Transcription
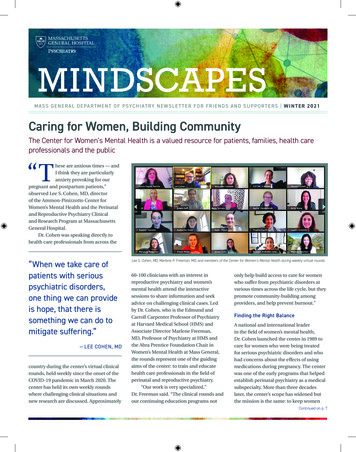
M A S S G E N E R A L D E PA RT M E N T O F P SYC H I AT RY N E W S L E T T E R F O R F R I E N D S A N D S U P P O RT E R S W I N T E R 2 0 2 1Caring for Women, Building CommunityThe Center for Women’s Mental Health is a valued resource for patients, families, health careprofessionals and the public“These are anxious times — andI think they are particularlyanxiety provoking for ourpregnant and postpartum patients,”observed Lee S. Cohen, MD, directorof the Ammon-Pinizzotto Center forWomen’s Mental Health and the Perinataland Reproductive Psychiatry Clinicaland Research Program at MassachusettsGeneral Hospital.Dr. Cohen was speaking directly tohealth care professionals from across the“When we take care ofpatients with seriouspsychiatric disorders,one thing we can provideis hope, that there issomething we can do tomitigate suffering.”— LEE COHEN, MDcountry during the center’s virtual clinicalrounds, held weekly since the onset of theCOVID-19 pandemic in March 2020. Thecenter has held its own weekly roundswhere challenging clinical situations andnew research are discussed. ApproximatelyLee S. Cohen, MD, Marlene P. Freeman, MD, and members of the Center for Women’s Mental Health during weekly virtual rounds.60-100 clinicians with an interest inreproductive psychiatry and women’smental health attend the interactivesessions to share information and seekadvice on challenging clinical cases. Ledby Dr. Cohen, who is the Edmund andCarroll Carpenter Professor of Psychiatryat Harvard Medical School (HMS) andAssociate Director Marlene Freeman,MD, Professor of Psychiatry at HMS andthe Abra Prentice Foundation Chair inWomen’s Mental Health at Mass General,the rounds represent one of the guidingaims of the center: to train and educatehealth care professionals in the field ofperinatal and reproductive psychiatry.“Our work is very specialized,”Dr. Freeman said. “The clinical rounds andour continuing education programs notonly help build access to care for womenwho suffer from psychiatric disorders atvarious times across the life cycle, but theypromote community-building amongproviders, and help prevent burnout.”Finding the Right BalanceA national and international leaderin the field of women’s mental health,Dr. Cohen launched the center in 1989 tocare for women who were being treatedfor serious psychiatric disorders and whohad concerns about the effects of usingmedications during pregnancy. The centerwas one of the early programs that helpedestablish perinatal psychiatry as a medicalsubspecialty. More than three decadeslater, the center’s scope has widened butthe mission is the same: to keep womenContinued on p. 7
IA Messagefrom the Chiefwrite to you when it is not yet spring, but notthe depths of winter either. COVID-19, it ishard to believe, has been with us for one yearnow. This issue of Mindscapes aptly illustratesthe work of the Department of Psychiatry duringthese challenging times. Our “virtual” patient carecontinues to be accessible, compassionate andinnovative. We are, in fact, providing more carethan ever before. In the last three months of 2020,department clinicians made 11% more outpatientvisits than in the same period in 2019. And 98% ofthose visits were virtual.As the cover story on the Ammon-PinizzottoCenter for Women’s Mental Health illustrates,we are using online technologies such asvideoconferencing to expand access to care, shareour expertise with health care professionals andprovide information to people wherever theyare. With COVID-19 exacerbating levels of stress,anxiety and depression, our faculty membershave stepped up to provide advice and solace invirtual venues ranging from webinars and blogsto podcasts and video interviews.At the same time, our groundbreaking researchto inform patient care continues. As you will read,we recently launched the Center for PrecisionPsychiatry to identify people early in the courseof their illness or at risk for suicide. The newCenter for the Neuroscience of Psychedelics isstudying the potential of psychedelics to makethe brain receptive to change, which could leadto improvements in mental health conditions likesevere depression. In addition, our researcherscontinue their work on developing digitalapplications, including those for smartphones,to