Transcription
Our result:All Florida children, youth and families have good oralhealth and well-being, especially those that arevulnerable.1
Table of ContentsAcknowledgements Page 3Background and Call to Action . .Page 4Story Behind the Baseline .Page 7Partners Page 17What Works . .Page 18Headline Indicator 1: Percentage of Medicaid-eligible Children 0 – 20 who received any dental serviceHeadline Indicator 2: Percentage of Medicaid-eligible Children 1 – 20 who received any preventive dental serviceIndicator Baselines . Page 25Story Behind the Curve . .Page 28What works? Page 30Results-Based Accountability for Collective Impact .Page 40Resources . Page 43Endnotes .Page 442
Acknowledgements:We would like to thank the following Florida Oral Health Alliance partner organizations for theircontributions to this plan:Agency for Health Care Administration (Florida Medicaid)Catalyst MiamiChildren’s Services Council of Broward CountyChildren’s Services Council of Palm Beach CountyThe Children’s TrustClear ImpactDental Health and WellnessDentaQuest (Florida)Florida Association of Community Health CentersFlorida CHAINFlorida Dental AssociationFlorida Department of Health Public Health Dental ProgramFlorida Department of Health in Palm Beach CountyFlorida Department of Health in Pinellas CountyFlorida Healthy KidsHealth Care District of Palm Beach CountyHealth Choice NetworkLiberty Dental PlanMiami-Dade College School of Health Sciences Dental Hygiene ProgramNova Southeastern University School of Dental MedicinePremier Community Health Care Group - Pasco CountySpecial Olympics FloridaTampa Bay Healthcare CollaborativeThis plan was developed using Results-Based Accountability as presented in the book Trying Hard IsNot Good Enough by Mark Friedman. Deitre Epps from Clear Impact facilitated this planning process.The Florida Institute for Health Innovation expresses our utmost appreciation to the DentaQuestFoundation for their support of the Florida Oral Health Alliance.3
Background: The oral health of Florida’s vulnerable childrenThe Pew Charitable Trust’s June 2013 children’s dental report entitled, In Search of Dental Care: Two Types ofDentist Shortages Limit Children's Access to Care, ranked Florida first among all 50 states as having the highestpercentage of children covered by Medicaid who did not see a dentist in 2011 – 75.5%, over 20 points higherthan the national average. i In addition to the Pew report, Florida Medicaid reported that in 2011 only 23% ofchildren eligible for Medicaid received any dental care with just 14% receiving preventive care. In 2015, 35% ofFlorida’s Medicaid eligible children received any dental services and 33% received preventive dental care.Although this shows considerable improvement over four years, Fl orida’s outcomes still fall behind the 2015national average: 47% of Medicaid-eligible children in the United States received any dental service (assupervised by a dentist) and 45% received preventive dental care nationally. iiFlorida’s children experience a high level of tooth decay. The August 2016 Florida Department of Health Burdenof Oral Disease Surveillance Report stated that a 2014-2015 oral health survey of 26 Head Start (HS) centersacross Florida found an estimated 17.8% of HS children with early childhood caries, 20.9% with untreated decay.17.3% of these children needed early care and 4.6% needed urgent care. According to a 2013-2014 survey ofthird grade students from 41 Florida schools, 43.1% had caries experience, 23.4% had untreated caries, 18.3%needed early care and 4.9% needed urgent care. Overall, non-Hispanic Black children had the highest diseaserates.iii Specifically, the rate of early childhood caries was highest among Hispanic children (21.1%). Non -HispanicBlack children had the highest rates of untreated decay (23.6%) and the highest rates of “need early care”(19.1%) and “need urgent care” (6.6%). ivIn Florida, children’s oral health problems have generated significant health care spending. In 2014, 31,524,982was spent on dental-related Emergency Department (ED) visits among children ages 0-20, representing 13.4% oftotal dental-related ED visit charges in the state. v A new report published in the 2016 Journal of Public HealthDentistry cited that dental-related visits to the ED have increased each year between 2005 and 2014 from104,642 to 163,900. Additionally, dental charges tripled during this period from 47.7 million to 193.4 million.Medicaid (38 percent) and self-pay (38 percent) made up the highest percentage of primary payors of dentalrelated ED visits in 2014. viCall to actionThe Florida Oral Health Alliance, a broad-based, multisector group ofstakeholders, is issuing a call to action to improve access to andutilization of dental care for Florida’s most vulnerable children. Asmembers of the Alliance, we pledge to leverage our influence, resourcesand ability to achieve collective impact in order to create statewidesystems change. We will work together to facilitate, plan and implementstrategies based on the needs of our most vulnerable children. Using adata-driven, results-based collaborative process, we, the Florida OralHealth Alliance, have designed this strategic oral health plan based onour state oral health environment. We will use CMS-416 data to track ourprogress. Incorporated into this plan is information provided by Florida’sOral Health Consumer Advisory Council.4
