Transcription
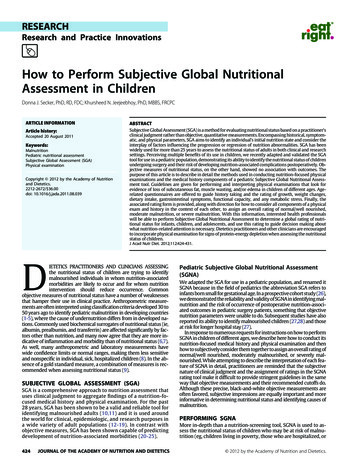
RESEARCHResearch and Practice InnovationsHow to Perform Subjective Global NutritionalAssessment in ChildrenDonna J. Secker, PhD, RD, FDC; Khursheed N. Jeejeebhoy, PhD, MBBS, FRCPCARTICLE INFORMATIONABSTRACTArticle history:Subjective Global Assessment (SGA) is a method for evaluating nutritional status based on a practitioner’sclinical judgment rather than objective, quantitative measurements. Encompassing historical, symptomatic, and physical parameters, SGA aims to identify an individual’s initial nutrition state and consider theinterplay of factors influencing the progression or regression of nutrition abnormalities. SGA has beenwidely used for more than 25 years to assess the nutritional status of adults in both clinical and researchsettings. Perceiving multiple benefits of its use in children, we recently adapted and validated the SGAtool for use in a pediatric population, demonstrating its ability to identify the nutritional status of childrenundergoing surgery and their risk of developing nutrition-associated complications postoperatively. Objective measures of nutritional status, on the other hand, showed no association with outcomes. Thepurpose of this article is to describe in detail the methods used in conducting nutrition-focused physicalexaminations and the medical history components of a pediatric Subjective Global Nutritional Assessment tool. Guidelines are given for performing and interpreting physical examinations that look forevidence of loss of subcutaneous fat, muscle wasting, and/or edema in children of different ages. Agerelated questionnaires are offered to guide history taking and the rating of growth, weight changes,dietary intake, gastrointestinal symptoms, functional capacity, and any metabolic stress. Finally, theassociated rating form is provided, along with direction for how to consider all components of a physicalexam and history in the context of each other, to assign an overall rating of normal/well nourished,moderate malnutrition, or severe malnutrition. With this information, interested health professionalswill be able to perform Subjective Global Nutritional Assessment to determine a global rating of nutritional status for infants, children, and adolescents, and use this rating to guide decision making aboutwhat nutrition-related attention is necessary. Dietetics practitioners and other clinicians are encouragedto incorporate physical examination for signs of protein-energy depletion when assessing the nutritionalstatus of children.J Acad Nutr Diet. 2012;112:424-431.Accepted 20 August 2011Keywords:MalnutritionPediatric nutritional assessmentSubjective Global Assessment (SGA)Physical examinationCopyright 2012 by the Academy of Nutritionand Dietetics.2212-2672/ 36.00doi: 10.1016/j.jada.2011.08.039DIETETICS PRACTITIONERS AND CLINICIANS ASSESSINGthe nutritional status of children are trying to identifymalnourished individuals in whom nutrition-associatedmorbidities are likely to occur and for whom nutritionintervention should reduce occurrence. Commonobjective measures of nutritional status have a number of weaknessesthat hamper their use in clinical practice. Anthropometric measurements are often interpreted using classification criteria developed 30 to50 years ago to identify pediatric malnutrition in developing countries(1-5), where the cause of undernutrition differs from in developed nations. Commonly used biochemical surrogates of nutritional status (ie,albumin, prealbumin, and transferrin) are affected significantly by factors other than nutrition, and many now agree that they are more indicative of inflammation and morbidity than of nutritional status (6,7).As well, many anthropometric and laboratory measurements havewide confidence limits or normal ranges, making them less sensitiveand nonspecific in individual, sick, hospitalized children (8). In the absence of a gold standard measure, a combination of measures is recommended when assessing nutritional status (9).SUBJECTIVE GLOBAL ASSESSMENT (SGA)SGA is a comprehensive approach to nutrition assessment thatuses clinical judgment to aggregate findings of a nutrition-focused medical history and physical examination. For the past28 years, SGA has been shown to be a valid and reliable tool foridentifying malnourished adults (10,11) and it is used aroundthe world for clinical, epidemiologic, and research purposes ina wide variety of adult populations (12-19). In contrast withobjective measures, SGA has been shown capable of predictingdevelopment of nutrition-associated morbidities (20-25).424JOURNAL OF THE ACADEMY OF NUTRITION AND DIETETICSPediatric Subjective Global Nutritional Assessment(SGNA)We adapted the SGA for use in a pediatric population, and renamed itSGNA because in the field of pediatrics the abbreviation SGA refers toinfants born small for gestational age. In a prospective cohort study (26),we demonstrated the reliability and validity of SGNA in identifying malnutrition and the risk of occurrence of postoperative nutrition-associated outcomes in pediatric surgery patients, something that objectivenutrition parameters were unable to do. Subsequent studies have alsoreported its ability to identify malnourished children (27,28) and thoseat risk for longer hospital stay (27).In response to numerous requests for instructions on how to performSGNA in children of different ages, we describe here how to conduct itsnutrition-focused medical history and physical examination and thenhow to subjectively consider them together to assign an overall rating ofnormal/well nourished, moderately malnourished, or severely malnourished. While attempting to describe the interpretation of each feature of SGNA in detail, practitioners are reminded that the subjectivenature of clinical judgment and the assignment of ratings in the SGNArating tool make it difficult to provide stringent guidelines in the sameway that objective measurements and their recommended cutoffs do.Although these precise, black-and-white objective measurements areoften favored, subjective impressions are equally important and moreinformative in determining nutritional status and identifying causes ofmalnutrition.PERFORMING SGNAMore in-depth than a nutrition-screening tool, SGNA is used to assess the nutritional status of children who may be at risk of malnutrition (eg, children living in poverty, those who are hospitalized, or 2012 by the Academy of Nutrition and Dietetics.
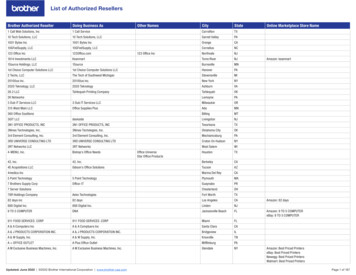
RESEARCHthose with neurocognitive disabilities or chronic illness/disease). Although effective in evaluating baseline nutritional status, it was notdesigned to be a responsive assessment tool (ie, one that measuresacute change). SGNA’s slowly changing parameters are an insensitive measure of acute nutritional manipulation, and after 7 to 10days of optimal nutrition support an SGNA rating would not be expected to change.SGNA considers seven specific features of a nutrition-focusedmedical history and three features of a nutrition-focused physicalexamination for signs of inadequate energy and/or protein intake.An age-specific questionnaire (Figures 1 and 2, available online atwww.andjrnl.org) can be used to guide the medical-nutrition interview of children and/or caregivers. Historical measurements of length/height and weight are obtained from medical records and/or caregiversand plotted on age- and sex-appropriate growth charts. Finally, a nutrition-focused physical examination is performed. Considering the presence or absence of the historical features and physical signs associatedwith malnutrition, a child’s nutritional status is assigned a global ratingof normal/well nourished, moderately malnourished, or severely malnourished according to guidelines provided on the SGNA rating form(see Figure 3).Nutrition-Focused Medical HistoryLinear Growth. A rating of normal, moderate, or severe is assigned forthe child’s height-for-age percentile, appropriateness of the child’sheight relative to their mid-parental height* (29), and serial growth. Weconsider length or height just below the third percentile as suspicious ofabnormal growth and rate it as moderate, whereas measures far belowthe third percentile are rated severe. Direction of serial measurementson the growth curves is also important; a rapid or sharp downwardmovement on the curves is considered severe whereas a gradual movement downward is rated moderate. With the exception of the first 2years of life, and during puberty, when shifting of percentiles is normal(30), crossing percentiles or channels downward is considered a potential sign of a nutrition-related growth disturbance. It is normal forhealthy infants to shift one to two major centiles for both length andweight, especially during the first 6 months of life. These shifts typicallyoccur toward, rather than away from, the 50th percentile (ie, regressiontoward the mean); a rapid or sharp decline or a growth pattern thatremains flat suggests a problem.Weight Relative to Length/Height. After plotting length/heightand weight on the growth chart a child’s ideal body weight (IBW)†and percent of ideal weight (% IBW)‡ are calculated. % IBW is rated as 90% IBW normal/well nourished, 75% to 90% IBW moderatemalnutrition, and 75% IBW severe malnutrition (31).