make current treatment as accessible andaffordable as possible. And we are committed toproviding new treatments for our patients. WithFDA approval of esketamine for treatment-resistantdepression, the department will be one of thefirst in the country to prescribe esketamine to ourpatients; we are working to make it available in ourintravenous ketamine clinic.These are all vital aspects of our mission tolessen suffering and reduce stigma. I am trulyinspired by our department’s incredible facultyand staff, and I am honored to serve as theirchief. Medical science and technology — whencombined with empathy, compassion, a firm beliefin facts and a strong commitment to equity — willcontinue to see us through.MAURIZIO FAVA, MDPsychiatrist-in-ChiefCreating a Roadmap for EquityApriority for the Department of Psychiatry is to address systemicracism, institutionally and individually. Psychiatrist-in-ChiefMaurizio Fava, MD, convened an anti-racism task force last fall with thecharge of drafting a strategic plan to create a roadmap for change.“We will focus on structural remedies,” Dr. Fava said. “We need tobe explicit that our department’s framework going forward will be oneof anti-racism.”The department’s anti-racism program will align with MassGeneral’s overarching equity plan. As one of its first steps, the23-member task force commissioned a survey of the department’s500 members, which garnered more than 300 responses.The survey found significant support for establishing a systemto report occurrences of racial bias within the department. Nearly70 percent of respondents indicated it was “very important” thatresearchers use an anti-racism lens in framing research questions.Department-wide training and education to change the culture wasranked as an urgent priority for anti-racism strategic planning.“We were overwhelmed by the response,” said Derri Shtasel, MD,MPH, who is one of three task force co-chairs, with Jonathan Jenkins,PsyD, and Nhi-Ha Trinh, MD, MPH. “This is about inclusion, and we need2mass general department of psychiatryJoseph Betancourt, MD, MPH, Vice President and Chief Equity and Inclusion Officer with theMigration is Beautiful butterflyeveryone’s voices for this effort to be successful.”Next steps for the task force include submitting recommendationsto Dr. Fava and creating a structure for implementation.
New Center Focuses on Precision Psychiatry to Reduce “Trial and Error”The Department of Psychiatry haslaunched a new center to identify risk formental illness early on and eliminate theprocess of “trial and error” through tailoredtreatment for individual patients.“Precision psychiatry, with its focuson individual differences in biology, genes,lifestyle and environment, is a new, emerging way of looking at how we approachpsychiatry and mental health,” said JordanSmoller, MD, inaugural director of theCenter for Precision Psychiatry. “The centerwas created to drive this transformationalshift, and I believe we have a tremendousopportunity to make a difference.”A major focus is to develop tools thatprevent suicide. Deaths from suicide haveincreased by more than 35% in the past20 years, making it the second leadingcause of death among young people. Thecenter will use electronic health recordsand computational methods like machinelearning to identify those at risk. “We’refinding that these methods providesubstantial improvement over what wecurrently do clinically,” Dr. Smoller says.The goals of risk prediction andprevention are also being applied toA Resource for Estate PlanningThe COVID-19 pandemiccontinues to pose complexchallenges for all ofus. Like any significantmoment in our lives, thepandemic forces us to lookat our long-term goals. Ifstructuring your charitablegiving for Mass Generalis one of your goals, now is an ideal time to thinkabout your legacy at the hospital.Planning your estate doesn’t have to becomplicated. We’ve created a guide — completewith checklists, definitions, tips and techniques— to help you navigate the process. To requestyour complimentary estate planning guide, pleasecall the Office of Planned Giving at 617-643-2220or download it at: www.giving.massgeneral.org/EPguide.tackle other pressing problems includingidentifying those at risk for PTSD anddeveloping strategies for preventingdepression. The center is