Transcription
Federally Qualified Health CentersWashington Apple Health (Medicaid)Federally-QualifiedHealth Centers (FQHC)Billing GuideJanuary 1, 2020Every effort has been made to ensure this guide’s accuracy. If an actual or apparent conflict between thisdocument and an agency rule arises, the agency rules apply.1
Federally Qualified Health CentersAbout this guide*This publication takes effect January 1, 2020, and supersedes earlier guides to this program.HCA is committed to providing equal access to our services. If you need an accommodation orrequire documents in another format, call 1-800-562-3022. People who have hearing or speechdisabilities call 711 for relay services.Washington Apple Health means the public health insurance programs for eligibleWashington residents. Washington Apple Health is the name used in WashingtonState for Medicaid, the children's health insurance program (CHIP), and stateonly funded health care programs. Washington Apple Health is administered bythe Washington State Health Care Authority.Who should use this billing guide?Federally qualified health centers (FQHCs) rendering services for encounter eligible AppleHealth clients who are fee-for-service and not in an integrated managed care (IMC) plan.*This publication is a billing instruction.2
Federally Qualified Health CentersWhat has changed?SubjectEntire guideChangeGeneral housekeeping,including hyperlink andtypographical correctionsReason for ChangeTo improve usabilityDefinitionsRemoved definition ofBehavioral HealthOrganization (BHO).Effective January 1, 2020, behavioralhealth services in all regions will beprovided under integrated managedcare.Added definitions forBehavioral HealthAdministrative ServiceOrganization (BH-ASO),Behavioral Health ServicesOnly (BHSO), and integratedmanaged care (IMC).Behavioral HealthOrganization (BHO)Removed this section and allreferences to BHOsthroughout the guide.Effective January 1, 2020, behavioralhealth services in all regions will beprovided under integrated managedcare.Integrated Managed Care Effective January 1, 2020,Effective January 1, 2020, HCARegionsintegrated managed care iscompleted the move to whole personbeing implemented in thecare to allow better coordination oflast three regions of the state: care for both body (physical health)and mind (mental health and Great Rivers (Cowlitz,substance use disorder treatment,Grays Harbor, Lewis,together known as “behavioralPacific, and Wahkiakumhealth”). This delivery model iscounties)called Integrated Managed Care Salish (Clallam,(IMC).Jefferson, and Kitsapcounties) Thurston-Mason(Mason and Thurstoncounties)Determining whether aAdded CPT code 99188To align with dental-related servicesservice is an encounterbilling guideMedical coverage group Added Recipient AidPolicy changecodesCategory (RAC) code 1272Medical/maternity/mental Revised language andhealth encounterreferences regardingencounter codes3Correction
Federally Qualified Health CentersSubjectHow does the agencyprevent duplicativepayment for pharmacyand BHO services?ChangeAdded language regardingpharmacy recoupmentprocessReason for ChangeTo clarify current change-in-scopepolicyHow can I get agency provider documents?To access provider alerts, go to the agency’s provider alerts webpage.To access provider documents, go to the agency’s provider billing guides and fee scheduleswebpage.How can I get agency fee schedules?To download and print agency fee schedules, go to the agency’s Rates Development FeeSchedules webpage.Copyright disclosureCurrent Procedural Terminology (CPT) copyright 2019 AmericanMedical Association (AMA). All rights reserved. CPT is aregistered trademark of the AMA.Fee schedules, relative value units, conversion factors and/orrelated components are not assigned by the AMA, are not part ofCPT, and the AMA is not recommending their use. The AMA doesnot directly or indirectly practice medicine or dispense medicalservices. The AMA assumes no liability for data contained or notcontained herein.4