*To determine mid-parental height for girls, subtract 13cm from the father’s height and average with the mother’sheight. To determine mid-parental height for boys, add 13cm to the mother’s height and average with the father’sheight. Thirteen centimeters is the average difference inheight between women and men. For both girls and boys,8.5 cm on either side of this calculated value (target height)represents the 3rd to 97th percentiles for anticipated adultheight (29).†Ideal body weight refers to the weight that is at the samepercentile for age as the child’s length/height. For childrenwhose length/height is less than the third percentile, determine ideal body weight by first estimating height age (ageat which their height would be at the 50th percentile) andthen identifying the weight at the 50th percentile for thatheight-age.‡Percent of ideal body weight is determined by the equation (actual body weight divided by ideal bodyweight) 100%.March 2012 Volume 112 Number 3Changes in Body Weight. Unintentional weight loss is a goodprognosticator of clinical outcome. In pediatrics, failure to gainweight is also a concern. Serial weight measurements are ratednormal if they are following the growth curves, moderate if theyare low but moving upward on the curves, and severe if shiftingdownward on the curves. Acute weight loss in children is oftendue to changes in hydration status or onset of acute illness. Therefore, the pattern of weight change (eg, amount, speed, and duration) is also important (11). A large, rapid weight loss (eg, ⱖ5% inless than 1 month is more concerning than a small, steady loss (eg,2% across 3 months). Percent weight loss§ between 5% and 10% isconsidered moderate and sustained loss 10% is considered severe. A separate rating is also made based on any change duringthe past 2 weeks (continued loss, stable weight, or weight gain).The normal/well-nourished rating or an upgraded rating could bebased on improvement in status (32). Accumulation or loss offluid is not regarded as real change in body mass.Adequacy of Dietary Intake. During assessment, ask about thechild’s appetite, frequency of intake, foods eaten, and feeding/eating problems, or dietary restrictions that interfere with theability to meet nutrition requirements. Subjectively comparethe child’s dietary intake to recommended intakes for age andlevel of activity. Rate inadequate intake as hypocaloric (moderate) or starvation (severe). Assign a rating for any changes infood intake compared to the child’s usual intake (eg, decreasing, same, or improving), as well as the duration of the change(eg, days, weeks, or months) (32). Low intakes lasting for morethan 2 weeks and that are continuing or worsening place achild at higher risk of malnutrition. Low, but improving, intakes could be rated as moderate.Persistent Gastrointestinal (GI) Symptoms. This feature helpsclarify the degree to which a child’s ability to take and tolerate anormal diet is restricted. Inquire about the presence, severity, andduration of GI symptoms such as anorexia, nausea, abdominalpain, vomiting/gastroesophageal reflux, diarrhea, and constipation. The more severe the symptoms, the poorer the SGNA rating.GI symptoms are considered severe if they have been present onan almost daily basis for at least 2 weeks. Short-term or intermittent symptoms, such as diarrhea or loss of appetite for 2 to 3 days,are considered less significant.Functional Impairment. Muscle function is an early index of nutrition changes and of complication risk in sick persons (33,34).Functional impairment helps clarify whether a child is simply anormally thin individual with lots of energy, or whether there aresigns that recent