Transcription
9/16/2016Pregnancy and Heart Disease for theGeneralistSharon L. Roble, MD, FACC1DISCLOSURES I have no disclosures relevant to today’s talk21
9/16/2016Cardiovascular Effects of Pregnancy Anatomic Ventricular muscle mass increases (1st trimester) End-diastolic volume increases (2nd and 3rd trimester) End-systolic volume unchanged Physiologic Plasma Volume Blood Volume3Plasma Volume 45% increase abovenon-pregnant values 1200 to 1600 mL intotal Unclear mechanism Possible initiated bynitric oxide–mediatedvasodilation Stimulating reninangiotensinaldosterone system Possibly adaptive inreducinghemodynamicinstability after bloodloss2
9/16/2016Blood Volume Plasma volumeincreasesdisproportionately tored blood cell mass Mild net anemia Maximal in themiddle of the thirdtrimester Possibly adaptive bydecreasing viscosity Countering increasedthrombotic risk Improved intervillousperfusionIncreased Cardiac OutputFrom Creasy & Resnik’s Maternal –Fetal Medicine: Figure 7-1 Adapted from Robson SC, Hunter S,Boys RJ, et al: Serial study of factors influencing changes in cardiac output during humanpregnancy. Am J Physiol 256:H1060, 1989.3
9/16/2016Vascular changes General softening of vascular collagenHypertrophy of the smooth muscle componentNet increased complianceFurther accentuated by vasodilator effectsprogesterone and prostaglandinHemodynamic ChangesDuring Normal PregnancyParameterBlood volumeCardiac volumeStroke volumeHeart rateSystolic BPDiastolic BPPulse pressureSVR1st Trimester2nd Trimester3rd Trimester to to or or 4
9/16/2016How do we risk stratify patients? No large randomized studiesNo standardized, evidence-based guidelinesCARPREG scoreZAHARA scoringWHO classificationLow Maternal/Fetal Risk Asymptomatic Aortic Stenosis Low mean gradient less than 25 mmHg Valve area greater than 1.5 cm2 Normal LV systolic function (EF 50%) Aortic Regurgitation NYHA functional class I or II Normal LV systolic function Mitral Regurgitation NYHA functional class I or II Normal LV systolic function5
9/16/2016Low Maternal/Fetal Risk Mitral Valve Prolapse Up to mild to moderate MR Normal LV systolic function Mild mitral stenosis MVA greater than 1.5 cm2 Mean gradient less than 5 mmHg Without severe pulmonary hypertension Mild to moderate pulmonary valve stenosisHigh Maternal/Fetal Risk Severe AS with or without symptoms Aortic Regurgitation NYHA functional class III-IV symptoms Mitral Stenosis NYHA functional class II-IV symptoms Mitral Regurgitation NYHA functional class III-IV symptoms6
9/16/2016High Maternal/Fetal Risk Aortic and/or mitral valve disease Resulting in severe pulmonary hypertension ( 75% systemic) Severe LV dysfunction (EF 40%) Mechanical prosthetic valve requiring anticoagulation Marfan syndrome with or without AR Pulmonary hypertension Cyanotic heart diseaseMarfan’s Collagen and vascular changes in pregnancy Increased risk for dissection for aorta 4-4.5 cm indiameter Continue beta blockers Surveillance echocardiography imaging every 6-8weeks Invasive arterial pressure monitoring and assistedsecond stage7
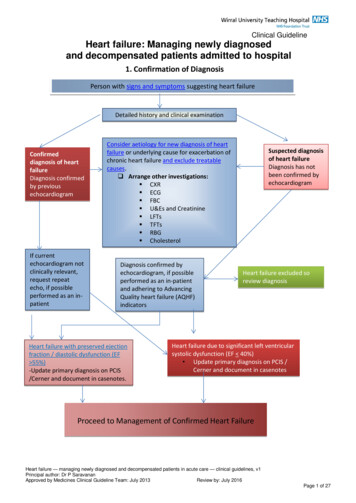
9/16/2016CARPREG Study Prospective study of 562 pregnant women with heartdisease in Canada between 1994-1999. 546 women underwent 599 pregnancies. Live birth rate-98% 27% C-section 96% for obstetrical reasonsCARPREG – Four Risk Factors Prior cardiac event Heart failure TIA or CVA Arrhythmia Baseline NYHA class III-IV or cyanosis Left heart obstruction MV area 2 cm2 AV area 1.5 cm2 Peak LVOT gradient 30 mmHg Myocardial dysfunction Ejection fraction 40% Hypertrophic cardiomyopathy Restrictive cardiomyopathy8
9/16/2016CARPREG Risk IndexSiu, S. C. et al. Circulation 2001;104:515-521ZAHARA I Study Retrospective study of1802 patients withcongenital heartdisease Cardiac complications Arrhythmia Heart failure Thrombo-embolicevents/MI/CVA Endocarditis Obstetric complications Pregnancy inducedhypertension Preeclampsia/Eclampsia/HELLP Premature labor Post-partumhemorrhage NeonatalComplications Premature delivery SGA Offspring mortality9
