Transcription
Teamwork and Malpractice: What's theConnection?April 13, 2022
Upcoming Team Training EventsWebinarsFlip Don’t Flop! Remodeling Communication Using Deconstructive Feedback – May 11 at 12 pm CTTelehealth and Its Emergence During the Pandemic – May 17 at 12 pm CTCourses & WorkshopsIn-person TeamSTEPPS Master Training Courseso May 16-17 at UCLAo May 24-25 at Dukeo June 7-8 at Tulaneo June 13-14 at NorthwellManaging Conflict in Health Care Workshop – Virtual workshop series taking place April 21-May 122
Today’s PresenterEnter headshot here(if applicable)David L. Feldman, MD, MBA, CPE, FAAPL, FACSChief Medical Officer, The Doctors Company, TDC Group3
Today’s ObjectivesTeamwork and Malpractice: What’s the connection?Define the nature ofmalpractice risk reduction,and the 3P modelDemonstrate the impact ofcommunication andteamwork on malpracticeratesUtilize malpractice data asa tool to engage hospitalleadership in patient safetyefforts4
Agenda Malpractice and risk reductionMalpractice data & the role of teamworkTeamwork, the patient & malpracticeEngaging leadership & insurers
Polling Question #1How do you feel about the role of malpractice in improving patientsafety?a. I'm already using malpractice data, want to use it moreb. Malpractice data is probably useful, but I don't have accessc. Malpractice is too rare an event to make the data meaningfuld. Malpractice is too arbitrary to make the data usefule. I don't know enough to answer the question
The Path to a LawsuitAdverse EventPatient/familycommunicationRisk ManagementInternal investigation“alert to carrier”Peer Review and/or Root Cause AnalysisQuality ImprovementReportingStateCMSTJCCorrective Action Planeducationsystem fixesPatient SafetyLawsuitTrialDropped/DismissedSettlement
The ABC’s of Malpractice Accepto Doctor-patient relationship Breacho Standard of practice Causeo “Proximate cause” Damageo Injury resulting from breach
The ABC’s of Malpractice One sentence definition:o Malpractice is a violated duty causingharm One word definition:o Unreasonableness
Medical Malpractice LitigationWhat does it involve?Plaintiff attorneys, with theaid of experts, try to make acase starting with a badoutcome and workingbackwards.RetrospectascopeThe principal piece ofevidence in virtually everymedical malpractice case isthe patient’s medical record.Courtesy P. Kolbert, Esq
Does the Medical Liability System Work?1452 Claim Files Reviewed1406 (97%) involved injury37 (3%) no injuryNo payment in 31 (84%)Error in 889 (63%)No error in 515 (37%)No payment in 370 (72%)Payment in 653 (73%)Payment in 6 (6%)Payment in 145 (28%)No payment in 236 (27%)Studdert, et.al. NEJM 354;19. 2006.
Reducing Malpractice RiskThe three “P’s” Prevent adverse events Preclude malpractice cases Prevail in lawsuits
Agenda Malpractice and risk reductionMalpractice data & the role of teamworkTeamwork, the patient & malpracticeEngaging leadership & insurers
Polling Question #2What is the biggest reason for malpractice cases?a. Poor clinical judgmentb. Unintended adverse eventsc. Bad teamwork between patients and providersd. Bad communication between providers about patientse. Poor documentation
Teamwork – Still a problemRosenbaum, NEJM, 2019.
Vanderbilt University Medical CenterCenter for Patient and Professional Advocacy Professional Conduct Policy Training for faculty ino Commitment to Credo behaviorso Feedback to students & residentso Behavior policy Patient Advocacy Reporting System (PARSSM) Co-Worker Observation Reporting SystemSM (CORSSM)
Vanderbilt Co-Worker Observation Reporting SystemSMDomain CodesDomain Subcategories Prevalence Domain Codes Domain Subcategories PrevalenceCompetent Medical CareResponsibilityPoor or unsafe care26Access/availability20Scope of Practice115Impairment1Failure/reluctance/refusal tocomplete role-related tasksFailure to accept feedback3Violation of statedorganizational values12Breach of patient/familyconfidentiality4Conflict of interests1False documentation1Clear & tinez, et.al., Jnl Pat Saf, 2018, 1-7.