Our areas of focus include: Oral health education Barriers to dental care Increased funding for oral health Improved data collectionThe resultIn response to this crisis, in 2015, a cross-sector group of providers and academic, public health, philanthropic,state, community and corporate partners with an interest in children’s health formed the Florida Oral HealthAlliance for the purpose of improving access to and utilization of dental care for Florida’s most vulnerablechildren. Convened and facilitated by the Florida Institute for Health Innovation, the Florida Oral Health Alliance(the Alliance) collaboratively crafted a result that states that “All Florida children, youth and families have goodoral health and well-being, especially those that are vulnerable.” Using the framework of Results-BasedAccountability (RBA), the Alliance employed Turn the Curve thinking to develop this strategic p lan forcommunities and stakeholders interested in increasing oral health equity and improving the oral health ofvulnerable children.Headline success indicatorsTo measure success toward our result, the Alliance chose the following indicators based on the best availabledata: The percentage of Medicaid-eligible children ages 0 – 20 who receive any dental service each year The percentage of Medicaid-eligible children ages 1 – 20 who receive any preventive dental service eachyearThis data is retrieved from the Center for Medicare and Medicaid Services’ (CMS) 416 report as provided by thestate Medicaid agency, the Florida Agency for Health Care Administration (Florida Medicaid). “Any dentalservice” includes both preventive services like cleanings and sealants as well as restorative services such ascavity treatment. “Dental services” refers to services provided by or under the supervision of a dentist.Supervision is a spectrum and includes, for example, direct, indirect, general, collaborative or publi c healthsupervision as provided in the state’s dental practice act.5
Data development agenda:At the beginning of the process (in May and July 2015), theAlliance began forming a data development agenda toinclude additional data that would help to track successtoward our result. The data development agenda included: Number of children that receive unaccounteddental services (no claims) Number and types of services provided by CDTcodes No show rates Other non-Medicaid (e.g. private, employeesponsored) children and youth receiving preventivedental services Other non-Medicaid (e.g. private, employee-sponsored) children and youth receiving any dental services ICD-10 diagnostic dataThe Florida Institute for Health Innovation report Florida Pediatric Emergency Department Visits for PreventableOral Health Conditions: 2012, was originally referenced as a possible secondary indicator. In March 2016, theUniversity of Florida published updated data to include Florida’s dental-related emergency department visits bypatient county of residence, age and primary payer. This updated data can be accessed lhealth/docs/actionteams/data collection/Dental ED Visits ByCounty CY2014.pdfBecause physician diagnoses alone may underestimate the frequency of ED encounters for dental con ditions,the 2014 study’s operational definition of an ED visit due to a dental -related reason was based on the patient’sreported reason for seeking care (admitting diagnosis) or the physician’s primary diagnosis of the problem. Thestudy defined the ED visit as being for a dental problem if the admitting diagnosis or primary diagnosis wascoded as one of the following ICD-9-CM codes: 520 – 526.9, 528 – 528.9, 784.92, V52.3, V53.4, V58.5, or V72.2.These codes are identical to those used in a recent analysis of national ED data by the American DentalAssociation.11For this report, all 2014 dental -related visits to Florida Emergency Departments (EDs) were coded for evaluation andmanagement. Five current Procedural Terminology (CPT) codes accounted for more than 95% of the visits: 99281 (ED visitfor the evaluation and management that includes problem-focused history, problem-focused examination, andstraightforward medical decision-making; 9.4%); 99282 (ED visit that includes expanded problem-focused history, expandedproblem-focused examination, and medical decision making of low complexity; 33.2%); 99283 (ED visit that includesexpanded