMERGENCY?In November 2016 NSW Ambulancelaunched the second phase of the “IsYour Urgency an Emergency?” a publiceducation campaign, building on themessaging delivered during the firstcampaign earlier in the year.In order for a case to be suitable for use as part of the trial itmust include the following factors: a patient aged between 12 – 70 years old patient must receive external cardiac compressionswithin 10 minutesNSW Ambulance and Triple Zero (000) calltakers answer a call for medical assistanceevery 28 seconds and only 10 per centof these calls are to patients with lifethreatening conditions. patient must have one cardiac or respiratory causeThe second phase of the campaignencouraged members of the community to a cardiac arrest must be witnessed initial rhythm should be VF or VT or they are hypothermic 32C2CHEER TRIALIn 2016/17 a new clinical trial commencedbetween NSW Ambulance, Royal PrinceAlfred (RPA) Hospital and St Vincent’sHospital which aimed to revolutionise howparamedics respond to cardiac arrestcases.2CHEER is a clinical trial which isinvestigating how a mechanical ExternalCardiac Massage (ECM), hypothermia,ECMO (extracorporeal membraneoxygenation) and early cardiac reperfusioncan improve survival rates of individualswho have suffered a cardiac arrest.NSW Ambulance Year in Review 2016/17The mechanical device involved in this trialis the Lucas2 device, which produces aconsistent, uninterrupted compression withgood palpable output.This means compressions are able to becontinued effectively throughout extricationand transport even in a carry sheet orstokes litter.The trial was conducted from six stationsin close proximity to the CBD as patientsmust be transported to either RPA or StVincent’s hospitals within a predefined timeframe.Intensive Care Paramedics (ICPs) havebeen trained to operate the machine andunderstand the 2CHEER trial benefits.patient centredcarefully consider whether they really needan ambulance, a paramedic or a stretcherbefore calling Triple Zero (000).doesn’t mean they will not receive anappropriate level of care through analternate pathway.treatment pathways available to patients,before or after they make a Triple Zero (000)call.The campaign aimed to realign communityexpectations by showcasing the alternatetreatment pathways available, empoweringpatients and their loved ones to make aninformed decision about the right levelof care they require instead of seeing anambulance and hospital treatment as theirfirst or only option.The community was educated that NSWAmbulance paramedics attending nonurgent cases could mean a patient witha life threatening emergency may have towait, potentially putting their life at risk.It also includes an emergency gauge withcommon conditions listed in a sliding scalefrom non-urgent to emergency.The messaging #Rightcallrightcaredemonstrated that just because a patientdoesn’t receive a lights and siren responseA series of posters were developed to showhow various conditions can be triagedand addressed via a range of appropriatetreatment pathways.Right call, right care In 2016-17 NSWAmbulance provided1,122,101 total responses(both emergency andnon-emergency). The total number ofemergency responses(P1-P2) for 2016-17 was985,799 compared to963, 562 for 2015-16.This reflects an annualincrease of 2.3% inemergency responses. On average, there were atotal of 3074 responsesper day during 2016-17which is the equivalentto an average of oneresponse every 28.1secondsThe colourful campaign is made up of fourposters which clearly show the range of or patient had an overdose with reversible cardiacdepression or patient has other reversible causes (PE/asthma).Exclusions include: cardiac arrest was due to trauma or active bleeding elected not for resuscitation (NFR) patient has known comorbidities or limitations8NSW Ambulance Year in Review 2016/179