weight loss due to low energy intake is affectinghis or her ability to perform. The magnitude of the effect of malnutrition is greater for an individual who has lost weight andbecome less ambulatory (11). Consider whether decreased foodintake has been severe enough to lead to compromised physicalfunction and altered daily activities. View this information compared to energy and activity levels that are usual for that child, notsimilar-aged children in general. Give separate ratings to severityof the dysfunction, and any change during the past 2 weeks. If theimpairment is worsening, assign the severe category. Rate nochange as moderate, and improvement as normal/well nourished.Only note changes in function related to nutritional status (11).Metabolic Stress. Evaluate the metabolic demands of a child’sunderlying illness and any acute stresses that may alter thosemetabolic demands and increase energy and/or protein requirements. Examples of severe- and moderate-stress conditions areshown in Figure 4.§Percent weight loss is determined by the equation (usualweight current weight)/usual weight.JOURNAL OF THE ACADEMY OF NUTRITION AND DIETETICS425
RESEARCHFigure 3. Pediatric Subjective Global Nutritional Assessment (SGNA) rating form. (continued on next page)426JOURNAL OF THE ACADEMY OF NUTRITION AND DIETETICSMarch 2012 Volume 112 Number 3
RESEARCHFigure 3. Pediatric Subjective Global Nutritional Assessment (SGNA) rating form. (continued)Nutrition-Focused Physical ExaminationA physical exam helps corroborate information obtained in themedical-nutrition history by providing supportive evidence ofweight loss or decreased functional capacity. Look for signs ofloss of fat stores, muscle wasting, and edema (Figure 5) (35),following a logical and sequential process using a head-to-toeapproach. Because it is difficult to determine fat vs muscle lossduring the early years of life, physical examination in infantsand toddlers assesses fat and muscle stores together as generalwasting.Loss of Subcutaneous Fat. Fat content in the body alters withage, increasing rapidly after birth from 14% to 15% of body weightto a peak of 25% to 26% by age 6 months (36). After age 6 months,fat content begins to decrease, reaching a minimum of 13% at age7 years in boys and 16% at age 6 years in girls, followed by anincrease to 14% in boys and 19% in girls around the age of 10 years(36). Infants are therefore physiologically fat compared to chilMarch 2012 Volume 112 Number 3dren and adolescents, and they have a higher proportion of protein in viscera than somatic tissue.Examine the child’s face, arms, chest, and buttocks for loss ofsubcutaneous fat. Look for clearly defined, bony, or muscular outlines because the outline of muscles is easily observed when thereis loss of fat. Hollow facial cheeks, little space between the fingerswhen pinching fat stores over the biceps and triceps, depressionsbetween the ribs, and flat or baggy buttocks are signs of loss ofsubcutaneous fat. Evaluation is not meant to be an exact measurement, but to provide a subjective impression of fat stores andlosses that may have resulted from inadequate nutrition (11).Muscle Wasting. Muscle wasting is defined as loss of bulk andtone. Examine the child’s temple, clavicle, shoulder, scapula,thigh, knee, and calf for signs of muscle wasting. Prominent orprotruding bone structure at the clavicle, shoulder, scapula, andknee sites, and flat or hollow areas in the upper or lower legs,suggest muscle wasting. Ask whether this is the usual amount ofJOURNAL OF THE ACADEMY OF NUTRITION AND DIETETICS427
RESEARCHFigure 4. Examples of moderate or severe metabolic stress conditions that should be considered when using the Subjective GlobalNutrition Assessment tool for pediatric populations.muscle mass for the child or whether there has been a recentchange. Consider if low muscle mass is due to neuropathy or myopathy rather than nutritional restriction.Edema. Test for dependent edema by applying firm pressure withthe thumb into the skin over the bony surface of the distal anteriorsurface of the foot, or over the sacrum (for infants and bedriddenchildren) for 5 seconds and observing the depth of the depressionand whether it persists after lifting the thumb. Edema known tobe related to a child’s illness (eg, oligoanuria, nephrotic syndrome,liver