working onalgorithms to match individual patients tothe most effective treatments and translatinggenetic discoveries into new therapies.In keeping with the department’s longstanding mission, the center will integrateresearch with patient care. One example:a suicide consultation risk managementteam that specializes in identifyingand managing suicide risk. Dr. Smollerenvisions a “learning health care system”to speed up the time it takes for research toimprove care.A renowned psychiatric geneticist,Dr. Smoller is uniquely positioned to leadthe interdisciplinary center. He is associatechief for Research, director of thePsychiatric and NeurodevelopmentalGenetics Unit, and a principal investigatorin the NIH All of Us Research Program,the largest-ever national research effort toadvance precision medicine. A professor ofPsychiatry at Harvard Medical School, heis also the MGH Trustees Endowed Chairin Psychiatric Neuroscience and presidentJordan W. Smoller, MD, ScDof the International Society of PsychiatricGenetics.Plans are underway for the first-in-thenation conference on precision psychiatry,as well as for the creation of trainingresources to disseminate discoveries tothose on the front lines of care. The centerhas also assembled a talented team,including Richard Liu, PhD, recruitedfrom Brown University for his expertise insuicide risk assessment.“To build the research infrastructureand the engine to drive this forward, wehave tremendous needs for support,”Dr. Smoller notes.SAVE-THE-DATESThe Massachusetts General Hospital Department of Psychiatry invites you to attend free, onlineeducational sessions designed for patients, families and friends. To learn more or to register,please email mghevents@partners.org.Supporting the Mental Health ofOlder Adults: Research Advancesand Innovative Approaches to CareApril 7, 2021, 4pmMGH Geriatric Psychiatry Clinical andResearch Program leaders will discuss thelatest in mental health research, treatmentand care for older adults.Pediatric Psychiatry OCD andTic Disorders OverviewApril 15, 2021, 4pmErica Greenberg, MD, will lead a discussion onthe Pediatric Psychiatry OCD and Tic DisordersProgram.MGH Leadership Council forPsychiatry 10th Annual Visiting DayJune 7, 2021Distinguished Department of Psychiatryfaculty will present the latest updates inclinical care and research and share theimpact of philanthropy on their work.COVID-19 and Mental HealthInformationThe Mass General Psychiatry Guide to MentalHealth Resources for COVID-19 is updatedregularly. Visit lth-resourcesmindscapes newslet ter3
Cathy Seilhan: Finding Hope and Giving BackCathy Seilhan looks back on her teenage self and realizes shealways had “an extreme kind of emotion and mood. When Iwas sad, I was very sad. When I was happy, I was very happy.”Even with these mood swings, “life was kind of easy” forCathy. But adulthood — a challenging marriage, a new baby anda demanding career as an educator — created so much stress,sadness and anxiety that she found herself unable to cope.Finally, one day at school during cafeteria duty, a young boyasked how she was doing. “I broke into tears and I couldn’t stopcrying,” she recalls.The school principal whisked her out the door and into theoffice of the school’s trusted diagnostician. The two professionalssat with her for hours as it became clear that she needed morethan an office visit. Cathy was eventually admitted to a behavioralhospital, diagnosed first with major depressive disorder and thenbipolar disorder. She spent six weeks in outpatient treatmentbefore she returned to school.It was as if nothing had happened. “Back then, people didn’ttalk about mental illness,” she notes. “We kept each other in thedark. It seemed like no one would understand, and it seemed tooscary to open. The stigma was huge.”“When you are given the diagnosis, thegame isn’t over. It is just beginning.”