Transcription
10th Annual Phoenix Area Integrated Behavioral Health TrainingApril 2013Norman G. Hoffmann, Ph.D.Evince Clinical sment.com828-454-9960
OVERRIDING PRINCIPLESClinicians make diagnoses –instruments don’tInstruments are tools to be used bycliniciansClinicians are not servants to toolsClinicians make decisions –tools don’t
Co-occurring PrevalencesMany adults presenting for services haveco-occurring conditions requiring treatmentfor bothSome with substance use disorders havesubstance induced MH problemsSome with MH conditions self-medicate andexperience substance related problemsSome have independently occurringconditionsExact rates will vary with setting andpopulation
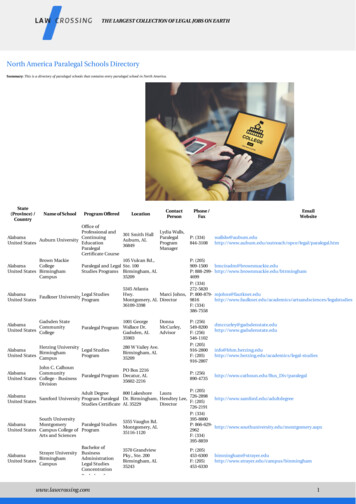
NIMH Epidemiologic CatchmentArea Study Lifetime PrevalenceN 18,571 ADULTSPrimaryPsychiatricDisorders28%havebothDrug orAlcoholAbuseGoodwin, F.K., J.A.M.A., 1989; 261:3517
NIMH Epidemiologic CatchmentArea Study Lifetime PrevalenceN 18,571 ADULTSPrimaryAlcohol orDrug Abuse71%havebothGoodwin, F.K., J.A.M.A., 1989; 261:3517PsychiatricDisorders
Screening vs.Diagnostic AssessmentScreens provide probability estimates.Screens should be fast, cheap, andeasy to use by those who are notnecessarily experts in the area underconsideration.Diagnostic assessment should be ascomplete and definitive as possible.Professionals with expertise in the areain question determined diagnoses.
WHEN TO SCREEN?WHEN TO ASSESS?Screen for what is NOT the presentingcomplaint or problem area.Screen for common problems otherthan the presenting complaintAddiction programs screen for MHMH clinics screen for addictionsDo an assessment for the presentingcomplaint or problem area and forpositive screen results.
The UNCOPEU – Have you spent more time drinking/usingthan intended? (Unintended Use)N – Have you ever neglected usualresponsibilities because of using?C – Have you ever wanted to cut down ondrinking/using?O – Has anyone objected to yourdrinking/use?P – Have you found yourself thinking a lotabout drinking/use? (Preoccupied)E – Have you ever used to relieve emotionaldistress, such as sadness, anger, orboredom?
UNCOPE: A Brief Screen forSubstance Use Disorders Six items used in screening adults andadolescents for any substance use disorder Free –from Evince Clinical Assessments[research tab at www.evinceassessment.com] Three or more positive responses indicaterisk for dependence Sensitivity for dependence 86% to 90% Specificity 82% to 87%
SCREENING FOR MENTALHEALTH CONDITIONS More complicated due to diversity ofconditions and symptoms involved Routine screening for the most commonconditions associated with addictions Screening or an initial assessment ofrarer conditions only if there is somesuspicion of a problem
COMMON CO-OCCURRINGMENTAL HEALTH CONDITIONS Affective disorders –depression & mania Anxiety disorders –PTSD, generalized anxiety, phobias,panic attacks Personality disorders –antisocial, obsessive-compulsive,borderline
STRATEGIES FOR MENTALHEALTH SCREENING No simple universal screens due toscope and diversity of conditions Cover key symptoms of commonconditions (e.g., depressed mode for aweek or more, experienced a traumaticevent, etc.) in psychosocial interview Use a structured interview coveringcommon problems – more than ascreen, but time efficient
Preoccupation with quantity of useUse of vague/poorly defined termsAsking clients to make valuejudgmentsOveremphasis on family historyGetting into other treatment issues
PRIORITIES FOR DIAGNOSTIC /PROBLEM ASSESSMENT Focus on DSM-5 diagnostic criteria Document nature and extent ofproblems and conditions Determine if additional assessments orconsultations are required Determine initial appropriateness of theclient for the program options available.
