Transcription
Cárdenas-Valladolid et al. BMC Family Practice (2018) EARCH ARTICLEOpen AccessEffectiveness of standardized nursing careplans to achieve A1C, blood pressure, andLDL-C goals among people with poorlycontrolled type 2 diabetes mellitus atbaseline: four-year follow-up studyJ. Cárdenas-Valladolid1,2,3,4*, A. López-de Andrés4,5, R. Jiménez-García4,5, M. J. de Dios-Duarte6,P. Gómez-Campelo3,4,7,8, C. de Burgos-Lunar3,4,5,9,10, F. J. San Andrés-Rebollo4,11, J. C. Abánades-Herranz3,4,12and M. A. Salinero-Fort3,4,9,13AbstractBackground: No studies that have measured the role of nursing care plans in patients with poorly controlled type2 diabetes mellitus. Our objectives were firstly, to evaluate the effectiveness of implementing Standardizedlanguages in Nursing Care Plans (SNCP) for improving A1C, blood pressure and low density lipoprotein cholesterol(ABC goals) in patients with poorly controlled type 2 diabetes mellitus at baseline (A1C 7%, blood pressure 130/80 mmHg, and low-density lipoprotein cholesterol 100 mg/dl) compared with Usual Nursing Care (UNC). Secondly,to evaluate the factors associated with these goals.Methods: A four-year prospective follow-up study among outpatients with type 2 diabetes mellitus: We analyzedoutpatients of 31 primary health centers (Madrid, Spain), with at least two A1C values (at baseline and at the end ofthe study) who did not meet their ABC goals at baseline. A total of 1916 had A1C 7% (881 UNC versus 1035SNCP). Two thousand four hundred seventy-one had systolic blood pressure 130 mmHg (1204 UNC versus 1267SNCP). One thousand one hundred seventy had diastolic blood pressure 80 mmHg (618 UNC versus 552 SNCP);and 2473 had low-density lipoprotein cholesterol 100 mg/dl (1257 UNC versus 1216 SNCP). Data were collectedfrom computerized clinical records; SNCP were identified using NANDA and NIC taxonomies.Results: More patients cared for using SNCP achieved in blood pressure goals compared with patients whoreceived UNC (systolic blood pressure: 29.4% versus 28.7%, p 0.699; diastolic blood pressure: 58.3% versus 53.2%,p 0.08), but the differences did not reach statistical significance. For A1C and low-density lipoprotein cholesterolgoals, there were no significant differences between the groups. Coronary artery disease was a significant predictorof blood pressure and low-density lipoprotein cholesterol goals.Conclusions: In patients with poorly controlled type 2 diabetes mellitus, there is not enough evidence to supportthe use of SNCP instead of with UNC with the aim of helping patients to achieve their ABC goals. However, the useof SNCP is associated with a clear trend of a achievement of diastolic blood pressure goals.Keywords: Patient care planning, Diabetes mellitus type 2, Prospective studies, Outcome assessment, NANDA, NIC* Correspondence: juan.cardenas@salud.madrid.org1Dirección Técnica de Sistemas de Información, Gerencia Asistencial deAtención Primaria, Servicio Madrileño de Salud, C/ San Martín de Porres, 6,28035 Madrid, Spain2Universidad Alfonso X el Sabio, Villanueva de la Cañada, Madrid, SpainFull list of author information is available at the end of the article The Author(s). 2018 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, andreproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link tothe Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication o/1.0/) applies to the data made available in this article, unless otherwise stated.