Meeting Demandpatient centredThe scope for the campaign is unlimitedand it is anticipated a reboot and thirdphase will be rolled out in 2018 in responseto surge events and periods of highdemand.On average, each NSW Ambulancecampaign element posted on Facebookhas a reach of 1.4million people and Twitteraround 980,000 people.Do you need?Do you need?Do you need?Do you need?Life saving treatment?Life saving treatment?Life saving treatment?Life saving treatment?Severe blood loss, unconsciousness, chest pain orstopped breathingSevere blood loss, unconsciousness, chest pain orstopped breathingSevere blood loss, unconsciousness, chest pain orstopped breathingSevere blood loss, unconsciousness, chest pain orstopped breathingHealth advice?Health advice?Health advice?Health advice?Or if you’re unsure if you need medical careOr if you’re unsure if you need medical careOr if you’re unsure if you need medical careOr if you’re unsure if you need medical careMedical attention?Medical attention?Medical attention?Medical attention?For abdominal pain, diarrhoea or a grazed kneeFor abdominal pain, diarrhoea or a grazed kneeFor abdominal pain, diarrhoea or a grazed kneeFor abdominal pain, diarrhoea or a grazed kneeRelief?Relief?Relief?Relief?For a cough, cold or a sore throatFor a cough, cold or a sore throatFor a cough, cold or a sore throatFor a cough, cold or a sore throatYou need a paramedic.Call Triple Zero (000) immediately.You don’t need a paramedic.Call HealthDirect on1800 022 222You don’t need a paramedic.Visit your GP or call an after hourshome GP service.You don’t need a paramedic.Choose self care, or visit apharmacy.If unsure, call Triple Zero (000) and we’ll you the right care for your condition.If unsure, call Triple Zero (000) and we’ll you the right care for your condition.If unsure, call Triple Zero (000) and we’ll you the right care for your condition.If unsure, call Triple Zero (000) and we’ll you the right care for your e clipboard poster, with a simple tickbox process, showing the recommendedpathway for the condition, providingsupport and guidance on what care wassuitable.Through green, red and yellow, boththe clipboard and thermometer postersNSW Ambulance Year in Review ded a touch point so potential callerscould stop and take stock of their conditionand adjust their expectations.This campaign educates patients with nonlife-threatening or non-urgent conditionsnot to expect a double crewed stretcherambulance response.Patients may be referred by NSWAmbulance Triple Zero (000) call takers orparamedics to healthdirect Australia, whichis staffed by registered nurses, or to theAfter Hours Medical Deputising Servicewhich will provide a doctor to the patient’shome.The campaign material was mainlydistributed via social media and throughstakeholders and prompted additionaltraffic and engagement with the contentvia the NSW Ambulance website, Twitter,Facebook and Instagram accounts.It is important that NSW Ambulance helpthe community to understand that justas every patient attending an EmergencyDepartment does not necessarily getadmitted to hospital, not every patient whocalls Triple Zero (000) will necessarily needor receive an ambulance or paramedicresponse.NSW Ambulanceparamedicsattending medicalemergencies couldmean a patient with a lifethreatening emergency mayhave to wait, potentiallyputting their life at risk.Meeting DemandTRANSFER OF CAREFor the first time the Bureau of HealthInformation (BHI) included NSW Ambulancedata in its Healthcare Quarterly report forthe period of January to March 2017.While NSW Ambulance’s transfer of careperformance has always been featured inBHI quarterly reports, this is the first timethe report has provided such a detailedexamination of our patient responseperformance and operations.transferred to hospital staff within 30minutes, an increase of 0.8 percentagepoints. The number of calls to Triple Zero (000)rose to 281,668 (up 0.7 per cent on thesame quarter last year. The NSW Priority 1A (most criticalpatients) median response time was7.5 minutes for the January to Marchquarter. The Priority 1 (all 1A, 1B, 1C cases)median response time was 11.1minutes in the January to Marchquarter. This ranged from 9.3 minutesin Sydney to 12.6 minutes in theHunter which has a wider geographicalresponse area. In the January to March 2017 quarter,the NSW median mobilisation timewas 2.4 minutes for Priority 1 and 4.0minutes for priority 2 responses. 62.5 per cent of Priority category 1mobilisations were within the threeminutes. 43.7 per cent of Triple Zero (000) callswere Priority 1 (emergency – e.g.breathing problems/unconscious), 44.4percent were priority 2 (urgent – e.g.abdominal pain).Assessing time of call to ambulancearrival time for all 18 ambulance zones inthe January to March quarter, the reportprovided an important benchmark tomonitor performance levels against otherareas of the health system.The BHI report found that there hasbeen a continued increase in demand foremergency medical responses acrossNSW, with NSW Ambulance providing277,218 individual ambulance responsesfrom January to March this year. Thisreflects a 1.2 per cent increase on the samequarter in 2016.Despite the continued increase in demand,response times remained stable for the twomost urgent priority categories over thepast three years.Other findings in the report included:10 145,801 patients were transported byparamedics to hospital in the quarter. 