problem-focused history, expanded problem-focused examination, and medical decision making of moderatecomplexity; 44.4%), 99284 (ED visit that includes detailed history, detailed examination, and medical decision making ofmoderate complexity; 7.3%) and 99285 (ED visit that includes comprehensive history, comprehensive examination, andmedical decision-making of high complexity; 0.9%). In addition, 29.5% of the patient visits were coded for at least oneadditional service or procedure during the visit. More than 560 unique CPT or Healthcare Common Procedure CodingSystem (HCPCS) codes were entered, although ten codes accounted for more than half of the services provided: five ofthose involved injection of local anesthesia or other substances (codes 96372, 96374, 64400, 64402, J1885). Otherprocedures in the top ten included drainage of abscesses (41800), providing prescr iption drugs (J8499), collection of venousblood (36415), urine pregnancy test (81025), or non-covered items or services (A9270).6
Additional data accessed during the planning periodincludes Florida Medicaid’s Medical Managed Assistance(MMA) Dental Services Profile, a data visualization. TheDental Service Profile was designed to assess utilizationof dental services for Florida Medicaid recipientsenrolled in a managed care plan. Managed MedicalAssistance program (MMA) enrollees were evaluated todetermine if they received at least one dental serviceduring the first year of MMA implementation, August 1,2014 through July 31, 2015.The data shows: High utilization percentages (45% – 55%) are similar to the national average of 60% Low utilization for two to three year olds High utilization in second and third graders Managed care profiles show how different plans serve different populations Need for data on special needs populationsThe group stated that this data can be used in the following ways: Identify utilization differences by region and by county in order to target low utilization areas, race andethnicity Examine higher performing areas and figure out what is working Target services toward parents of one to three year olds by integrating into maternal -child healthprogramsAlso during the planning period, the American Dental Association’s Health Policy Institute (HPI) released TheOral Health Care System: A State-Level Analysis. Florida’s fact sheet revealed that only 30% of children withMedicaid coverage in Florida visited a dentist in the past 12 months in 2013 as compared to the national averageof 48%. The percentage of dentists in Florida participating in Medicaid for child dental services in 2014 (30%)was also significantly lower than the national average (42%). In addition, the survey showed that oral healt hknowledge and attitudes differed among Florida residents based on income level. Low -income adult residentshad an oral health status index of 8.5 out of 10, based on a scale of 1 being poor oral health and 10 beingexcellent oral health, compared to 6.6 for low-income adult residents. 51% of high-income adult Floridaresidents answered all of HPI’s 2015 oral health knowledge survey questions correctly compared to 43% of low income residents. vii The Alliance used these new data sources to inform the plan’s story behind the baseline andstrategy ideas.Story behind the baselineFlorida’s story behind children’s dental care access and utilization outcomesIn order to design appropriate change strategies, the Alliance planning group developed a list of factors thatboth drive and restrict progress toward achievement of the result. From this extensive list (included below), thegroup prioritized six factors to be used as the impetus for strategy development.7
These include:1. There is a lack of understanding of the impact of community decisions and personal beliefs on oralhealth, the importance of preventive dental care and the value of oral health.2. There is a lack of information regarding available dental services and how to access them.3. There are available dental health services that are not being accessed.4. Inadequate funding does not provide access to services which leads to a low number of provi ders, lackof coverage and benefits.5. There is a lack of consistent collaboration from partners and stakeholders, including oral healthunderstanding by legislators.6. Services are not meeting the needs of the population, including special needs and children needingspecial procedures.7. There is a lack of real time data that can identify which patients need dental care. Data is needed at thepatient level.We have explained each factor based on Florida’s current oral health landscape.1. There is a lack of understanding of the impact of community decisions and personal beliefs on oralhealth, the importance of preventive dental care and the value of oral health.Oral health education has not beenintegrated into all school districts