Transcription
A publication of theNational KidneyFoundationInsidethis issue:Vol. 16, No. 1Winter 2007QUALITY IN DIALYSISDefining whatquality means toyou can lead toimprovedoutcomes.Improving Quality of Care in DialysisBy Adeera Levin, MD, FACP—Page 5There areYOUR KIDNEY TRANSPLANT: FINDINGTHE BEST MATCH AND BEST OUTCOMESscientificA successful transplant depends onmany factors.measurementsavailable—Pages 8 and 9to rateKIDNEY CARE QUALITY INITIATIVENew initiativeaims to define,assess, monitorand rewardquality care.—Page 13NEXT ISSUEDIABETESquality care.Adeera Levin, MD, FACPQUALITY OF CARE MAY SEEM LIKE AFUZZY CONCEPT TO YOU. YOU MAYFIND IT HARD TO MEASURE QUALITYWHEN IT COMES TO DIALYSIS. But, in try-ing to figure out what “quality” in dialysis caremeans, many of the important aspects havebeen clearly defined. There are scientific measurements available to rate quality of care.30 East 33rd StreetNew York, NY 10016800.622.9010www.kidney.orgNON-PROFIT ORG.U.S. POSTAGEPA I DShakopee, MNPermit No. 211The National KidneyFoundation (NKF), throughits Kidney Disease OutcomesQuality Initiative (KDOQI),has developed clinical practiceguidelines to help dialysis professionals—doctors, nurses,social workers and dietitians—improve outcomes for peoplewith chronic kidney disease(CKD). Since the KDOQI program began in 1995, studieshave shown improvement inmany patient outcome measures, such as anemia, dialysisadequacy and dialysis access.research. They define importantaspects of dialysis care, suchas the amount of dialysis treatment patients need, and theyrecommend clinical measuresthat help tell how well peopleon dialysis are doing. Yourcare team should do the testsdescribed in this article on aregular basis and make changesto your treatment if your resultsare not in the target range.When your lab results arewhere they should be, you willbe more likely to feel better andlive longer.The KDOQI recommendations are based on scientificFor example, your care teamshould do a monthly blood testto find your delivered dose ofdialysis. This tells whether youare getting the right amountof dialysis to remove enoughwastes from your blood andkeep you healthy. Your resultis called your Kt/V. Accordingto KDOQI, for hemodialysispatients, Kt/V should be at least1.2 per treatment. For people onperitoneal dialysis, the weeklyKt/V should be at least 1.7. Inhemodialysis, another measurethat may be used to check delivered dialysis dose is called ureareduction ratio, or URR. If URRis used, the result should be atleast 65 percent per treatment.Continued on page 3This publication is a part of the National Kidney Foundation’s Kidney Learning System (KLS).
F R O M T H E E D I TO RTHERE ARE TIMESWHEN THE MEANINGOF QUALITY IS CLEAR ANDOBJECTIVE. We know that anindividual needs an “adequate”amount of dialysis, measuredby such things as Kt/V. Wealso know that a person whois on dialysis should have ahematocrit and hemoglobinthat are in specific ranges. Itis generally agreed that theideal hemodialysis access is anarteriovenous fistula. Muchscientific evidence exists thatsupports each of these findings. The National KidneyFoundation’s (NKF) KidneyDisease Outcomes QualityInitiative (KDOQI) has evaluated that research data and usedit to develop clinical practiceguidelines in these and otherareas, confirming that there areindeed certain standards thatshould be met.the topic. We hopebeing might notthat this issue willbe of equal meaninggive you a wideto another individual.lens with whichFor example, to someto view quality, aslife would be incomwell as ways thatplete if they were noyou can improvelonger able to runthe overall qualitymarathons, yet othKarren Kingin and of your life.ers are quite satisfiedwith being able to take aOur next issue will be the lastwalk in the park. On the otherthat was planned by our 2006hand, someone might find cerEditorial Board. It will featuretain life situations intolerablediabetes, the major cause ofor unbearable, while someonechronic kidney disease, andelse might view the same situwill highlight the NKF’s newation with a totally differentest KDOQI guidelines. It is alsoperspective. Research