— CATHY SEILHANGrateful to the Dauten Family CenterCathy credits her happier and healthier life to her husband, Denton,and to Andrew Nierenberg, MD and his team at the Dauten FamilyCenter for Bipolar Treatment Innovation. The grateful Seilhans aregenerous supporters of the Dauten Center. “I think [the DautenCenter team members] are going to make breakthroughs in ourlifetime,” Denton says. “We are happy to be a part of that.”With bipolar disorder, Cathy says, “practicing forms ofmeditation has great benefits. I began learning the power ofstepping back and being curious about my emotions, insteadof being a victim of them. That was a huge breakthrough.”A Supportive PartnerCathy and Denton married in June 2010. From the beginning,Cathy was honest with him about her illness and its effects. SaysDenton, “it can be really hard. When Cathy is doing well, everythingis so simple and beautiful. When she is having difficulties, it canget tense. It takes a lot of patience and understanding.”4mass general department of psychiatryDenton and Cathy SeilhanDenton also found it helpful to talk to a mental healthprofessional to gain understanding and insight. “He’s learned alot,” Cathy says. “He’s loyal. He’s not going anywhere because of it.”Effective Holistic SolutionsFinding the most effective treatment for Cathy was a “trial anderror” process. She had difficulty tolerating the side effects ofmedication.“When you are given the diagnosis, the game isn’t over,” shesays. “It is just beginning.”The breakthrough occurred when Dr. Nierenbergrecommended that Cathy try over-the-counter supplements. Thatled her to renew a focus on diet and exercise — even a 10-minutewalk would prove beneficial. She is thankful that Dr. Nierenbergalways made the case for the holistic approach. It was cognitivebehavioral therapy, not medication, that became the bedrock ofher treatment.“Over time, I was calmer and less irritable, and happier,” shesays. “I was able to regulate my emotions.”Today, she is retired, which, she contends, makes it easier tobe more open about mental illness, with no worry about stigmaand loss of livelihood.“I want everybody to feel better,” Cathy states, “and to share inmy hope. The frontier is very exciting, and I live a deeply meaningfullife with my bipolar disorder. I want others to know that they can too.”
The Arielle Soussan Fund for Psychedelic Research:A Young Woman’s LegacyWayne Blank won’t forget aconversation with his younggranddaughters at a diner nearhis art gallery 18 years ago. “I was puttingmoney away for them and asked, ‘what areyou going to do with your money?’ Arielle,who was then 7 years old, spoke up rightaway. I’m going to give my money to charity.”That was just like Arielle, he explained,a brilliant and sensitive young womanwho radiated kindness and cared deeplyabout the world. She was keenly aware ofits inequities and wanted to make thingsbetter. Arielle cared about her friendsand the people she loved. Whether it washelping someone overcome their shynessor standing up for someone who was beingbullied, “Arielle was always helping herfriends,” says her mother, Keren Soussan.Arielle’s LegacyA year after her death at age 24, Arielle’sfamily has fulfilled her wish with a giftto the Center for the Neuroscience ofPsychedelics at Mass General. The ArielleSoussan Memorial Fund for PsychedelicResearch supports groundbreaking work toexplore how psychedelics impact the brainand alleviate suffering in people with majordepression.Arielle herself struggled with intractabledepression. While her family was aware ofher depression and her continual search foran effective treatment, they did not realizeher life was in danger. “Her grandmotherand I are discovering now the depths of herdespair, how desperate she really was,” saysWayne Blank.But she was also funny andmischievous, with a love for poetry andmusic and cats and a passion for readingand writing in both French and English.Buoyed by her curiosity and sense ofadventure, Arielle traveled the world,living in Australia for six months andIsrael for two years. In San Francisco,she volunteered for an organizationArielle Soussanhelping undocumented immigrants withapplications for visas. In Haifa, Israel,she worked in a shelter for children ofbattered women.Arielle graduated in 2017 with abachelor’s degree in communicationsand culture from Indiana University inBloomington, a college she selected inlarge part because of its bucolic campus.At the time of her death, she was a freelancenewspaper writer in Bloomington, coveringmusic and movies.Arielle was troubled by the stigma ofmental illness, contrasting the support forcancer patients with the lack of supportgiven to people with a mental illness. “Ariellewas right. I hope that this will