Co-Worker Complaints & OutcomesNSQIP data from Stanford and VanderbiltPatients whose surgeons had higher numbers of coworker reports about unprofessional behavior in the 36months before the patient’s operation appeared to be at increased risk of surgical and medical complications.“.nurse [who] reports, “I asked for the procedure time out. Dr X said,‘Look, we’re all on the same page here. Let’s get going without all this timeout nonsense,’”Cooper, JAMA Surgery, 2019.
Teamwork Communication& Malpractice Ambulatory Care – 22% Unprofessional Responsibility unclear Inpatient Care – 18% Reading the EMR Reaching consensus ED Care – 19% Hierarchical issues19CRICO 2018 Benchmarking Report
Risk Management Issues in Surgery ClaimsAdverse eventSurgeryi.ii.iii.iv.Technical SkillJudgmentPatient’s DiseaseSystemsPreclude lawsuitDefendContributing Factors CategoryPossible technical problem resulting in known complicationPoor techniqueMisidentified anatomic structureSelection of procedureFailure to order testFailure to appreciate signs/symptomsCommunication amongst providers about condition/closed loopFailure of systems – undergoing/reporting tests, consultsClinical environment - Weekend/holiday/busynessSupervision of housestaffInadequate response to patient concernsInadequate consent for surgical procedurePatient expectations/poor rapportDocumentation issues – inconsistent, inaccurate, lack of, delayedElectronic Health RecordClaim Count
Risk Management Issues in OB ClaimsAdverse eventPreclude lawsuitDefend lawsuitContributing Factors CategorySelection/management of therapyPatient assessment issuesPatient monitoringFailure/delay in obtaining a consultTechnical performanceCommunication among providersClinical environmentClinical systemsPatient non-adherence with treatmentNon-insured issuesSupervision of housestaffCommunication with patient and familyInsufficient/lack of documentationInconsistent/inappropriate documentationInaccurate documentationClaim Count
Risk Management Issues in ED ClaimsAdverse eventPreclude lawsuitDefend lawsuitContributing Factors CategoryClaim CountOngoing assessment: monitoring of clinical statusOrdering of diagnostic testsFailure/delay in obtaining a consultCommunication among providers about condition/failure to read EMRClinical environment - busynessClinical environment – Weekend/holiday/night shiftPerformance of diagnostic testsAdministrative – EMR/staffing/policiesTechnical skillSupervision of house staffCommunication with patient and familyDocumentation issues – findings, rational, delayed, inconsistent
Risk Management Issues in ED ClaimsED Process of Care% of casesAverage indemnity1. Patient notes problem and seeks care6% 529,0002. Initial assessment: history and physical exam11% 816,0003. Ongoing assessment: monitoring of clinical status30% 653,0004. Ordering of diagnostic tests65% 525,0005. Performance of diagnostic tests5% 670,0006. Interpretation of diagnostic tests22% 463,0007. Transmittal of test results to (ED) provider7% 576,0008. Consultation management26% 566,0009. Development of discharge plan43%10. Post discharge follow-up (includes pending test results)9% 488,00011. Patient adherence to plan5% 220,00023 499,000CRICO 2011 Benchmarking Report
Communication & Handoff Failuresin Medical Malpractice Claims 498 random claims - Candello malpractice databaseo Communication errors in 244 (49%) – 130 (26%) among staffo Patient severity of illness 61 (54%)o Handoff errors (53%)*o Patient contingency plan 51 (45%)o Patient diagnosis 39 (34%)o Medication plan 16 (14%) Mean cost/case 359,000 (v. 130,000 staff & patient/family)*77% likely preventable with a handoff toolHumphrey, J Pat Saf, 2021.
Agenda Malpractice and risk reductionMalpractice data & the role of teamworkTeamwork, the patient & malpracticeEngaging leadership & insurers
Polling Question #3What’s the best way to engage with patients to avoid malpractice?a. Use good informed consent before treatment/proceduresb. Be sure to console patients after an adverse eventc. Explain treatment options in detail with patient and family togetherd. Apply shared decision making to all treatment decisionse. Maintain an ongoing relationship with patients before, during andafter treatment
Patient Complaints& Malpractice Risk 645 general and specialistphysicians, January 1992 - March1998; 2546 physician-years ofcare. Patient complaints (adjusted forclinical activity) related to: Risk management file openings File openings with expenditures LawsuitsHickson, JAMA, 2002.
Communication Issues with Patients/Families Seen inMalpractice Claims Patient contingency plan Patient diagnosis Patient severity of illness Medication plan Radiologic result Procedure or test result Laboratory result Specialist recommendations Need to see specialist or primary care physicianHumphrey, J Pat Saf, 2021.