has alsowith great sadness that I shareshown that we are not verywith you that the next issue ofgood at evaluating another perFamily Focus will be the last.son’s quality of life. This is mostWhile the NKF will continue tolikely because it is very difficultfind ways to educate those indifor us to assess someone else’sviduals who are on dialysis andsituation without allowing ourtheir families, it has decided toown value judgments, experimove in another direction.ences and circumstances to getin the way.However, there are other areaswhere quality measurementsare more subjective, personaland individual. Quality oflife— what is important andof value to you emotionally,socially, physically and vocationally—is one such area. Whatis crucial to one person’s well-However, regardless of whetherwe are talking about qualitymedical care or quality of life,both contribute a lot to one’sability to live a full, productivelife. Quality in all aspects oflife is vitally important, whichis why we have dedicated thisentire issue of Family Focus toDear Family Focus,Thank you,Donna NelmsDonna is 37-years-old and receives treatment inWest Warwick, Rhode Island.2FAMILY FOCUS Volume 16, Number 1In closing, I want to thank youfor your support and interest inFamily Focus. You have been aninspiration to each of us.Karren King, MSW, ACSW,LCSWFor the Editorial BoardNKF Family Focus is published by theNational Kidney Foundation.Opinions expressed in this newspaper donot necessarily represent the position ofthe National Kidney Foundation.EDITOR-IN-CHIEF:FITNESS EDITOR:Karren King, MSW, ACSW, LCSWKansas City, MOPatricia L. Gordon, RN, PhDSan Francisco, CAMEDICAL EDITOR:Wendy W. Brown, MD, Nashville, TNNURSING EDITOR:Sally Burrows-Hudson, MS, RN, CNNSunnyvale, CANUTRITION EDITOR:PATIENT EDITOR:READING YOUR PAPERHAS BROUGHT A LOTOF EASE AND HOPE. Ifeel now as if I do havea future ahead of me. Abright future. I cannotand will not let a littlething like dialysis stopme from living whenin reality it helps meto live. It’s hard butI abide by the rulesbecause I want to live. The staff atmy unit has made it easy for me to go through withmy treatments, and I am very grateful to them.It is also with great sadnessthat I write about the recentloss of Family Focus EditorialBoard member, JosephineMahi. Josephine had chronickidney disease and had beenon in-center hemodialysis since2000. She was a fairly recentmember of the Editorial Board,having been with the newspaper for less than one year.Although she was with us foronly a brief time, her contributions were always enlightening,and we appreciate the opportunity that we had to work withJosephine.PEDIATRIC EDITOR:SOCIAL WORK EDITOR:TRANSPLANT EDITOR:ESRD NETWORK LIAISON:EDITORIAL OFFICE:EDITORIAL DIRECTOR:EDITORIAL MANAGER:VICE PRESIDENT OF HEALTHPOLICY AND RESEARCH:EXECUTIVE EDITOR:MANAGING EDITORS:DESIGN DIRECTOR:Lori Fedje, RD, LD, Portland, ORJosephine Mahi, Brookings, SDBarbara Fivush, MD, Baltimore, MDMary Beth Callahan, ACSW/LMSW-ACPDallas, TXNancy Swick, RN, BSN, CCTCSanta Rosa, CAKimberly Thompson, RN, BSN, CNNKansas City, MONATIONAL KIDNEY FOUNDATION30 E. 33rd Street, New York, NY 10016800.622.9010 212.889.2210www.kidney.orgE-mail: info@kidney.orgGigi PolitoskiSheila Weiner, MSW, LCSWDolph Chianchiano, JD, MPASara KosowskyMelissa Caravella, Monica SirignanoOumaya Abi Saab
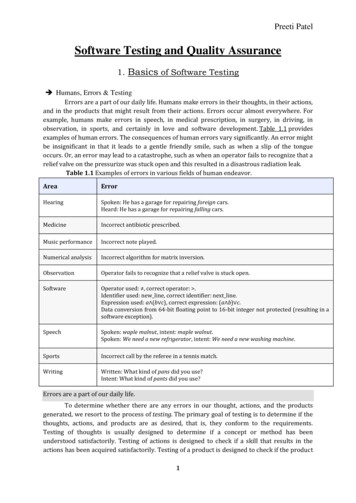
Improving Quality of Care in Dialysis Continued from page 1Over the past 15 years, manyimprovements have been notedin dialysis dose in the UnitedStates. Data published by theUnited States Renal DataSystem (USRDS; www.usrds.org) and the Dialysis Outcomesand Practice Patterns Study(DOPPS) showed a 50 percentincrease—from 0.99 in 1986to 1.53 in 2003. This improvement is due to more awarenessof the importance of dialysisand to the development ofclinical practice guidelines suchas the KDOQI guidelines onhemodialysis adequacy.Anemia treatment is anotherimportant part of quality carefor people on dialysis. Mostpeople with kidney disease getanemia because their kidneysno longer make enough of thehormone erythropoietin (EPO),which stimulates red blood cellproduction