Federally Qualified Health CentersTable of ContentsResources Available .8Definitions .9Program Overview .11What is a federally qualified health center (FQHC)? .11What is the purpose of the FQHC program? .12What are the basic requirements for services provided in an FQHC? .12Who may provide services in an FQHC? .13What are the FQHC staffing requirements?.14How does an FQHC enroll as a provider? .14What is the effective date of the Medicaid FQHC certification?.15Servicing site location certification .15Client Eligibility .16How do I verify a client’s eligibility? .16Are clients enrolled in an agency-contracted managed care organization (MCO)eligible? .17Managed care enrollment .18Apple Health – Changes for January 1, 2020 .19Clients who are not enrolled in an agency-contracted managed care plan forphysical health services.20Integrated managed care (IMC) .20Integrated Apple Health Foster Care (AHFC) .22Encounters .23What is an encounter? .23What services are considered encounters? .23Alcohol or substance misuse counseling .24Surgical procedures .24Services and supplies incidental to professional services .24Determining whether a service is an encounter .25What services do not qualify as encounters? .29Collaborative care model (CoCM) services .29What FQHC-related activities are NOT covered by the agency? .30Categories of encounters .30Medical/maternity/mental health encounter .30Maternity Support Services and Infant Case Management (MSS/ICM) .31Dental encounter .32Mental health encounter – clients whose mental illness requires a higher acuityservice .32Mental health encounter – psychiatrists and psychologists .32Substance use disorder treatment programs .32Alert! This Table of Contents is automated. Click on a page number to go directly to the page.5
Federally Qualified Health CentersReimbursement .33When does the agency pay for FQHC services? .33The reimbursement structure .33Payment for services eligible for an encounter .34Payment for services not eligible for an encounter .34Choice of rates .35Managed care clients.35Enhancement payments for managed care clients .36Are FQHCs liable for payments received? .36How does the agency prevent duplicative payment for pharmacy and behavioralhealth services? .37What is a change in scope of service? .37What are the criteria for a change in scope of service rate adjustment? .37How is a change in scope of service rate adjustment requested? .38What is a prospective change in scope of service? .39What is a retrospective change in scope of service? .40How does the agency process applications for a change in scope of service rateadjustment? .40How does the agency set an interim rate for prospective changes in the scope ofservice? .41How does the agency set an adjusted encounter rate for retrospective changes inthe scope of service? .41When does the agency conduct a post change in scope of service rate adjustmentreview? .42May an FQHC appeal an agency action? .43What are examples of events that qualify for a rate adjustment due to changes inscope of service? .43What are examples of events that do not qualify for a rate adjustment due tochanges in scope of service? .44Reporting Requirements .45What are allowable costs? .45What are allowed direct health care costs? .45What are unallowable direct health services costs? .48What are allowable uncapped overhead costs? .50What are allowable capped overhead costs? .51What are unallowable overhead costs and other expenses?.52What are the requirements for cost reports? .55Desk reviews and audits.56Submission requirements .56Productivity, full-time equivalent (FTE), and treatment of on-call time .58Productivity standards and capped overhead methodology .59Encounters for all patients .59Billing .60What are the general billing requirements? .60Alert! This Table of Contents is automated. Click on a page number to go directly to the page.6
Federally Qualified Health CentersWhat special rules are there for FQHCs to follow when billing? .60How do I bill for encounter services? .61How do I bill for maternity care? .63How do I bill for orthodontic services performed in an FQHC? .64What are the rules for telemedicine? .65How do I bill for more than one encounter per day? .65What procedure codes must an FQHC use? .66Can FQHCs get paid for noncovered services? .66How do I bill taxonomy codes? .67Billing taxonomy electronically.67How do I bill claims electronically? .68How do I handle crossover claims in an FQHC setting? .69How do I handle Managed Medicare or Medicare Part C crossover claims for dentalbilling? .69Alert! This Table of Contents is automated. Click on a page number to go directly to the page.7
Federally Qualified Health CentersResources AvailableTopicContactInformation on becoming aprovider or submitting a changeof address or ownershipInformation about payments,claims processing, denials, oragency managed careorganizationsElectronic billingSee the agency’s Billers and Providers webpage.Finding agency documents(e.g., billing guides, feeschedules)Private insurance or third-partyliability, other than agencycontracted managed careSubmit claim denials for reviewFollow the instructions in the agency’s Billers andProviders webpage.Information about ICD-10Email: ICD10questions@hca.wa.govWho do I contact if I havequestions about enrolling as amedical assistance-certifiedFQHC?Who do I contact if I have aquestion about overallmanagement of the program orspecific payment rates?Provider EnrollmentPO Box 45562Olympia, WA 98504-5562Ph.: 800-562-3022, ext. 16137Fax: 360-725-2144providerenrollment@hca.wa.govEmail: FQHCRHC@hca.wa.gov8