change in mylifetime,” says her mother.In part because of her own struggles,Arielle had expressed interest in thepotential of psychedelic compounds for thetreatment of mental illness. “She would havebeen a good candidate for psychedelics. Sheneeded something to help change themind,” her grandfather Wayne believes.The Center for the Neuroscience ofPsychedelicsJerrold Rosenbaum, MD, psychiatrist-inchief emeritus at Mass General, and oneof the world’s authorities on mood andanxiety disorders, founded the Center forthe Neuroscience of Psychedelics earlierthis year because of the promise thatpsychedelic compounds hold to transformmental health care treatment. Studiesshow that even a single dose of thesecompounds can bring previously treatmentresistant patients into remission andprovide sustained relief. “What we dohere has the potential of one day changingmillions of lives for the better,” statesDr. Rosenbaum.The mission of the center is tounderstand how psychedelics promoteneuroplasticity and enhance the brain’scapacity for change, to optimize currenttreatments, create new options for treatingmental illness, and, ultimately, make theterm “treatment resistant” obsolete.“Psychedelic compounds hold thepotential to move the dial on the capacityfor change and provide hope to those inmost need of hope, patients with treatmentresistant illness,” states Sharmin Ghaznavi,MD, PhD, associate director of the centerand director of Cognitive Neuroscience,adding, “patients like Arielle.”In addition to Drs. Rosenbaum andGhaznavi, the center’s leadership includesBruce Rosen, MD, director of the AthinoulaA. Martinos Center for Biomedical Imagingand pioneer of functional magneticresonance imaging and Stephen J. Haggarty,PhD, a leading chemical neurobiologist.Philanthropist and entrepreneur DickSimon, who aims to reduce the stigma andraise awareness of psychedelic treatmentsfor mental health issues, chairs the center’sadvisory board.“The whole team is very impressive,”says Shoshana Blank, Arielle’s grandmother.“We feel that we made a very, very gooddecision.”Arielle’s fund is supporting threeinaugural studies on the effects of psilocybinon different features of treatment resistantdepression. In Dr. Ghaznavi’s words,“Arielle’s story is a reminder of why we dothe work we do.”To contribute to the Arielle SoussanMemorial Fund visit san/.mindscapes newslet ter5
The Advantage of Talk TherapyRobert Waldinger, MD, says many emotional problems can be solved by psychodynamic (talk) therapy.More than 20 million Americans seekhelp each year for emotional problems.The Endowment for the Advancement ofPsychotherapy at Massachusetts GeneralHospital ensures that highly effectivepsychodynamic or insight-oriented therapyis available for patients in need througheducation, research and professional training.Robert Waldinger, MD, is a psychiatristand psychoanalyst at Mass General; professorof Psychiatry at Harvard Medical School;and a Zen priest. Dr. Waldinger serves as codirector of the endowment with Carl Marci,MD, a Mass General psychiatrist, scientist andentrepreneur.What is psychodynamic therapy?It’s the kind of therapy that encouragespeople to talk in depth about their lives —not just about what’s troubling them, butwhat they care about the most. It helpspeople connect their previous experienceswith what’s happening now, so they can seepatterns in their lives.A classic example is the person whofights with every boss they work for. Intherapy, the patient may begin to recallmemories of a difficult father who constantlydemanded blind obedience. The patientmay come to realize a pattern of castingevery new boss in the role of a ‘dictator’ andin this way accidentally undermining workrelationships. Seeing this kind of pattern canbe enormously liberating, freeing people tomake wiser choices.You are a Zen priest. How does that informyour work as a psychotherapist?Both psychotherapy and meditation areways of studying the mind. Zen helps ussee the difference between the stories ourminds create about the world and what theworld is really like. The analogy often usedis the difference between reading a menuand tasting the food. Our descriptions ofthe world — for example, a description ofthe taste of chocolate — cannot begin to dojustice to experiencing the real thing.6mass general department