in the body. To treatthis problem, medications andiron supplements are used toraise red blood cell production.Hemoglobin is the key measurerecommended by KDOQI to tellif people are getting the rightamount of anemia treatmentand are responding well totheir treatment. Hemoglobinlevels should be 11 g/dLor higher. Results from theDOPPS showed the importanceof reaching the recommendedhemoglobin level. The studyreported that people who raisetheir hemoglobin level havea much lower risk of death.Other data from 2006, althoughpreliminary, show that mostpeople on dialysis are reachingthe KDOQI target for hemoglobin, but 15–20 percent are stillbelow the target.The following chart lists otherimportant clinical measures(tests) recommended by KDOQI.To ensure that you are gettingquality dialysis care, you shouldknow what your numbers are.Ask your dialysis care teamabout your results. Keep trackof your numbers. Your dialysiscare team may be able to giveyou a tracking tool. Or, youcan use the Dialysis Lab Logavailable from the NKF by calling 800.622.9010 or visitingthe Web site at www.kidney.org. If any of your results arenot in the target range, askyour care team what can bedone to improve them. Some ofthe steps you can take to helpinclude: TAKE all your medicationsas prescribed for you.FOLLOW your special dietcarefully.FOLLOW your fluid andsodium (salt) limits.DO all the dialysis treatments prescribed for you; donot skip treatments. LEARN all you can aboutyour kidney disease and itstreatment. Call the NKFtoll-free at 800.622.9010 fora list of brochures on dialysis or visit the Web site atwww.kidney.orgSPEAK to your care teamif you have any problems orquestions.Dr. Adeera Levin is a professorof medicine and the co-director of the Clinical InvestigatorProgram at the University ofBritish Columbia. She alsoserves as the executive directorof the British ColumbiaProvincial Renal Agency,the Director of the KidneyFunction Clinic at St. Paul’sHospital in Vancouver,Canada, and the KDOQICo-Chair at the NationalKidney Foundation.BEGIN your treatment ontime and complete the fulltreatment.Important Clinical Measures (Tests) Recommended by KDOQIName of TestKt/VWhat It ChecksDialysis doseKDOQI Recommended TargetAt least 1.2 per treatment for HD; at least 1.7per week for PDURR (Hemodialysis)Dialysis doseAt least 65 percent per treatmentHemoglobinAnemia control11 or greaterSerum ferritinIron stores in bodyAt least 200 (HD); at least 100 (PD)Transferrin saturation (TSAT)Iron stores in bodyAt least 20%AlbuminNutritional health4 or greaterPhosphorusBone health3.5–5.5CalciumBone health8.4–9.5Blood pressureBlood pressure controlLess than 140/90 pre-dialysis; less than 130/80on dialysisTotal cholesterolHeart healthLess than 200LDL cholesterolHeart healthLess than 100HDL cholesterolHeart health40 or moreTriglycerideHeart healthLess than 150Abbreviations: HD, hemodialysis; PD, peritoneal dialysis; URR, urea reduction ratio.FAMILY FOCUS Volume 16, Number 13
FOR RETIRED ATTORNEYROBERT GROSS, QUALITY IN HIS DIALYSIS EXPERIENCE IS SUMMED UPIN ONE WORD: PATIENCE.More than anything, he appreciates patience in his careteam and a caring atmosphereduring treatment sessions.Quality is a personal experience and is therefore differentfor each individual. Anotherperson, for example, reportedhaving a horrible time in thetreatment chair with restlesslegs syndrome (RLS), whichis a strong urge to move yourlegs often accompanied byuncomfortable sensations thatstart or become worse whenyou are resting. One day herprimary care nurse gave hera newspaper clipping from amedical column. In the article,the doctor described RLS andsuggested avoiding all caffeine-rich drinks like coffee,tea and colas. The person triedthe advice and after a coupleof weeks it worked. Qualityof life for this individual wasquite simply relief from restless twitching during dialysis.Today, people with CKD, boththose on dialysis and those inthe earlier stages of CKD, andtheir caregivers can compareMedicare-certified dialysisfacilities by services provided,characteristics and threequality measures— anemia,hemodialysis (HD) adequacyand patient survival—byusing