9/16/2016ZAHARA I Results 1302 completed ical24%Neonatal25%--Drenthen W et al. Eur Heart J 2010;31:2124-2132ZAHARA I ScoringRisk FactorPointsHistory of arrhythmias1.50Cardiac medication before pregnancy1.50NYHA class prior to pregnancy II0.75LHO (PG 50 mmHg or AVA 1.0 cm2)2.50Systemic AV valve regurgitation (moderate/severe)0.75Pulmonary AV valve regurgitation (moderate/severe)0.75Mechanical valve prosthesis4.25Cyanotic heart disease (corrected/uncorrected)1.00TOTAL POSSIBLE13.00--Drenthen W et al. Eur Heart J 2010;31:2124-213210
9/16/2016ZAHARA IDrenthen W et al. Eur Heart J 2010;31:2124-2132Published on behalf of the European Society of Cardiology. All rights reserved. The Author2010. For permissions please email: journals.permissions@oxfordjournals.orgZAHARA II Prospective study involving women with structuralheart disease 2008-201011
9/16/2016WHO Classification Based on underlying diagnosis in additionto any other co-morbidity It includes contra-indications for pregnancynot found in other scoring systems Recommended by European Society ofCardiology (ESC)12
9/16/2016WHO ClassificationWHO I: Low-risk Cardiology followup may be limitedto 1-2 visitsthroughoutpregnancy13
9/16/2016WHO II: Low/Moderate Risk Follow-up once atrimesterWHO III: High Risk Monthly-tobimonthlycardiology and OBfollow-up14
9/16/2016WHO IV: Pregnancy Contra-indicatedImaging in Pregnancy EchoNo Radiation Exposure; Tests of ChoiceMRIX-rayCTNuclear ImagingAngiography3015
9/16/2016313216
9/16/2016Iodizing Radiation Majority of fetal exposure from cardiothoracicimaging is from scatter (Compton) radiation Sheilding fetus is of little value33--Colletti P et al. “Cardiovascular Imaging of the Pregnant Patient”. AJR 2013;200:515-521.Radionuclide Exposure--Colletti P et al. “Cardiovascular Imaging of the Pregnant Patient”. AJR2013;200: 515-521.3417
9/16/2016Radiation Exposure--Colletti P et al. “Cardiovascular Imaging of the Pregnant Patient”. AJR 2013;200: 515-521.35Contrast Agents Iodinated contrast Readily cross placenta Pregnancy Class B Use only if necessary Gadolinium-based contrast Easily cross placentaPregnancy Class CAvoid if possibleEnters breast milk3618
9/16/2016FDA Drug Classification for Pregnancy Class A: Controlled clinical studies in humans showsafety Class B: Human data reassuring (animal positive),animal studies show no risk. Dobutamine Normal saline Class C: Human data lacking, animal studies positiveor not done (67%) Adenosine Echo contrast agents (Definity, Optison)37 Class D: Human data show risk, benefit mayoutweigh risk. Class X: Animal or human data positive forunacceptable risk.Agitated saline (Bubble) studies andPregnancy There is currently no data looking at the safety ofbubble studies in pregnant women Generally felt as safe based on concept that normalsaline is a category B drug to use in pregnancy(considered safe) Case reports of CVA/TIA in patients undergoingbubble studies Would wait until after first trimester if feasible3819
9/16/2016Residual Intracardiac Shunting Theoretical risk of paradoxical emboli Aspirin 81 mg daily IV filtersReferences Colletti P et al. “Cardiovascular Imaging of thePregnant Patient”. American Journal ofRoentgenology. 2013;200: 515-521. Committee on Obstetric Practice. “ACOG CommitteeOpinion No 299: Guidelines for Diagnostic ImagingDuring Pregnancy”. Obestet Gynecol 2004; 104:647-51.4020
9/16/2016THANK YOU4121
End-diastolic volume increases (2nd and 3rd trimester) End-systolic volume unchanged Physiologic Plasma Volume Blood Volume 3 Plasma Volume . Cyanotic heart disease (corrected/uncorrected) 1.00 TOTAL POSSIBLE 13.00--Drenthen W et al. Eur Heart J 2010;31:2124-2132. 9/16/2016 11