ASSESSMENT vs. THERAPYAssessment goal:Objective data collectionAssessment is NOT therapyComplete assessment firstBuy in is not initially expected orrequiredEngagement can develop based onassessment feedback, that isassessment can be therapeutic
ASSESSMENT PRINCIPLESSimple, direct, concrete questionsLogical, natural flowFriendly, neutral toneMatter-of-fact presumptive wordingMinimal probing on initial interview
INITIAL INTERVIEWREQUIREMENTS Cover all 11 criteria substance usedisorders For MH cover sufficient content to meetminimal diagnostic criteria for commonconditions Use concrete, specific, and unambiguousquestions Document, document, & document
WHY A STRUCTURED INTERVIEW?Eliminates problems caused by illiteracyGuarantees systematic content coverageGet more information in less timeMeasure for judging respondentsconsistency of reportingDocuments specific responsesFacilitates outside verificationFoundation for standard communication
INITIAL INTERVIEW OPTIONSDevelop your own structured interviewtailored to your populationUse a good commercially availableinterview that has sound clinicalproperties and is practical for your useSome combination of a standard tool plusquestions to address unique issues foryour populationTools and procedures for adults may notbe appropriate for adolescents
ADULTS VS. ADOLESCENTSAdults are often more willing to talk aboutsubstance use than mental health issuesAdolescents are typically least willing totalk about substance use but more willingto talk about emotional discomforts andissues other than substancesThe strategy is to begin with what thetypical individual is most open todiscussing and move to more sensitiveissues during the interview
CAAPE: Comprehensive Addictionand Psychological EvaluationUsed in this presentation as an exampleof a structured interviewCharacteristics include:Logical order of inquiryAbility to be administered in 45-50minutesCan be used by people not credentialed inboth MH and SUD for initial informationgathering
CAAPE Order of InquirySubstance use disordersAxis I (all but psychosis)Axis IIPsychosis indications
Axis I Mental Health ConditionsCovered by the CAAPEDepressionManiaPanic disordersAnxiety and phobiasPosttraumatic stress disorderObsessive-compulsive disorder
Axis II Personality DisordersCovered by the CAAPEAntisocial – thoroughly coveredScreening for the sive-compulsive – different fromAxis I condition with similar name
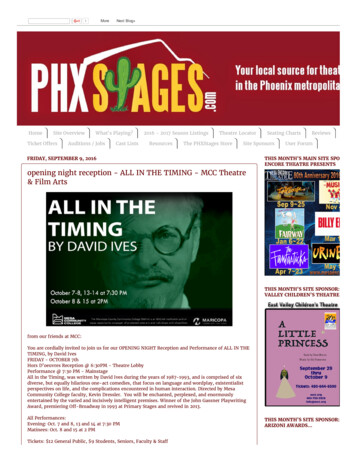
SUDDS-IV Prevalence of SubstanceDependence Among US Inmates80%Any in40%20%0%Adult InmatesN 7682
CAAPE Prevalence of SubstanceDependence Among UK Inmates80%Any ts40%20%0%Adult InmatesN 155
CAAPE PREVALENCE OF SUBSTANCEDEPENDENCE AMONG EVALUATION CASES80%Any ts40%20%0%40 Individuals Evaluated at a TreatmentProgram
PREVALENCE OF PROBABLE AXIS ICONDITIONS AMONG UK INMATES80%DepressionManic episodeBipolar70%60%50%Panic attacksPTSDAny of these40%30%20%10%0%Adult InmatesN 155
AXIS I CONDITIONS AMONG SUBSTANCEDEPENDENT US JAIL INMATES80%70%Depression60%Manic episode50%BipolarPanic attacks40%PTSD30%Any of these20%10%0%Adult InmatesN 176
PROBABLE AXIS I CONDITIONSAMONG TREATMENT CASES80%70%Depression60%Manic episode50%Panic attacks40%PTSD30%Any of these20%10%0%Treatment Convenience SampleN 40
PRESENCE OF PROBABLE AXIS IICONDITIONS AMONG UK endent40%Any of these20%0%Adult InmatesN 155
PROBABLE AXIS II CONDITIONSAMONG DEPENDENT US endent40%Any of these20%0%Adult InmatesN 155
PROBABLE AXIS II CONDITIONS INTREATMENT ndent40%Any of these20%0%Treatment Convenience SampleN 40
CAAPE Findings for ProbableConditions Among Inmates100%80%60%Sub Dep.Axis IAxis II40%20%0%Adult InmatesN 155
CAAPE Findings for ProbableConditions in Treatment Sample80%70%60%50%Sub Dep.Axis IAxis II40%30%20%10%0%Treatment Convenience SampleN 40
ConditionAlcohol DependenceCocaine DependenceMajor DepressionManic EpisodesPanic AttacksPTSDUK US.96.95.91.89.87.78.92.96.94.87.93.87
IMPLICATIONS OF STATISTICSPrevalence for conditions vary frompopulation, but similar patterns emergePrevalence rates of common conditionsprovides rationale for routine preliminaryassessmentInternal consistence reliability is afunction of how uniform or consistent asyndrome a condition presents
CATEGORICAL VS. DIMENSIONALVIEW OF DISORDERSDimensional – symptoms and problemsfall on a continuum – usually in anormal distribution.Categorical – distinct syndromesemerge such that those with a conditionare distinct from those without it.Can have categorical syndromes withvarying levels of severity within each.