the Dialysis FacilityCompare (DFC) tool launchedin January 2001 on Medicare’sWeb site (go to www.medicare.gov, then click on“Compare Dialysis Facilitiesin Your Area” at the bottomof the page). The anemia tabmeasures how well peopleon dialysis at a facility havetheir anemia (low red bloodcell count) under control. TheHD tab measures how manyindividuals at a facility getenough waste removed fromtheir blood during dialysistreatments (urea reduction4QUALITY in DialysisBy Josephine MahiKnowing what quality dialysis care means toyou can improve your quality of life.ratio [URR] of 65 or greater).The patient survival tab measures if the people treated ata facility generally live longerthan, as long, or not as long asexpected.The DFC tool also includesother types of informationon HD and peritoneal dialysis (PD) for individuals ondialysis and family members,such as dialysis and kidneydisease publications, linksto other kidney disease Websites, statement of rights andresponsibilities of people whodialyze and contact information for End Stage RenalDisease (ESRD) Networks andstate survey agencies.Care teams and nephrologists usually measure monthlyblood tests for levels of albumin, hemoglobin and Kt/V(URR) as markers of qualityof life. However, quality oflife, including physical andmental health and spiritualfactors are equal, if not moreimportant matters for peoplewith kidney failure in dialysisfacilities, based on the information gathered from participants with CKD in the study,“Promoting Excellence in Endof-Life Care” by the NationalProgram Office of the RobertWood Johnson Foundation (1).Those individuals who participated in the study respondedto interviewers’ questionsbased on the McGill Qualityof Life Questionnaire, theSatisfaction of Life Scale, andtwo patient satisfaction scales,with one adapted from theKidney Disease Quality of Lifeinstrument. The interviewersincluded a new scale exploringthe effects of spiritual beliefsand patient supports. Issuessuch as encouragement fromFAMILY FOCUS Volume 16, Number 1the care team and their levelof satisfaction with doctors,nurses and social workerswere important. More researchneeds to be done to help dialysis care teams improve qualityof life with an informed understanding of the psychologicaland social needs of the personon dialysis.concerned physicians and thevoices of patients, there maycome a time when dialysis providers receive payment basedon measurements of the quality of care given.REFERENCE1. Robert Wood Johnson Foundation.Executive summary of findings fromthe ESRD Quality of Life for DialysisPatients Questionnaire Study. l Editor's Note:Josephine passed away inFebruary. She had chronic kidney disease and had been on incenter hemodialysis since 2000.HandsBy John RiderJosephine MahiTo support the educationalneeds of people on CKD andtheir families for a betterquality of life, the NationalKidney Foundation launchedKidney Learning System(KLS) in April 2003. KLSprovides live programs andaudio/video and printed materials for people with CKD.Visit www.kidney.org/KLSor call 800.622.9010. Requesta copy of the NKF Patientand Family Council DialysisPatients’ Bill of Rights andResponsibilities, or view itonline at www.nkfkidneypatients.orgThe demand for quality indialysis should be a priorityfor people with CKD becauseit would lead to better outcomes and decreased hospitalizations. Concerns about costefficiency and dialysis caredelivery should bring aboutchanges in the future. Withthe leadership of Congress,There is a special groupWho come into this place,With hands of love and kindness,Bringing helpful care and grace.Sometimes the day is hardWith many ups and downsBut they handle each and every one,Without any grumps and frowns.Their hands are sure and nimble,As we watch them do their workWith the sounds of daily business,There is never time to shirk.Friends of those who come here,Are amazed at all they doThey encourage all of us folks,Without an ounce of rue.Their hands and great big hearts,A wonder in every wayLet’s clap our hands for them,Let’s honor them today.John’s wife dialyzes at CedarValley Dialysis Center inWaterloo, Iowa.