of psychiatryMany people who are hurtingemotionally end up in a primary caredoctor’s office, and some people getmedication they don’t need, or surgeriesthey don’t need. We know that at least halfof these doctors’ visits for physical ailmentsare emotionally based. Many of theseproblems can be better helped bytalk therapy.What are the challenges involved in thepractice of this type of therapy?Robert J. Waldinger, MDRecognizing that stories about ourlives are not the whole truth is one way thatpsychotherapy can relieve suffering. BothZen and psychotherapy help us see thateverything constantly changes, that yourcurrent low mood or difficult situation is notgoing to stay that way — a much-neededperspective when people feel stuck. Thetruth of impermanence has been especiallyhelpful for me during this pandemic.What is the Endowment’s mission?We train mental health professionalsin psychodynamic perspectives andtechniques that can inform every area ofmental health care. The Department ofPsychiatry does not want this approach tomental illness to go away. In 2010, I wasrecruited to Mass General with the expresspurpose of ensuring that psychodynamicthinking is always taught to our trainees.“So that tomorrow, there will be someone totalk to,” is the Endowment’s motto.Could you describe the training?It starts with illustrating very basic premisesabout how the mind works. Instead of justteaching theory, we use vivid case examplesto show students how psychodynamicprinciples operate both in their ownlives and in their patients’ lives. Researchdemonstrates that psychodynamic therapyis very effective — as powerful or morepowerful than medication for anxiety anddepression.Insurance companies are worried thatpeople will linger in psychotherapy forever.But in fact, when people are offered apsychotherapy benefit in their health plan,they do not overuse it, and it reduces othermedical costs.The vast majority of people who comefor psychotherapy want to get the workdone, feel better and get on with their lives.There is a more limited role for long-termpsychotherapy, and it can be cost effectivein keeping people out of the hospital. Apsychiatric hospitalization can cost tensof thousands of dollars. Seeing a therapistonce a week or once a month doesn’t costmuch at all by comparison.How can philanthropy make a difference?Expensive medical procedures are muchbetter reimbursed than primary carevisits and psychotherapy. The lack ofparity in insurance reimbursement isone of the reasons why philanthropy isso important.We need support for trainingprograms and for professional developmentopportunities such as conferences andfellowships in advanced psychotherapy sotrainees can take a much deeper dive intothese therapeutic techniques. We especiallyneed support for endowed positionsto ensure the long-term stability andsustainability of this teaching program.For more information, pleasevisit ment
Caring for Women, Building Communitycontinued from p. 1and their families emotionally well by providing high-qualitycare informed by groundbreaking research. Finding the rightbalance between treating psychiatric illness and choosing theright treatment is a major dilemma for patients and clinicians,who must grapple with the question, what are the risks and whatare the benefits? Center clinicians are experts at tailoring effectivetreatments to women before, during and after pregnancy whileminimizing the risk to the fetus of potentially harmful exposure tomedications.Optimizing wellness before pregnancy is a main tenet of thecenter. “Our focus is on helping a woman to pause, and to reallyget psychologically well in anticipation of a pregnancy,” Dr. Cohennotes. If a woman is pregnant or postpartum, the goals are tomaintain or even achieve remission from psychiatric disorders.He added, “The pandemic has broadened that focus.”Providing Resources During a PandemicPregnant and postpartum patients were deeply affected byCOVID-19 in the early days of the surge. The pregnancy and deliveryexperience they hoped for suddenly was no longer possible.Without having in-person, new mother support groups availableafter delivery and direct support from family members outside thehome, many patients reported a sense of isolation and sadness.Telemedicine, however, made it possible to continuecomprehensive