Federally Qualified Health CentersDefinitionsThis section defines terms and abbreviations, including acronyms, used in this billing guide.Refer to Chapter 182-500 WAC for a complete list of definitions for Washington AppleHealth.Alternative payment methodology (APM)index – A measure of input price changesexperienced by Washington’s federallyqualified health center (FQHC) and ruralhealth clinic (RHC) providers. The index isderived from the federal MedicareEconomic Index (MEI) and Washingtonspecific variable measures. The APM indexis used to update the APM encounterpayment rates on an annual basis.Encounter – A face-to-face visit between aclient and a qualified FQHC provider (e.g., aphysician, physician assistant, or advancedregistered nurse practitioner) who exercisesindependent judgment when providingservices that qualify for an encounter rate.Encounter rate – A cost-based, facilityspecific rate for covered FQHC servicespaid to an FQHC for each valid encounter itbills.Base year – The year used as the benchmarkin measuring an FQHC’s total reasonablecosts for establishing base encounter rates.Enhancements (also called managed careenhancements) -- A monthly amount paidby the agency to FQHCs for each clientenrolled with a managed care organization(MCO). MCOs may contract with FQHCs toprovide services under managed careprograms. FQHCs receive enhancementsfrom the agency in addition to the negotiatedpayments they receive from the MCOs forservices provided to enrollees. To ensurethat the appropriate amounts are paid to eachFQHC, the agency performs an annualreconciliation of the enhancement payments.Behavioral Health Administrative ServiceOrganization (BH-ASO) – Means an entityselected by the agency to administerbehavioral health services and programs,including crisis services for all people in anintegrated managed care regional servicearea. The BH-ASO administers crisisservices for all people in its defined regionalservice area, regardless of a person’s abilityto pay.Fee-for-service – A payment method theagency uses to pay providers for coveredmedical services provided to medicalassistance clients, except those servicesprovided under the agency’s prepaidmanaged care organizations, or thoseservices that qualify for an encounter rate.Behavioral Health Services Only (BHSO)– Means the program in which enrolleesreceive only behavioral health benefitsthrough a managed care delivery system.Cost report – A statement of costs andprovider usage that occurred during the timeperiod covered by the cost report. FQHCsmust complete a cost report when there is achange in scope, rebasing of the encounterrate, or when the agency sets a base rate.9
Federally Qualified Health CentersIntegrated Managed Care – Means theprogram under which a managed careorganization provides: Physical health services funded byMedicaid; and Behavioral health services funded byMedicaid and other available resourcesprovided for in chapters 182-538B, 182538C, and 182-538D WAC.Mid-level practitioner –An advancedregistered nurse practitioner (ARNP), acertified nurse midwife, a licensed midwife,a woman’s health care nurse practitioner, aphysician’s assistant (PA), or a psychiatricARNP. Services provided by registerednurses are not encounters.Rebasing – The process of recalculatingencounter rates using actual cost report data.Interim rate – The rate established by theagency to pay an FQHC for covered FQHCservices prior to the establishment of apermanent rate for that facility.Medicaid certification date – The date anFQHC can begin providing services toMedicaid clients.10
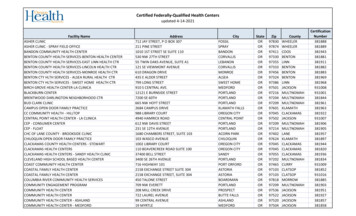
Federally Qualified Health CentersProgram OverviewWhat is a federally qualified health center(FQHC)?A federally qualified health center (FQHC) is a facility that is any* of the following: Receiving grants under Title 42, Chapter 6A, Subchapter II, Part D, subpart i, section254b of the U.S. Code (formerly known as Section 330 of the Public Health ServicesAct) Receiving the grants referenced above based on the recommendation of the HealthResources and Services Administration (HRSA) within the Public Health Service, asdetermined by the secretary, to meet the requirements for receiving such a grant A Tribe or Tribal organization operating outpatient health programs or facilities under theIndian Self-Determination Act that elects to be designated as an FQHC (see the programoverview in the Tribal Health Program Billing Guide for more information.)