TM E D I C A LC O R N E RNational Kidney Foundation'sDialysis Guidelines UpdatesIf you are preparing for HD,plans for a vascular accessshould be made at least sixmonths before you start dialyBy Michael Rocco, MDsis. Planning early will helpimprove the chances thatUpdated guidelines help to determinea fistula (also known as anarteriovenous [AV] fistula),the treatment plan that's best for you.the preferred type of access,recommended unless yourstarted and allow the doctorwill be ready to use whendoctor is able to test your urine you start dialysis. A fistulato take care of other medicalto be sure that your kidneysproblems that may be presentis the best type of accessclear enough waste productsbecause of kidney disease.because they last longer andon their own.For people who receive HDhave fewer problems thanthree times a week, the recgrafts or catheters. A gortexFor individuals on PD, theommendation about howgraft should be consideredminimum amount of dialysismuch dialysis is needed hasfor dialysis access only if ayou should get has been lownot changed. The amount offistula cannot be placed. Thedialysis is based on blood work ered to achieve a weekly Kt/Vuse of catheters for dialysisof 1.7. This change is based on access should be discouragedobtained at the start and endseveral studies done in Mexico because long-term catheterof the dialysis session. Theseand Hong Kong that showednumbers show how muchuse results in a higher risk ofdialysis has cleaned your blood this lower dose of dialysis didinfections and death comparednot result in a higher rate ofof the waste products thatwith fistulas or graphs. Oncebuild up when your kidneys do death. All people on PD should a fistula is placed, the doctorhave enough dialysis to be atnot work. The reduction ratioshould examine it about sixleast at this level, and somebetween the blood urea nitroweeks later to find out if themay require levels higher than fistula is growing normallygen level at the start and end1.7 to stay healthy. Your doctor or if some additional surgeryof dialysis (the urea reductionratio or URR) should be higher will determine if you need awill be needed to make thehigher amount of dialysis. You fistula usable for dialysis. Thethan 65%, which is aboutYour stage of kidney disease is equivalent to a Kt/V (yourneed to bring your collection of guidelines inform doctors andbased on the presence of kiddialysis fluid and urine (if youdelivered dose of dialysis) ofdialysis units how to monitorney damage and your glomeru- 1.2 or more. This recommenda- make any) to the home trainthe access on a regular basislar filtration rate (GFR), which tion is based on a study calleding unit at least three times ato allow them to find and fixis a measure of your level ofyear to help determine if youthe HEMO Study. This studyproblems as early as possiblekidney function. Thus, theare getting enough dialysis.was done in more than 1,800to keep the access from failing.treatment of your kidney dispeople in the United Statesease is based on your level ofwho received HD three timesWhether you receive HD orare on PD, it is important foryou to work with your doc"Whether you receive HD or are on PD, it istor to be sure that your bloodimportant for you to work with your doctorpressure is under good control. Blood pressure controlto be sure that your blood pressure is underincludes not only taking yourblood pressure medicines, butgood control."Peritoneal Dialysisalso not eating too much saltkidney function. People with a per week and showed thator drinking too much fluid.GFR less than 30 ml per minincreasing the time for eachIf you are on HD, limitingThe dialysis unit should haveute should know about the dif- dialysis treatment by aboutyour fluid intake not onlya plan to look at the qualityferent ways to replace kidney30 to 45 minutes per sessionmakes controlling your bloodof care for all people on dialyfunction, including HD in adid not lower the death ratepressure easier, you are lesssis. Recommendations of whatdialysis center or at home, PD for people on dialysis. Therelikely to have cramps or lowto look at are included in theand kidney transplant. If your are now new recommendations blood pressure during treatguidelines. Finally, recommenGFR falls to 15 ml perthat help your doctor decidement. For those on PD, if youdations are given for childrenminute or less, regular dialyhow much dialysis you needlimit the amount of fluid youwho are on either HD or PD.sis may need to be started.if you dialyze either more ordrink, you may need to useConsultation with a kidneyless than three times perfewer dialysate bags withEvaluation and treatment ofdoctor (nephrologist) will helpweek. Getting HD less thana high dextrose or sugaranemia for people on dialysisdecide when dialysis should be three times a week is notconcentration.Continued on page 12REATMENT GUIDELINESFOR HEMODIALYSIS(HD) AND PERITONEALDIALYSIS (PD) ADEQUACY,VASCULAR ACCESS ANDANEMIA (LOW RED BLOODCELL COUNT) WERE FIRSTPUBLISHED IN 1997 ANDFIRST UPDATED IN 2001.Because a number of importantstudies were done to improvetreatment for people on dialysissince 2001, new informationwas available and the NationalKidney Foundation decidedthat it was time for anotherupdate. These new guidelineswere outlined in the supplement to the July 2006 edition ofthe American Journal of KidneyDiseases (AJKD) and are highlighted below.FAMILY FOCUS Volume 16, Number 15