disease, or congestive heart failure) should not be rated aspotential malnutrition. If observed, assess weight change andedema together to determine whether tissue wasting is hidden byfluid retention.Assigning the Overall SGNA RatingDetermine a child’s nutritional status by first rating each of thecomponents of the seven features of the medical-nutrition history as well as the physical examination as normal, moderate, orsevere using the SGNA Rating Form (Figure 3). The overall SGNArating is subjective and is not based on a numerical scoring system. Examine the rating form to obtain a general feel for thechild’s status. More checkmarks on the right-hand side of theform suggest the child is likely to be malnourished. If most of thecheckmarks are on the left-hand side, the child is likely to benormal/well nourished. It is inappropriate to simply add thenumber of normal, moderate, or severe ratings to arrive at theoverall classification. Give the most consideration to unintentional changes in body weight and serial growth, adequacy ofdietary intake, and physical signs of loss of fat or muscle mass.Use the other components to confirm the child’s or caregiver’sself-reports and support or strengthen these ratings.Consider also the progression of the child’s nutritional status inrelation to his or her usual. SGNA is based on the hypothesis thatrestoration of food intake to optimal levels can rapidly reduce therisks associated with malnutrition (37,38), even though an individual is still wasted and underweight. Therefore, if the child hasrecently gained weight, and other indicators such as appetiteshow improvement, the child may be assigned the normal/wellnourished rating despite previous loss of fat and muscle that remains physically noticeable. On the other hand, children withobesity could be moderately or severely malnourished basedupon a poor medical history and signs of muscle loss.The severely malnourished rating is generally given when achild has physical signs of malnutrition in the presence of a medical history suggestive of risk (eg, continuing weight loss 10%and a decline in dietary intake, with or without poor lineargrowth) (32). GI symptoms and functional impairments usually428JOURNAL OF THE ACADEMY OF NUTRITION AND DIETETICSexist in these children. Severely malnourished children rank inthe moderate to severe category in most features on the SGNAform, and show little or no sign of improvement during the previous month.A child is assigned the moderately malnourished rating whenrecent weight loss is 10% (eg, 5% in 1 month; 7.5% in 3 months)with no subsequent gain and there is a reduction in dietary intakeand mild or no loss of subcutaneous fat or muscle (32). Thesechildren may or may not have functional impairments or GIsymptoms. The child may be experiencing a downward trend butstarted with reasonably good nutritional status and has the potential to progress to a severely malnourished state. The moderate rating is expected to be the most ambiguous of all SGNA classifications. These children may have rankings in all threecategories.The normal/well nourished category is assigned if the child hasfew or no physical signs of malnutrition, weight loss or growthfailure, dietary difficulties, nutrition-related functional impairments, or persistent GI symptoms that might predispose to malnutrition.LimitationsSGNA was designed to identify undernourished children and, assuch, it does not differentiate children with adiposity from wellnourished children. Children with overweight or obesity could bemoderately or severely malnourished based on a current poor medical history and signs of muscle loss. Physical detection of loss of fatand muscle mass in these children is difficult. Although the usefulness of body mass index in identifying pediatric overweight and obesity is well established, accurate body mass index cutoffs for determining undernutrition that is associated with adverse outcomeshave not been well established. When that occurs, research to determine whether body mass index better replaces percent ideal bodyweight in SGNA will be warranted. Most of the older children andadolescents declined assessment of the fat mass in their buttocks.For future use, we suggest that this site be used only for infants andtoddlers. In our original study (26), moderate edema was identifiedin only 11 out of 175 (6%) children and severe edema not at all,numbers too small to assess the importance of this variable in theoverall SGNA rating. Given limitations of serum proteins as markersof nutritional status, we suggest that inclusion of edema in physicalexams be considered exclusively for populations where its frequency is high in association with their underlying illness. We alsosuggest that it be used solely to evaluate whether a child’s measuredweight is a true “dry” or euvolemic weight, rather than using it as asign of inadequate intake.March 2012 Volume 112 Number 3