Partnering With the PatientStrategies for involving patients in their care Include patients in bedside rounds Conduct handoffs at the patient’s bedside Provide patients with tools for communicating with their care team Involve patients in key committees Actively enlist patient participationAHA TeamSTEPPS TEAM STRUCTURE Module.
Patient and Family Responsibilities Provide accurate patient information Comply with the prescribed plan of care (e.g., schedule and attend appointments asdirected) Ask questions and/or voice any concerns regarding the plan of care Monitor and report changes in the patient’s condition Manage family members Follow instructions of the clinical teamAHA TeamSTEPPS TEAM STRUCTURE Module.
Agenda Malpractice and risk reductionMalpractice data & the role of teamworkTeamwork, the patient & malpracticeEngaging leadership & insurers
Polling Question #4Which is the best approach to get hospital leadership buy-in for patientsafety programs?a. Present malpractice data to the patient safety committee of the hospitalboardb. Use a well thought out business plan with a defined ROI for all patientsafety expensesc. Have the CFO attend all root cause analysesd. Be sure the hospital performs well on all publicly reported hospital metricse. Create a dedicated hospital committee to ensure top HCAHPSperformance
How to Measure – KirkpatrickLevel IV: ResultsLevel III: BehaviorLevel II: LearningLevel I: ReactionsMULTILEVELAPPROACH(Organizational results)(Transfer to the job)(Think, Do, Feel)(Like it and Useful)AHA TeamSTEPPS MEASUREMENT Module.
Level IV: Results Patient Outcome Measureso Examples: Complication rates, infection rates, measurable medication errors, and patientperceptions of care and satisfaction with their care Clinical Process Measureso Examples: Length of patient wait time, time to intubate, medication administration delays,compliance with preventive screenings, number of misdiagnoses, number of structuredhandoffs used Malpractice Data!AHA TeamSTEPPS MEASUREMENT Module.
Retained Surgical Items Prevention - Counting, Teamwork, Radiography, New technology Risk Reduction Strategies to Decrease the Incidence of RetainedSurgical Itemso 997,237 Operative Procedureso TeamSTEPPS training and RF technology interventionso RSI decreased - 11.66 to 5.80 events per 100,000 operationso RSI involving RF detectable items decreased - 5.21 to 1.35 events per 100,000operationso Malpractice claims related to sponges and lap pads decreased - 1.6/year to .67/yearFeldman, Mt Sinai J Med, 2011.Kaplan, JACS, 2022.
Value of Malpractice Data Qualitative details “Tip of the iceberg”Combining with other data sourceso Adverse eventso Patient/staff complaintso Outside data bases – NSQIP, STS
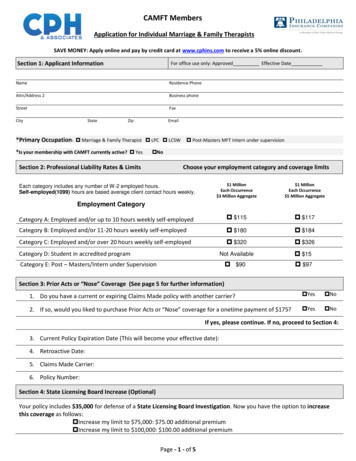
Using Malpractice Data to Drive Safety Determine your professional liability insurance carriero Individual physicianso Hospital Understand state-based lawso Charitable immunityo Caps on non-economic damageso Pricing of premiums Get the data!o Your carriero National sources – Candello (CBS), MPLA (DSP)
Agenda Malpractice and risk reductionMalpractice data & the role of teamworkTeamwork, the patient & malpracticeEngaging leadership & insurers
Key Takeaways1. Malpractice data can be useful as a tool to identify events and theassociated costs can be a driver for investment in patient safety efforts.2. Poor teamwork can be identified in malpractice analyses along with itsspecific impact on payment.3. Risk managers and patient safety leaders in healthcare institutions shouldunderstand the nature of their malpractice program to help them reducethe costs incurred by poor teamwork and communication.
Questions? Stay in Touch!www.aha.org/teamtrainingEmail: teamtraining@aha.org Phone: (312) 422-2609
2. Poor teamwork can be identified in malpractice analyses along with its specific impact on payment. 3. Risk managers and patient safety leaders in healthcare institutions should understand the nature of their malpractice program to help them reduce the costs incurred by poor teamwork and communication. Key Takeaways