H E L P I N GQUALITY MEANS DIFFERENT THINGS TODIFFERENT PEOPLE. TheU.S. Office of PersonnelManagement defines “good”quality health care as doingthe right thing at the righttime in the right way forthe right person and gettingthe best possible results (1).Experiencing quality in yourlife means investing time andenergy in yourself. Ways tobegin investing are to understand and manage your disease. “Doing the right thing”belongs to both you and yourhealth care team.In 1998, the Centers forMedicare and MedicaidServices (CMS) developed EndStage Renal Disease (ESRD)Clinical Performance Measures(CPMs) based on the NationalKidney Foundation’s KidneyDisease Outcomes QualityInitiative (NKF-KDOQI ; ref.2). Sixteen CPMs were identified to measure and reportthe quality of dialysis servicesprovided under Medicare (3).However, the performancemeasures relating to bonehealth, nutrition, anemia,diabetes and blood pressureare expected outcomes for allpeople with CKD, regardlessof stage of kidney failure ortreatment. Table 1 lists several of these quality measurements (see page 7).These measurements are onlya few pieces of the puzzlerequired to achieve high quality care for you. Although yourhealth care team is responsiblefor providing the education,you need to understand eachmeasurement and how to getto your target as you go aboutyour daily activities. Of course,you should participate as ateam member to ensure thatyou are meeting your goalson a monthly basis. The tableshows a checklist to help youtrack if you met your target.6Y O U R S E L FQUALITY OF CARE: You Are in ChargeBy Jennifer Vavrinchik, MSN, RN, CNNTake charge of your health by makinghealthy lifestyle choices.If not, develop an action planwith your health care team toachieve your goals.Being faced with a chronicillness and ongoing treatmentcan be a frightening experience, especially at first if youdo not know what to expect. Itis your responsibility to applywhat you have learned toeveryday living, and in return,lessen your fears and live lifeto the fullest. Examples maybe learning new recipes for aCKD diet and savoring everya quality life. One thing thatmight help is to get involvedwith patient organizations tolearn more about your disease and how others like youmanage their daily activities.Ask yourself and your doctorand staff what changes youneed to make. Pick one or twoand work on them little bylittle. This is the essence ofself-management, which linkswith higher physical andmental functioning (4). Askyour health care team thefollowing questions throughout your care.1. HOW can I keep my qualitymeasurements in the goalrange? By medication, diet,lifestyle?2. WILL I see my laboratoryresults every month? Whowill review them with me?3. WILL someone help me withmy diet and make suggestions for menus and recipesthat are good for me?Your health care teamhas a responsibility to“do the right thing” andprovide quality care, butultimately, you are incontrol of your care.bite, learning to enjoy activities again because your energylevel has improved or goingback to work because you havelearned to manage your disease. Taking small steps eachday toward a more normaland healthy lifestyle willbring you one step closer toachieving your goals towardFAMILY FOCUS Volume 16, Number 14. WHAT help can I get withquestions about health insurance and prescription drugs?5. WHO will help me withwork and family issues? Arethere support groups for meand my family to discussthese issues?6. WHAT are my treatmentoptions? Which treatmentmodality (HD, PD or transplant) is best for me?7. WHAT kind of vascularaccess do I have and how doI care for it? Am I a candidate for a fistula?8. WILL I have access to mymedical records? Havingaccess to your medicalrecords allows for greaterknowledge and coordinationof care for both you and yourhealth care team.9. WILL my various doctorsand health care team talkto one another to coordinatemy care?The more you know aboutyour treatment and healthstatus, the better able youwill be to care for yourself andlive a quality life. Expect noless. Your health care teamhas a responsibility to “do theright thing” and provide quality care, but ultimately, youare in control of your care.Get involved with the healthcare team to set your monthlygoals. Ask questions! The bottom line is to invest in you andquality will follow.REFERENCES1. Office of Personnel Management.Federal Employees Health BenefitsGlossary. 28 April 2006. www.opm.gov/insure/health/about/glossary.asp 2. National Kidney Foundation. ClinicalPractice Guidelines. 11 June 2006. www.kidney.org 3. Center for Medicare and MedicaidServices. Clinical PerformanceMeasure (CPM) Project. 11 June2006. www.cms.hhs.gov/CPMProject 4. Curtin, R.B. Self-management,Knowledge, and Functioningand Well-being of Patients onHemodialysis. Nephrology NursingJournal 41:1286–1292, 2003.Jennifer Vavrinchik holdsa Master of Science andBachelor of Science inNursing from the University ofCincinnati. She has 18 yearsexperience in nephrology asa clinical educator, and staffdevelopment and client services professional.