*Refer to other requirements within this guide.An FQHC is unique only in the way it is paid for services eligible for an encounterpayment, not by the scope of coverage for which it is paid.Note: A corporation with multiple sites may be designated as a single FQHC, oreach site may be designated as an individual FQHC, depending on the designationby the U.S. Department of Health & Human Services (DHHS).Participation in the FQHC program is voluntary.The agency allows only Department of Health and Human Services (DHHS)-designated FQHCsto participate in the FQHC program.Participating FQHCs receive an encounter payment that includes medical services, supplies,and the overall coordination of the services provided to the agency client.Nonparticipating DHHS-designated FQHCs receive reimbursement on a fee-for-service basis.11
Federally Qualified Health CentersWhat is the purpose of the FQHC program?The purpose of the FQHC program is to enhance the provision of primary care services inunderserved urban and rural communities. FQHCs are “safety net” providers, such as communityhealth centers, public housing centers, and outpatient health programs funded by the IndianHealth Service, and programs serving migrants and the homeless.What are the basic requirements for servicesprovided in an FQHC? FQHCs must furnish all services according to applicable federal, state, and local laws. Unless otherwise specified, FQHC services provided are subject to the limitations andcoverage requirements detailed in the Physician-Related Services/HealthcareProfessional Services Billing Guide and other Washington Apple Health programspecific billing guides. The agency does not extend additional coverage to clients inan FQHC beyond what is covered in other agency programs and state law. The FQHC must be primarily engaged in providing outpatient health services. FQHCstaff must furnish those diagnostic and therapeutic services and supplies commonlyfurnished in a physician’s office or the entry point into the health care deliverysystem. These include: Medical historyPhysical examinationAssessment of health statusTreatment for a variety of medical conditionsThe FQHC must provide medical emergency procedures as a first response tocommon life-threatening injuries and acute illness. The FQHC must have availablecommonly used drugs and biologicals, such as: AnalgesicsAnesthetics (local)AntibioticsAnticonvulsantsAntidotes and emeticsSerums and toxoids12
Federally Qualified Health CentersWho may provide services in an FQHC?(WAC 182-548-1300(3) and RCW 18.36A.040)The following people may provide FQHC services: Physicians Dentists Physician assistants (PAs) Nurse practitioners (NPs) Nurse midwives or other specialized nurse practitioners Certified nurse midwives Registered nurses (RNs) or licensed practical nurses (LPNs) Mental health professionals – for a list of qualified professionals eligible to providemental health services, refer to the Mental Health Services Billing Guide Naturopathic physicians, refer to the Physician-Related Services/Health CareProfessional Services Billing GuideNote: Providers approved to deliver screening, brief intervention, and referral totreatment (SBIRT) services, Maternity Support Services/Infant Case Management(MSS/ICM), and substance use disorder services may also provide services in an FQHC.13
Federally Qualified Health CentersWhat are the FQHC staffing requirements?(42 CFR 491.7-8)All of the following are staffing requirements of an FQHC: An FQHC must be under the medical direction of a physician. An FQHC must have a health care staff that includes one or more physicians. A physician, physician’s assistant (PA), advanced registered nurse practitioner (ARNP),midwife, clinical social worker, or clinical psychologist must be available to furnishpatient care services within their scope of practice at all times the FQHC operates. The staff must be sufficient to provide the services essential to the operation of theFQHC.A physician, PA, ARNP, midwife, clinical social worker, or clinical psychologist member of thestaff may be the owner or employee of the FQHC, or may furnish services within thepractitioner’s scope of practice under contract to the FQHC. The staff may also include ancillarypersonnel who are supervised by the professional staff.How does an FQHC enroll as a provider?(WAC 182-548-1200 (2))To enroll as a provider and receive payment for services, an FQHC must: Receive FQHC certification for participation in the Title XVIII (Medicare) programaccording to 42 C.F.R. Part 491. Go to http://www.cms.hhs.gov/home/medicare.asp forinformation on Medicare provider enrollment. Submit a signed Core Provider Agreement (CPA). Comply with applicable federal, state, and local laws, rules, regulations, and agreements.When enrolling a new clinic through ProviderOne, select the Fac/Agency/Org/Inst option fromthe enrollment type menu.When adding a new site or service, indicate on the CPA that the provider is an FQHC.14