initial consultations as well as ongoing careto monitor the effects of prescribed medications, observethe emotional status of patients and modify treatment plansaccordingly. “These virtual visits allow us to keep women welland out of the hospital for psychiatric care as much as possible,”Dr. Cohen said.The center, with its long-standing role in the deliveryof comprehensive women’s mental health resources, waswell-positioned to transition to virtual care, education, andconsultation when COVID-19 hit. The center’s website,www.womensmentalhealth.org, offers the latest resources,articles on scientific advances and other educational materialsfor patients, providers and the public. During the pandemic,visits to the website are up 38 percent.Research is Essential to the MissionStemming from the pandemic, the center is researching theimpact of the coronavirus on maternal and infant health andwellbeing during pregnancy and the postpartum period. Inaddition, the center is currently conducting several new clinicaland translational research studies. One is the MGH PostpartumPsychosis Project (MGHP3.org), which aims to identify potentialunderlying genetic risk factors associated with this severe illness.“This is an important undertaking as very little is knownabout the factors which contribute to postpartum psychosis, theLee S. Cohen, MDMarlene P. Freeman, MDmost severe and potentially life-threatening form of postpartumdepression,” said Dr. Cohen.The center recently enrolled their 2,000th patient as part of theNational Pregnancy Registry for Psychiatric Medications. The goalof this registry is to gather information on the safety of psychiatricmedications such as antidepressants during pregnancy that willhelp to inform evidence-based treatment decisions and will guidefuture studies. The center is also seeking support for clinicalresearch on women of reproductive age diagnosed and treatedfor ADHD, as there is a lack of data to inform and guide medicalchoices for women when it comes to treatment during pregnancy.The research initiatives, as well as the focus on education andclinical care, speak to the center’s patient-focused mission. “Whenwe take care of patients with serious psychiatric disorders, onething we can provide is hope, that there is something we can do tomitigate suffering, that any improvement can be meaningful, thatwe are going to stay in the game,” Dr. Cohen notes.Persistence and Determination are KeyThat philosophy was in evidence during the recent virtualrounds, when Dr. Freeman described three years of persistent,determined, treatment trials to help a seriously ill patient — themother of young children who experienced severe and disablingobsessive compulsive disorder after delivery of her son. Aftermany medication trials, she was still suffering greatly, as was herfamily. Finally, deep brain stimulation provided relief. The patient’shusband reported that it was as if “a switch had flipped.”“We encourage patients to partner with us until we cancollaboratively find a treatment solution that leaves them in abetter place,” Dr. Cohen said.“It had taken a really long time,” Dr. Freeman said of herpatient’s successful outcome, repeating a favorite inspirationalquote: You never say never, you never say always, and always saythere is one more thing to try.mindscapes newslet ter7
Nonprofit Org.U.S. PostagePAID125 Nashua Street, Suite 540Boston, Massachusetts 02114-2548N. Reading, MAPermit No. 211If you do not wish to receive certain or all fundraising communications from Mass General, please call 877-644-7733, or visit giving.massgeneral.org/com-pref.Dr. Uchida is doing just that. As a childpsychiatrist and director of Mass General’sChild Depression Program, she is working withcolleagues at Biederman Lab and the GabrieliLab at MIT to understand how biological factorscontribute to underlying vulnerability in teens.“Just as high cholesterol and hypertensionare warning signs for heart attack, mooddisorders
Psychiatry 10th Annual Visiting Day June 7, 2021 Distinguished Department of Psychiatry faculty will present the latest updates in clinical care and research and share the impact of philanthropy on their work. COVID-19 and Mental Health Information The Mass General Psychiatry Guide to Mental Health Resources for COVID-19 is updated regularly.