and is notbeing discussed in many communities.School-based health education does notinclude oral health’s connection to overallhealth nor does it address how communitydecisions impact oral health (ex.community water fluoridation, fooddeserts). Parents have limited access toknowledge about how to achieve oralhealth. In general, groups educatingcommunities are not exploring theimportance of culture, race or ethnicity oncommunities’ perceptions of oral health.To achieve oral health and prevent dental disease requires self-care, care of others, community programs,policies, laws and regulations and reimbursement structures that support evidence-based interventions andpractices. Obtaining, understanding and using information to prevent oral diseases and promote oral health areessential parts of personal health maintenance; are the foundation of the skills and effectiveness of caregivers;and are imperative for policy makers in order to make effective decisions. Developing oral health knowledgeincludes acquiring and trusting information, skill development, grasping concepts and technique-intensiveprotocols, and applying them appropriately. Studies indicate that approximately 80% of dental disease fallswithin 25% of the population and primarily affects vulnerable populati ons including low income families.Individuals with less oral health knowledge are less likely to seek preventive dental care and more likely to utilizeemergency care for oral health problems. Vulnerable populations lack political, social and economic pow er.Therefore, we feel that it is imperative to educate legislators, advocates and other change agents to increasetheir understanding of the importance of prevention and the value of oral health.8
2. There is a lack of information regarding available dental services and how to access them.Throughout the planning process, Alliance participants maintained that Medicaid beneficiaries, medical/dentalproviders and health and human services organizations lack information about comprehensive dental benefitsfor children available under the Medicaid program. This includes information regarding the broad range ofMedicaid benefits, how to fully access these benefits through Medicaid managed care (including accessingtransportation to dental appointments) and the availability and access to services for special populations (suchas children with special needs or children from non-English-speaking families).Alliance and Consumer Advisory Council discussions revealed that Medicaid beneficiaries and key st akeholdersdo not have the information needed to overcome barriers to dental care nor do they have information regardinggrievances and appeal rights. Asset maps that list resources and available service locations have not beendeveloped. In addition, direct service providers working with oral health consumers are not fully aware of howthe dental care system works. This points to a need for an orientation that explains the Medicaid system andbenefits. With the shift to Medicaid managed care, dental benefi ts vary from plan to plan. This causes confusionregarding CMS and Medicaid services, resulting in delays in obtaining dental services.Several factors have contributed to this lack ofinformation and to Florida’s poor access andutilization outcomes for vulnerable children.These include Florida’s switch from a Medicaidfee-for-service model to Medicaid managedcare. Pursuant to a change in statute, in 2014,the Florida Agency for Health CareAdministration (Florida Medicaid), implementedthe statewide transition to managed care formost Medicaid recipients. The goal of thistransition was to improve health outcomesusing the strategies of care coordination andpatient engagement, coupled with fiscalresponsibility. Medicaid Managed Assistance(MMA) plans are required to providecomprehensive and integrated services includingmedical, dental and behavioral health care.Contract requirements require them to perform a Performance Improvement Project to improve the use ofpreventive dental services by children, and there are contract benchmarks for preventive dental and treatmentservices. Some stakeholders assert that this shift has allowed for an increase in child eligibility and coverage.Others state that it has increased bureaucratic burden for providers.3. There are available dental health services that are not being accessed.Evidence points to numerous reasons that Medicaid enrollees choose not to use services when providers andcoverage are available. Reasons include a lack of information regarding the benefits of dental treatment, longwait times and fear or distrust of available providers. A 2011 study by the Centers for Disease Control andPrevention (CDC) on dental care access among Hispanic and Latino groups found that those most likely to9