Examples of Categorical vs. DimensionalIndications Dimensional distribution: conductdisorder and generalized anxietyand phobic disorders. Categorical distribution: majordepression, manic episodes, andsubstance dependence.
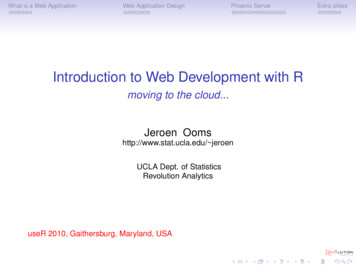
Positive Dependence Criteria ForDependent Cases – SUDDS-IV60CocaineN 854% of Cases5040MarijuanaN 13893020AlcoholN 226510Heroin N 18303456Positive Dependence Criteria7
Positive Abuse Criteria ForAbuse Cases – SUDDS-IV70% of Cases60CocaineN 30350MarijuanaN 9364030AlcoholN 119320Heroin N 32100123Positive Abuse Criteria4
Positive Dependence Criteria For AlcoholDependent Cases60% of Cases50CAAPE UK40CAAPE WI30SUDDS MN201003456Positive Dependence Criteria7
Dependence vs. AbuseMild vs. SevereDependence and abuse are distinctconditions—not just variations in severityThe same will be true for mild vs. severedesignations of the DSM-5Dependence has different prognoses andtreatment goals as compared to abuseDependence is a requirement for residentialplacement according to ASAM PPC-2R
Importance of DocumentingRepeated/Multiple ProblemsThe DSM criteria require a pattern ofuse plus repeated problems related tothe substance in questionThe same problem may occurrepeatedly or different problems maybe associated with a given substanceTo qualify for a diagnosis, problemscannot all be associated with a singleincident
A Word on BlackoutsThe word “blackout” should not be usedin the context of an interview because itis likely to be confused with passing outBlackouts may fit one criteria fordependenceAmnesic periods during or immediatelyafter use are relatively commonThe blackout defined by prolongedfunctioning without later recall are rareand late-stage symptoms
Mental Health ConditionsPrevalent co-occurring conditionsshould be considered on a routinebasesConditions likely to complicatetreatment (e.g., bipolar, PTSD,antisocial personality, borderlinepersonality) should be consideredA clinician does not have to be amental health expert to identify riskindications
Axis I ConditionsMay require treatment independent ofor in concert with addictions treatmentSome conditions may requiremedications for appropriatestabilization (e.g., bipolar disorder)The nature and severity indicated fromthe interview may suggest the type ofprofessional to whom a referral isindicated
Axis II ConditionsCertain conditions may pose behavioralissues beyond those related to addictions(e.g., antisocial personality disorder)Some conditions may be related tomanipulation or instigation of conflicts (e.g.,obsessive-compulsive personality disorderor borderline personality disorder)Individuals with certain conditions may havedifficulty with group situations (e.g., paranoidor schizoid personality disorders)
Use of Findings Within One’sArea of ExpertiseIntegrate results from the assessmentwith other available informationReconcile any contradictory informationif possibleUse specific findings to supportdiagnostic conclusionsUtilize information relevant to treatmentplanning and placement
Use of Findings Outside One’sArea of ExpertiseIntegrate results from the assessmentwith other available informationReconcile any contradictory informationDetermine potential referral issues andthe professional best suited to addressthemUtilize specific findings to support thereferral and to inform the professionalto whom the referral is made
Matter-of-fact presumptive wording . antisocial personality disorder) Some conditions may be related to manipulation or instigation of conflicts (e.g., obsessive-compulsive personality disorder or borderline personality disorder) Individuals with certain conditions may