91.5 per cent of patients whoarrived by ambulance had their careNSW Ambulance Year in Review 2016/17patient centred 94.7 per cent of priority category 1patients (emergency cases) had acall to ambulance arrival time within30 minutes. These are patients that,for example, experience breathingproblems or were unconscious. 95.0 per cent of priority category 2patients (urgent cases) had a callto ambulance arrival time within 60minutes. These are patients thatexperience, for example, abdominalpain.All ambulance local response areasmet the target of 90 per cent of priority2 responses with a call to ambulancearrival time within 60 minutes.163 of 200 stations reported on metthe target of 90 per cent of priorityone responses achieving a call toambulance arrival time within 30minutes. Of the 37 that did not, 28 ofthese stations are on call overnightmeaning activation time was one factorin response times, as was travel time. Eight stations improved their averagecall to ambulance arrival time within 30minutes by greater than 5 per cent inthe most urgent case category (priority1).As always, there is room for improvementand we will continue to strive to deliverappropriate timely care to our communities.11
To be a paramedic or NSW Ambulance staffmember comes with a core responsibility– and that is - to never lose sight of the privilegebestowed on you . the ability to play a role –frontline or otherwise – in ensuring care gets to apatient who needs us.”- Chief Executive Dominic MorganNSW Ambulance Year in Review 2016/1712NSW Ambulance Year in Review 2016/1713
Meeting Demandpatient centredAmong these initiatives: NSW Ambulance Year in Review 2016/17The implementation of the ParamedicResponse Network (PRN) operationalmodel which is being progressivelyrolled out across metropolitanSydney. The PRN model is specificallydesigned to better distributeparamedics across metropolitanSydney, allowing them to deliver highquality, mobile, emergency medicalcare to the community.In regional and rural NSW, wecontinued rolling out the RegionalAmbulance InfrastructureReconfiguration (RAIR) program, whichis delivering the biggest transformationof regional and rural NSW Ambulanceinfrastructure in our history.In order to further improve responsetimes, NSW Ambulance also regularlymakes adjustments to paramedicdeployments to better match ourdemand patterns and ensure wedeliver clinical care to urgent patientsas quickly as possible.Our ability to meet patient demand hasalso been aided through the delivery ofsignificant NSW Government fundingincluding 12.8 million as part of the2016 state budget for 85 frontline NSWAmbulance staff.patient centredALTERNATIVE TREATMENTPATHWAYSTo assist us to continue to meet demandfor emergency medical responses rightacross the state, NSW Ambulance isimplementing a number of major initiativesaimed at enhancing our capabilities. Integrated Carean additional 7.5 million in the2017 budget for 50 additional reliefparamedics across rural and remoteNSW which will assist with managingabsence and fatigue. The introduction of the new MakeReady Model into superstations willsupport paramedics by employingnon-clinical staff to clean and restockambulances to make paramedics moreavailable. Funding of 4 million for thisprogram was announced in the 2017State Budget. An expanded new suite of communityeducation programs was developedto teach and promote the ‘urgency oremergency’, ‘save Triple Zero (000)for saving lives and ‘big accident/littleaccident’ key messaging to all sectorsof the community.This continues to be achieved throughparamedics responding to the wishes ofpalliative patients with Authorised CarePlans or NSW Health Resuscitation Plans.These strategies include Low AcuityPatient Referral to Alternate Destinations,Palliative and End of Life Care, AgedCare, Paramedic Connect, FrequentUser Management and initiatives withResidential Aged Care Facilities.Low acuity patient careIn 2016 a Memorandum of Understanding(MOU) was established with a number ofAfter Hours Medical Deputising Services,providing paramedics with a ‘see andrefer’ pathway for low acuity patientswho call Triple Zero (000) and whosecondition does not warrant transport to anEmergency Department.NSW Ambulance’s See, Treat, Refer andDischarge integrated care pathwaysinclude assessment, treatment, and/orNSW