underutilize dental services were poor or near poor,foreign-born or had lived in the U.S. for less than fiveyears.viiiAccording to the Florida Oral Health Consumer AdvisoryCouncil, this underutilization of dental services can also beattributed to a lack of cultural competency among personsinforming families about benefits and makingappointments. This includes people working at insurancecompanies, the Medicaid agency and dental offices.For example: People answering phones for insurance companies andMedicaid do not know the importance of oral health. Consumers are not aware of what is available to them (interpreters, transportation to appointments, etc.). Mandated/available services are not being communicated. For example, heal th plans are required by thestate to find dental care for consumers “in a timely manner” which includes 30 days non -emergent and oneto two days for urgent needs.Furthermore, research shows that the use of untrained, unprofessional interpreters, such as family members,can lead to a substantially higher risk of medical errors and negative health outcomes. Since there are a shortageof oral health professionals within communities of color that share the same racial/ethnic background as thepatients they serve, people of different racial and ethnic backgrounds often rely on their social referral system,avoiding healthcare professionals or insurance providers that perceivably lack the cultural competency tounderstand their distinct background. Additionally, racial and ethnic minorities with Limited English Proficiency(LEP) may refer to community social networks rather than oral health care experts when seeking medical advice.Improving the diversity and cultural competency of oral health professionals is essential to successfullyaddressing oral health needs in a growingly diverse population. ixIn 2016, HB5101 bill extended Florida KidCarecoverage to lawfully-residing immigrantchildren, without a five-year waiting period,beginning on July 1, 2016. To date, thesechildren were required to wait for five yearsbefore receiving any Florida KidCare benefits.This law change will provide additionalenrollment opportunities into the FloridaKidCare Program2 , which includes health anddental benefits to children ages birth through18 years old. This will increase the need forculturally and linguistically competent workers.2Florida KidCare is the State of Florida’s high-quality, low-cost health insurance for children. The program was createdthrough Title XXI of the Social Security Act and reauthorized in 2009. Through its four partners, including Florida HealthyKids, the program covers children from birth through age 18.10
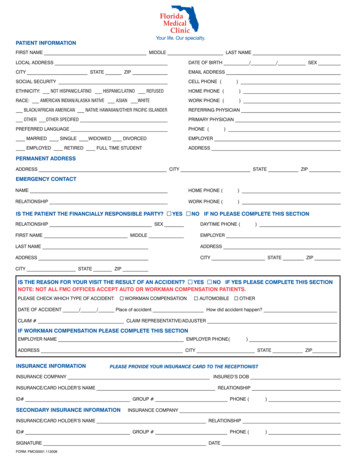
In addition, available school-based oral health services are not being accessed because of a lack of enforcementand a low consent form return rate. In Florida, dental exams are not required for school entry. However,included on the School Entry Health Examination form 3 it is recommended that a parent obtain a comprehensivedental exam for their child. The form provides a place for the dentist to record the finding of this exam. Floridalaw in section 1003.22 F.S. and section 6A-6.024 FAC requires any child who is entering a Florida school for thefirst time to present proof of a health examination. The exam must include a review of all body systemsperformed by a licensed medical provider within 12 months prior to enrollment. It is recommended thatchildren receive a comprehensive dental exam by a dentist, but the law also requires a “gross” dental exam by amedical provider. However, this requirement is for a “gross dental exam” is not being enforced.The Alliance planning group researched the use of “opt-out” consent for in-school dental services. The grouplearned that dental services and screenings are viewed as “i nvasive procedures” and therefore they do notqualify for inclusion on an “opt out” form like the consent process used for physical health screenings. Section381.0056, F.S., which is the Florida law regarding the provision of school health services, requires an activeconsent for invasive procedures. Since these diagnostic and preventive procedures include placing a mirror orplacing materials such as sealants in the mouth, Florida considers these procedures invasive and thus requiresactive consent. Therefore, dental care and screening require that parents “opt in” in order for their children toreceive in-school dental services.4. Inadequate funding does not provide access to services which leads to a low number of providers, lackof coverage and benefits.According to the American Dental Association Health Policy Institute’s October 2014 Research Brief, A Ten-Year,State-by-State, Analysis of Medicaid Fee-for-Service Reimbursement Rates for Dental Care Services, there exists apositive relationship between Medicaid fee-for-service (FFS) reimbursement rates and utilization of dental careamong