C H I L D ' SYOU MAY NOT KNOWTHAT THE KIDNEYSCONTROL BLOOD PHOSPHORUS, A MINERALFOUND IN BONES. The kidneys also turn the vitamin Dthat we get in our diets into ahormone that helps our bodiesabsorb calcium, which is important for keeping bones strongand healthy.When the kidneys fail, phosphorus builds up in the bloodand levels of calcium andvitamin D fall. These changeslead to higher amounts ofparathyroid hormone (PTH),which is made by the parathyroid glands, and weaker bones(commonly known as rickets).The medical term for thiscondition is renal osteodystrophy, which is one of the majorreasons children with chronickidney disease may not grownormally.The signs and symptoms ofrenal osteodystrophy are listedin Table 1. Fortunately, bloodtests and X-rays can be used tocheck for signs of renal osteodystrophy, and medicationssuch as phosphate binders andspecial forms of vitamin D canbe used to treat it. Althoughpediatric nephrologists haveknown about renal osteodystrophy for many years, they didnot agree on guidelines for howto watch for it and treat it.This changed in October of2005, when the NationalKidney Foundation’s KidneyDisease Outcomes QualityInitiative published BoneMetabolism and Disease inChildren with Chronic KidneyDisease as a supplement to theAmerican Journal of KidneyDiseases. This publication isthe result of three years’ workby eight volunteer experts inkidney disease, pediatrics,nutrition, bone and mineralmetabolism disorders whoreviewed scientific evidenceH E A L T HYour Child's HealthBy Joseph T. Flynn, MD, MSNew bone disease guidelines for children highlight the importance of early interventionpublished in medical journalsbefore writing the guidelines.Many aspects of renal osteodystrophy in children are highlighted in the new guidelines.For example, the guidelinespoint out that osteodystrophybegins early in the course ofCKD in children and thatGood nutrition, especiallygetting enough calciumand vitamin D, and avoiding too much phosphorus,is the first step recommended by the guidelines inmanaging osteodystrophy.children must have enoughcalcium in their diets in orderto grow and develop properly.The importance of vitamin Dand proper nutrition in childrenwith CKD is stressed, as is theneed to check levels of calcium,phosphorus and PTH regularly.As seen in Table 2 (p. 11), thenew guidelines vary for different stages of CKD. Thisis because some of the goalsand treatments used for earlier stages of CKD are different than those for people ondialysis, and vice versa. Forexample, treating the problemof not enough dietary vitaminD is helpful in mild to moderate CKD Stages 2, 3 and 4,but probably is not helpful inCKD Stage 5, when dialysisis needed.Good nutrition, especially getting enough calcium and vitamin D, and avoiding too muchphosphorus, is the first steprecommended by the guidelinesin managing renal osteodystrophy.
be more likely to feel better and live longer. For example, your care team should do a monthly blood test to find your delivered dose of dialysis. This tells whether you are getting the right amount of dialysis to remove enough wastes from your blood and keep you healthy. Your result