RESEARCHFigure 5. Physical examination findings: What to look for when applying Subjective Global Nutritional Assessment in a pediatricpopulation. Adapted with permission from reference (35).March 2012 Volume 112 Number 3JOURNAL OF THE ACADEMY OF NUTRITION AND DIETETICS429
RESEARCHparison of clinical judgment and objective measurements. N Engl JMed. 1982;306(16):969-972.CONCLUSIONSSGNA is a comprehensive, organized representation of the thoughtprocess a clinician should use in assessing a child’s nutritional status.Its simple, noninvasive nature moves an assessor away from a fixation on objective measures and numerical precision and back to thechild. It allows one to capture the dynamic nature of malnutritionthrough consideration of subtle patterns of change in variables, suchas the direction and duration of weight changes rather than absoluteamounts. Many children are thin or have lost weight, and this initself does not constitute malnutrition. Objective measurements areunable to discern the difference. SGNA outperforms objective measures and has advantages over them that merit its use.Practitioners who work with pediatric populations should incorporate clinical judgment into their nutrition assessments and relyless on black-and-white objective measures. Further developmentand testing of SGNA and its ability to portray adverse events in otherpediatric populations, including those with overnutrition, is warranted.Physical examination as a component of pediatric nutrition assessment is rarely utilized; however, it can be quite revealing.Physical signs of wasting were one of the variables that had thehighest correlation with the overall SGNA rating for children of allages in our original study. This is consistent with studies of SGA inadults (11,39,40). Dialog during a physical exam can provide additional information on physical activity and functional capacitynot revealed while taking a medical-nutrition history. Anotherimportant benefit is the opportunity to assess a child withoutbulky clothes that can effectively hide under- or overnutrition.Some children have a deceptively normal or mildly low weightfor-height, but on examination have visible severe wasting in thepresence of organomegaly or edema. In situations such as these,dimensionless assessment can be more useful than exact weight.Using a critical eye and feel is as informative as skinfold measurement when assessing fat and muscle mass in children.Dietetics practitioners are less familiar than physicians andnurses with this physical, hands-on aspect of care and are, therefore, less prepared to get a complete picture of the patient (41).We strongly advocate for inclusion of a nutrition-focused physicalexamination in pediatric nutrition assessments performed by dietetics practitioners as well as physicians and nurses. We alsorecommend that physical examination skills be incorporated intothe core curriculum of dietetics students to facilitate this clinicalpractice.References1.Gomez F, Galvan RR, Cravioto J, Frenk S. Malnutrition in infancy andchildhood, with special reference to kwashiorkor. Adv Pediatr. 1955;7:131-169.2.Jelliffe D. The Assessment of the Nutrition Status of the Community (withSpecial Reference to Field Surveys in Developing Regions of the World).Geneva, Switzerland: World Health Organization; 1966. Monograph53.3.Waterlow JC. Classification and definition of protein-calorie malnutrition. BMJ. 1972;3(5826):566-569.4.Waterlow JC. Note on the assessment and classification of proteinenergy malnutrition in children. Lancet. 1973;2(7820):87-89.5.McLaren DS, Read WWC. Classification of nutritional status in earlychildhood. Lancet. 1972;2(7769):146-147.6.Fuhrman M, Charney P, Mueller C. Hepatic proteins and nutritionassessment. J Am Diet Assoc. 