publicly insured children as well as dentist participation in Medicaid. Low Medicaid FFS reimbursement isa major factor in influencing the success of Medicaid programs. Therefore, a nationwide trend in decliningreimbursement rates poses a serious concern for the ability for states to offer accessible dental care services.Thirty-nine states including Florida experienced a decline in the Medicaid-to-commercial-dental insurance feeratio for pediatric dental services between 2003 and 2013. In 2003, Florida ranked among the top two stateswith the lowest Medicaid FFS reimbursement as a percentage of commercial dental insurance charges forpediatric dental care services (36.7%) and among the top 8 in 2013 (36.6%), as shown below. Florida’sreimbursement rates were significantly lower than the national average of 57.4% in 2003 and 48.8% in 2013.3Students in grades kindergarten through 12th grade who are making their initial entry into a Florida school must present arecord of a physical examination completed within the past 12 months. The exam record should be taken to the child'sschool upon enrollment. This operates according to Florida Statute (s. 1003.22(1), F.S.). Although a specific form is notrequired, it is recommended that Florida's standardized School Entry Exam form (DH 3040 -CHP-07-2013) be used todocument completion of a physical examination. It must be completed by a health care provider licensed in the UnitedStates to perform physical examinations. For students transferring to a Florida school, a comparable form from anotherstate would also be acceptable, if completed within 1 year.11
Top 10 States with Lowest FSS Reimbursement Rates in200370.00%60.00%57.40%50.00%40.00%30.00%40.40% 40.60% 42.80%33.40%44.00% 44.90% 45.70%36.70% 38.60% 38.70%20.00%10.00%0.00%1District of ColumbiaFlorida**Rhode on**MarylandNational AverageTop 10 States with Lowest FSS Reimbursement Rates in201360.00%48.80%50.00%36.60% 37.10%40.00%30.00%26.70% 27.90% 29.00%39.50%31.50% 32.50% 32.50% 32.60%20.00%10.00%0.00%1Minnesota**Rhode *Florida**New YorkNew HampshireNational Average12
Evidence shows states that have significantlyreformed their Medicaid programs, including anincrease in Medicaid dental reimbursement rates,including Connecticut, Maryland and Texas, haveexperienced an increase in dental care use forMedicaid eligible children. Beyond improving accessto dental care, increasing dental care reimbursementrates also leads to a significant increase in providerparticipation. We believe that this will close thegrowing gap in dental care utilization between lowincome and high-income patients. xIn the state of Florida, legislative statute (466.023 subsection 3) states that a Registered Dental Hygienist (RDH)can provide fluoride-varnish and education in a health access setting. Health access settings include schools,community health centers and health departments and increase opportunity for preventive dental care at alower reimbursement rate. The Florida Legislature has enacted legislation to encourage health care practitionersto provide their services in public schools in accordance with s. 381.0056, Florida Statutes (F.S.). This legislation,section 381.00593, F.S., the public school volunteer health care practitioner program, includes services by adentist or dental hygienist licensed under chapter 466, F.S.An Alliance subcommittee contacted the Department of Education and was advised that current Florida law,section 381.0056, F.S., requires the local health department and county school district to collaboratively developan annual school health services plan. Each school health services plan describes local strategies andresponsibilities for implementing activities that promote the health and well-being of students to support theiracademic success. Therefore, policies and procedures for school health services, which include dental services,are developed and implemented at the local county school district level. This process may be another avenue topursue to include dental screening and services in Florida schools.Florida has increased its funding for community water fluoridation. The Florida Department of Health and thestate’s oral health coalition, Oral Health Florida, have been working with partners to promote an increase incommunity water fluoridation through federally-funded community education and support for fluoridated watersystems. A cost-effective method for preventing tooth decay, community water fluoridation has been shown toreduce dental decay by 25% over a person’s lifetime (AFS: n
across Florida found an estimated 17.8% of HS children with early childhood caries, 20.9% with untreated decay. 17.3% of these children needed early care and 4.6% needed urgent care. According to a 2013-2014 survey of third grade students from 41 Florida schools, 43.1% had caries experience, 23.4% had untreated caries, 18.3%