Ambulance also received14NSW Ambulance continues to worktowards providing quality palliative andend of life care for patients with a lifelimiting illness, as supported by theAgency for Clinical Innovation’s Blue PrintPalliative Model of Care and the NSWHealth Advance Planning for Quality Endof Life Action Plan 2013-2018.To support the right care philosophyin 2016/17 NSW Ambulance rolled outa range of integrated care strategies,which provide patients with appropriatealternative treatment pathways,consequently contributing to a reductionin the volume of Emergency Department(ED) transports.Each strategy has been developed inorder to strengthen and deliver integratedcare and establish new low acuitypathways through Local Health Districts(LHD), social service providers, PrimaryHealthcare Networks and non-governmentorganisations.To meet increasing local demand,NSW Ambulance began working toprogressively implement 24 houron-duty operations at a number ofstations that have not traditionallyoperated under this model, toassist with managing staff fatigueand improving mobilisation times,enhancing our ability to deliver timely,high quality out-of-hospital care forthe communities surrounding thesestations. This year NSW Ambulancehas increased staff numbers tosupport 24 hour on-duty operations atMerimbula, Laurieton, Oak Flats andMaclean Ambulance Stations.Palliative and end of life careNSW Ambulance Year in Review 2016/17A number of resources and tools havebeen developed to support paramedics inproviding palliative and quality end of lifecare.referring patients to care providers otherthan hospitals.These programs improve integrationand patient connectedness and eachpathway decision can reduce case cycletimes and also assists in eliminatingdelays associated with transfer ofcare, ambulance vehicle availabilityand avoiding clinically unnecessarypresentations.Low acuity patient care including theassessment and referral to alternatedestinations continues to be a growingchallenge for NSW Ambulanceparamedics.Paramedics are now supported by aTreatment and Referral Decisions protocoland a strengthened Referral Decisionprotocol.During 201516 paramedicsundertook 29,373patient referrals to analternative care pathway.”This approach ensures that the decisionsabout care are jointly made and inclusiveof the patient, the paramedic and asappropriate with the GP.A protocol was developed andimplemented across NSW to supportqualified paramedics to formally undertakeVerification of Death.Verification of Death is a clinicalassessment process to establish that aperson has died. Using standard clinicalassessment tools, a qualified paramediccan establish and document that deathhas occurred.The successful implementation of thismodel of care means paramedics haveimproved operational capacity through adecreased case cycle time and availabilityto respond to emergencies, as well asfreeing up hospital Emergency Departmentcapacity15
Integrated CareAGED CAREThe Aged Care Emergency (ACE) serviceis a partnership between Hunter NewEngland Health and the Hunter NewEngland Central Coast Primary HealthNetwork.It is dependent on collaborativerelationships with Residential Aged CareFacilities (RACFs), NSW Ambulance,Primary Health Networks (PHNs) andgeneral practitioners (GPs).The service provides triage, consultancy,clinical support, and advice for RACFstaff and GPs, so care for patients can bedelivered in the facility where appropriateand transfers to hospital are avoided.The ACE service provides information,and when necessary, assists with thecoordination of outreach or outpatientservices for clinical issues such as woundmanagement, continence problems,behavioural issues, IV antibiotic therapy,and the management of some acute andchronic conditions.patient centredIntegrated CareHow does it work? Local registered nurses answer ACE calls within the EDMonday to Friday within business hours. After Hours nurses take ACE calls from RACFs, using triagealgorithms to determine the best care for patients andalso providing advice to assist RACF staff on care for theirpatients. These tria
NSW Ambulance ICP's were the first non-doctors in NSW to go into theatres, do intubations and cannulations. The first ICPs were launched in 1977 and regarded by many as 'cowboys' because they were delivering care that only doctors could do. Graduating at a time of immense change, ICPs arrived when NSW Ambulance was
![MOH STANDARDS FOR EMERGENCY AMBULANCE SERVICE (2017) [Updated 21 Nov 2018]](/img/51/emergencyambulancestandards.jpg)