2004;104(8):1258-1264.7.Banh L. Serum proteins as markers of nutrition: What are we treating? Pract Gastroenterol. 2006;Series 43:46-64.8.Tonglet R, Lembo E, Zihindula P, Wodon A, Dramix M, Hennart P.How useful are anthropometric, clinical and dietary measurements of nutritional status as predictors of morbidity of youngchildren in central Africa? Trop Med Int Health. 1999;4(2):120-130.9.American Society for Parenteral and Enteral Nutrition Board of Directorsand Clinical Practice Committee. Definition of terms, style, and conventions used in A.S.P.E.N. Board of Directors–approved documents. http://www.nutritioncare.org. Accessed April 13, 2011.10.430Baker JP, Detsky AS, Wesson DE, et al. Nutritional assessment: A com-JOURNAL OF THE ACADEMY OF NUTRITION AND DIETETICS11.Detsky AS, McLaughlin JR, Baker JP, et al. What is subjective globalassessment of nutritional status? JPEN J Parenter Enteral Nutr. 1987;11(1):8-13.12.Gupta D, Lammersfeld C, Vashi P, Burrows J, Lis C, Grutsch J. Prognostic significance of Subjective Global Assessment (SGA) in advancedcolorectal cancer. Eur J Clin Nutr. 2005;59(1):35-40.13.Shirodkar M, Mohandas K. Subjective global assessment: A simpleand reliable screening tool for malnutrition among Indians. Indian JGastroenterol. 2005;24(6):246-250.14.Pham N, Cox-Reijven P, Greve J, Soeters P. Application of subjectiveglobal assessment as a screening tool for malnutrition in surgicalpatients in Vietnam. Clin Nutr. 2006;25(1):102-108.15.Steiber A, Leon JB, Secker D, et al. Multicenter study of the validity andreliability of Subjective Global Assessment in the hemodialysis population. J Ren Nutr. 2007;17(5):336-343.16.Bauer J, Capra S, Ferguson M. Use of the scored patient-generatedsubjective global assessment (PG-SGA) as a nutrition assessmenttool in patients with cancer. Eur J Clin Nutr. 2002;56(8):779-785.17.Waitzberg D, Caiaffa W, Correia I. Hospital malnutrition: The Brazilian National Survey (IBRANUTRI): A study of 4000 patients. Nutrition.2001;17(7/8):573-580.18.Makhija S, Baker J. The Subjective Global Assessment: A review of itsuse in clinical practice. Nutr Clin Pract. 2008;23(4):405-409.19.Sheean P, Peterson S, Gurka D, Braunschweig C. Nutrition assessment:the reproducibility of subjective global assessment in patients requiringmechanical ventilation. Eur J Clin Nutr. 2010;64(11):1358-1364.20.Baker JP, Detsky AS, Whitwell J, Langer B, Jeejeebhoy KN. A comparison of the predictive value of nutritional assessment techniques. HumNutr Clin Nutr. 1982;36(3):233-241.21.Detsky AS, Baker JP, O’Rourke K, et al. Predicting nutrition-associatedcomplications for patients undergoing gastrointestinal surgery. JPENJ Parenter Enteral Nutr. 1987;11(5):440-446.22.The Veterans Affairs Total Parenteral Nutrition Cooperative StudyGroup. Perioperative total parenteral nutrition in surgical patients. NEngl J Med. 1991;325(8):525-532.23.Wakahara T, Shiraki M, Murase K, et al. Nutritional screening withSubjective Global Assessment predicts hospital stay in patients withdigestive diseases. Nutrition. 2007;23(9):634-639.24.Norman K, Schutz T, Kemps M, Lubke H, Lochs H, Pirlich M. The Subjective Global Assessment reliably identifies malnutrition-relatedmuscle dysfunction. Clin Nutr. 2005;24(1):143-150.25.Martineau J, Bauer J, Isenring E, Cohen S. Malnutrition determined by thepatient-generated subjective global assessment is associated with pooroutcomes in acute stroke patients. Clin Nutr. 2005;24(6):1073-1077.26.Secker D, Jeejeebhoy K. Subjective Global Nutritional Assessment forchildren. Am J Clin Nutr.2007;85(4):1083-1089.27.Mahdavi AM, Safaiyan A, Ostadrahimi A. Subjective vs objective nutritional assessment study in children: A cross-sectional study in thenorthwest of Iran. Nutr Res. 2009;29(4):269-274.28.Gerasimidis K, Keane O, Macleod I, Flynn DM, Wright CM. A fourstage evaluation of the Paediatric Yorkhill Malnutrition Score in atertiary paediatric hospital and a district general hospital. Br J Nutr.2010;104(5):751-756.29.Tanne
weight loss or decreased functional capacity. Look for signs of loss of fat stores, muscle wasting, and edema (Figure 5)(35), following a logical and sequential process using a head-to-toe approach. Because it is difficult to determine fat vs muscle loss during the early years of life, physical examination in infants