Federally Qualified Health CentersWhat is the effective date of the Medicaid FQHCcertification?(WAC 182-548-1200 (2))The agency uses one of two timeliness standards for determining the effective date of aMedicaid-certified FQHC: Medicare’s effective date: The agency uses Medicare’s effective date if the FQHCreturns a properly completed CPA and FQHC enrollment packet within 60 calendardays from the date of Medicare’s letter notifying the center of the Medicare certification. The date the agency receives the CPA: The agency uses the date the signed CPA isreceived if the FQHC returns the properly completed CPA and FQHC enrollment packet61 or more calendar days after the date of Medicare’s letter notifying the center of theMedicare certification.Note: The FQHC enrollment packet includes: CPA, ownership disclosure form,debarment form, Electronic Funds Transfer (EFT) form, W9, copy of business license,copy of liability insurance information, and either the Centers for Medicare and MedicaidServices (CMS) approval letter or the Health Resources and Services Administration(HRSA) approval letter. Dental, Substance Use Disorder, and Maternity Support Servicessites must provide the HRSA approval letter to the agency.Servicing site location certificationAll servicing sites listed under a clinic’s domain within ProviderOne must be certified by eitherCMS or HRSA depending on the kinds of services offered at the location. Site certificationdocuments can be faxed to the agency using the correct cover sheet, which will then beautomatically attached to the domain requesting a new servicing location.Refer to the agency’s Billers and Providers website for document submission cover sheets. Thecorrect cover sheet is the Provider Information Update Requests document. Because this is anestablished domain, select either the NPI or the ProviderOne ID option. The clinic’s ProviderOneID is the same number as the domain number. On the site approval document, note whichlocation code this approval document pertains to.15
Federally Qualified Health CentersClient EligibilityMost Apple Health clients are enrolled in an agency-contracted managed care organization(MCO). This means that Apple Health pays a monthly premium to an MCO for providingpreventative, primary, specialty, and other health services to Apple Health clients. Clients inmanaged care must see only providers who are in their MCO’s provider network, unless priorauthorized or to treat urgent or emergent care. See the agency’s Apple Health managed carewebpage for further details.It is important to always check a client’s eligibility prior toproviding any services because it affects who will pay for the services.How do I verify a client’s eligibility?Check the client’s Services Card or follow the two-step process below to verify that a client hasApple Health coverage for the date of service and that the client’s benefit package covers theapplicable service. This helps prevent delivering a service the agency will not pay for.Verifying eligibility is a two-step process:Step 1. Verify the patient’s eligibility for Apple Health. For detailed instructions onverifying a patient’s eligibility for Apple Health, see the Client Eligibility, BenefitPackages, and Coverage Limits section in the agency’s ProviderOne Billing andResource Guide.If the patient is eligible for Apple Health, proceed to Step 2. If the patient is noteligible, see the note box below.Step 2. Verify service coverage under the Apple Health client’s benefit package. Todetermine if the requested service is a covered benefit under the Apple Health client’sbenefit package, see the agency’s Program Benefit Packages and Scope of Serviceswebpage.16
Federally Qualified Health CentersNote: Patients who are not Apple Health clients may submit an application forhealth care coverage in one of
Jan 01, 2020 · provider usage that occurred during the time period covered by the cost report. FQHCs must complete a cost report when there is a change in scope, rebasing of the encounter rate, or when the agency sets a base rate. Encounter – A face-to-face visit between a client and a qualified FQHC provider