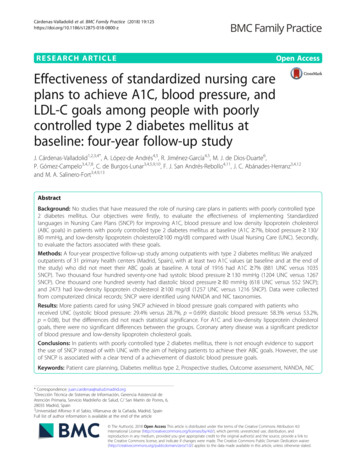
Cárdenas-Valladolid et al. BMC Family Practice (2018) 19:125BackgroundIn Spain, approximately 6 million people have diabetesmellitus (DM) [1], and this number is increasing annually[2]. DM represents a major public health problem becauseit is a well-known risk factor for stroke [3], coronary arterydisease (CAD) [4] and cardiovascular disease [5].Poor control of blood pressure (BP), lipids, and glycosylated hemoglobin (A1C) is strongly associated with adverse outcomes in patients with type 2 DM (T2DM) [6].The American Diabetes Association (ADA) recommendsthat patients with DM achieve their ABC goals, namely,A1C 7%, BP 130/80 mmHg, and low density lipoprotein cholesterol (LDL-C 100 mg/dl [7]. However, atleast one-third of patients with T2DM [8] fail to achievetheir ABC goals.The responsibility for the care of patients with T2DMin Spain has shifted to multidisciplinary teams based inprimary health care (PHC) settings that are composedmainly of family doctors and nurses.Achieving ABC goals for T2DM patients depends onseveral factors, such as physical activity levels [9], stressreduction [10], medication adherence [11], and meal plans[12]. These targets form the basis of wide range of interventions implemented by nurses and aimed at improvingdiabetes care and achieving metabolic control [13].In the last decade, there has been a considerable improvement in Standardized languages in Nursing CarePlans (SNCP) with NANDA-International [14] NursingDiagnoses and Interventions (NIC) [15]. Since 1998,these taxonomies have been progressively incorporatedinto clinical practice and computerized clinical records(CCR) in Madrid (Spain). However they are still notused by 100% of nursing staff [16].Our group recently established the effectiveness of SNCPfor improving health outcomes for T2DM patients [17].However, to our knowledge, no studies have measured therole of nursing care plans in patients with poorly controlledT2DM. Accordingly, we hypothesize that SNCP may be effective in helping patients with poorly controlled T2DM toachieve their ABC goals. We also consider that it is necessary to know the magnitude of the effect of SNCP and tocompare it with that of other therapeutic strategies.Our study had two objectives. First, we evaluated the effectiveness of SNCP as a component of CCR registration forhelping patients with poorly controlled T2DM at baseline(A1C 7%, blood pressure 130/80 mmHg, and LDL-C 100 mg/dl) to achieve their ABC goals and compared ourfindings with those of Usual Nursing Care (UNC), providedby dedicated trained nurses in PHC settings, second, weevaluated the factors associated with meeting ABC goals.MethodsThis study was conducted as part of a broader researchproject which is described in detail elsewhere [17, 18]. APage 2 of 10prospective cohort follow-up study was carried out between March 2008 and February 2012 in T2DM patientsattending follow-up appointments with a nurse at PHCcenters.The two types of nursing care plans implemented:SNCP (n 2105) and UNC (n 2105) were delivered byregistered nurses trained in diagnostic reasoning basedon NANDA-I and NIC taxonomies and working in 31PHC centers in the northeastern area of the city ofMadrid, Spain.Eligibility criteria for patients were: age 30 years with atleast two records in the CCR during the previous year andan International Classification of Primary Care [19] codeindicating T2DM (T90). Patients were not selected if theymet any of the following exclusion criteria: gestational diabetes, being homebound, and a life expectancy of less than1 year (according to the physician’s clinical judgment).The number of patients selected for this study waslower than in the our previous study [17], as we preferred to restrict our analysis to patients from the SNCPgroup with at least two A1C values (baseline and end ofstudy) over the four-year follow-up (n 2105) Therefore,we decided to select a random sample of an equal size inthe UNC group (n 2105).Figure 1 provide details of the study procedure, patientsrecruitment and exclusion, and patients without baselineand final A1C, LDL cholesterol and BP values Only thosewith poor diabetes control were finally included.The sample size was calculated taking into account aUNC: SNCP ratio of 1:1.10 (estimated a proportion of30% patients with A1C 7% in the UNC group, alpharisk of 0.05 and a beta risk of 0.20 in a two-sided test). Asample size of 873 UNC patients and 1029 SNCP patients is necessary to recognise a statistically significantrelative risk of good glycemic control (A1C 7%) of 1.22 in the UNC vs. the SNCP group. A drop-out rateof 0.05 was anticipated.We only analyzed patients who did not meet their ABCgoals at baseline: A1C 7% (n 1916; 881 with UNC and1035 with SNCP), systolic blood pressure (SBP) 130 mmHg(n 2471; 1204 with UNC and 1267 with SNCP), diastolicblood pressure (DBP) 80 mmHg (n 1170; 618 with UNCand 552 with SNCP) and LDL-C 100 mg/dl (n 2473;1257 with UNC and 1216 with SNCP).MeasuresData were collected under routine clinical practice conditions from CCR at PHC centers in the Madrid HealthService and processed using OMI-AP software., TheCCR was previously validated for patients with a diagnosis of T2DM [20].SNCP was identified based on the following threecriteria:
Cárdenas-Valladolid et al. BMC Family Practice (2018) 19:125Page 3 of 10abcdFig. 1 Procedure and patients included in the study, stratified by ABC goal. ABC goals: (a) HbA1c 7%, (b) SBP 130 mmHg, (c) DBP 80mmHg and (d) LDL-C 100 mg/dl; UNCP: Usual Nursing Care; SNCP: Standardized languages in Nursing Care Plans; HbA1c: glycosylatedhemoglobin; DBP: diastolic blood pressure; SBP: systolic blood pressure; LDL-C: low-density lipoprotein-cholesterol
Cárdenas-Valladolid et al. BMC Family Practice (2018) 19:125– Criterion 1. The patient has a CCR code thatcorresponds to Gordon’s functional health patterns[21] in at least one of the following areas: activityand exercise; nutritional and metabolic; and healthperception and health management.– Criterion 2. The problems identified were describedusing nursing diagnosis statement codes based onthe NANDA-I taxonomy, which is used in T2DMpatients. A nursing diagnosis based on NANDA-Itaxonomy is defined as a clinical judgment concerning a human response to a health condition/lifeprocess, or a vulnerability in that response, by an individual, family, group, or community and providesthe basis for selection of nursing interventions toachieve outcomes for which the nurse has accountability [14].– Criterion 3. The nursing intervention carried outwas registered according to the NIC taxonomycodes, which used in T2DM patients [15].The nurses who applied SNCP used the following domains: nutrition, coping/stress tolerance, life principles,health promotion, self-perception, perception/cognition,activity/rest and safety/protection. The main nursingdiagnoses were Imbalanced nutrition: more than bodyrequirements (00001), Non-compliance (00079), Ineffective self-health management (00078), Ineffective seeking behaviors: Management DM (00084),Deficient knowledge (00126), Sedentary lifestyle (00168)and Impaired skin integrity (00046). The same nursesalso delivered UNC to the control group.UNC was defined as the treatment and monitoring ofT2DM including control of blood sugar, control of cardiovascular risk factors, adherence to drug anagement according to local guidelines [22].The following variables were recorded: sociodemographic characteristics (gender, age), clinical variables (diabetes over time), personal health habits sucha as smoking(cigarettes/day) and drinking (alcohol units/week), physical activity (measured in hours per week with any exerciseor activity outside of the patients’ regular job erate-intensity, sedentary), associated morbidity (dyslipidemia, hypertension, coronary heart disease), complications of diabetes mellitus (retinopathy, nephropathy,neuropathy), and the type of treatment prescribed (dietaryand pharmacological). Biochemical–biological parameterswere also collected, as follows: body mass index (BMI),SBP, DBP, total cholesterol, LDL-C, high-density lipoprotein cholesterol (HDL-C), triglycerides, and A1C.Blood pressure was measured according to the recommendations of the Seventh Report of the Joint NationalPage 4 of 10Committee on Prevention, Detection, Evaluation, andTreatment of High Blood Pressure [23]; these recommendations were current at the start of this study.Cholesterol and triglycerides were determined usingenzyme assays. LDL-C was calculated according to theFriedewald formula [LDL-C total cholesterol (HDL-C trigycerides/5)] in participants with triglycerides below400 mg/dL. HDL-C was measured after precipitation ofapoB lipoproteins. A1C was measured using ahigh-performance liquid chromatography.Statistical analysisA descriptive analysis was carried out for each variable included in this study; quantitative variables were expressedas the mean and standard deviation and qualitative variables as. The chi-square test was used to compare the percentage of patients who achieved their ABC goals. Thet-test was used for quantitative data. Multiple logisticregression analysis was used to identify the variablesassociated with each goal (A1C 7%, DBP 80 mmHg,SBP 130 mmHg, and LDL cholesterol 100 mg/dl) andthe relationship between each ABC goal and selected predictor variables was examined. In addition, each logisticregression model was adjusted for all potential confounders, including the variables for which differences between the groups were observed at baseline.In all instances, the accepted level of significance was0.05 or less. The 95% confidence interval was reported.All analyses were carried out on an intention-to-treat(ITT) principle. With the analyses were performed usingSPSS (SPSS for Windows, V.19.0; IBM Corp, Armonk,New York, USA).ResultsThe demographic and clinical characteristics of patientswith poorly controlled T2DM at baseline, stratified by SNCPand UNC group
languages in Nursing Care Plans (SNCP) for improving A1C, blood pressure and low density lipoprotein cholesterol (ABC goals) in patients with poorly controlled type 2 diabetes mellitus at baseline (A1C 7%, blood pressure 130/ 80 mmHg, and low-density lipoprotein cholesterol 100 mg/dl) compared with Usual Nursing Care (UNC). Secondly,