Transcription
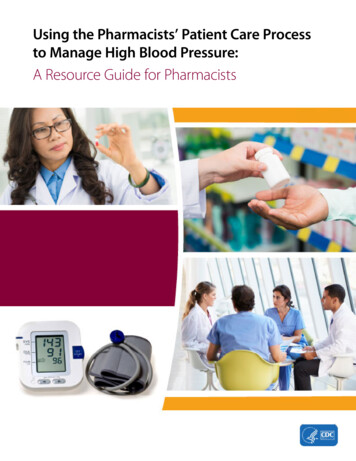
Using the Pharmacists’ Patient Care Processto Manage High Blood Pressure:A Resource Guide for Pharmacists
AcknowledgmentsThis guide was developed by the Division for Heart Disease and Stroke Prevention within the Centers forDisease Control and Prevention and in collaboration with the American Medical Association and the AmericanPharmacists Association (APhA).Contributions to the development and review of this guide were made by Jeffrey M. Durthaler, MS, RPh (IHRC,Inc.); Lauren Taylor, BS (Oak Ridge Institute for Science and Education guest researcher); Stacia Spridgen,PharmD, Anne Burns, BSPharm, and Lindsay Kunkle, PharmD (APhA); Michael Rakotz, MD, and Kathleen A.Heneghan, MPH (American Medical Association); Marialice Bennett, RPh, FAPhA (Ohio State University Collegeof Pharmacy); and Mary Ann Kliethermes, PharmD (Midwestern University College of Pharmacy).Suggested CitationCenters for Disease Control and Prevention. Using the Pharmacists’ Patient Care Process to Manage High BloodPressure: A Resource Guide for Pharmacists. Atlanta, GA: Centers for Disease Control and Prevention,U.S. Department of Health and Human Services; 2016.Website addresses of nonfederal organizations are provided solely as a service to our readers. Provision of anaddress does not constitute an endorsement by the Centers for Disease Control and Prevention (CDC) or thefederal government, and none should be inferred. CDC is not responsible for the content of other organizations’web pages.
ContentsIntroduction . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1Background . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1About This Resource Guide . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 2Pharmacists’ Patient Care Process . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3Overview . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3Using the Pharmacists’ Patient Care Process to Manage High Blood Pressure . . . . . . . . . . . . . . 5High Blood Pressure . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6Overview . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6Importance of Measuring Blood Pressure Accurately . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7How to Use the Pharmacists’ Patient Care Process to Manage High Blood Pressure . . . . . . . . . . . 10Step 1: Collect . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 10Step 2: Assess . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 12Step 3: Plan . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13Step 4: Implement . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15Step 5: Follow-Up: Monitor and Evaluate . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16Quality Measures of Value: A Population Health Approach . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 18References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20iii
IntroductionBackgroundHeart disease and stroke are leadingcauses of death and disability inthe United States, according tothe American Heart Association.1In this country, someone has aheart attack every 42 seconds,someone dies of a heart attackevery minute, someone has a strokeevery 40 seconds, and someonedies of a stroke every 4 minutes.1People can protect themselvesfrom heart disease and stroke inmany ways. For example, theycan reduce their risk by makinglifestyle changes such as:y Maintaining a healthy weight.y Being more physically active.y Eating more fruits, vegetables,whole grains, fish, and lowfat dairy products.y Consuming less sodium,sugar, animal fat, sugarydrinks, and alcohol.y Avoiding or stopping smoking.yy Keeping medical appointmentsto monitor their bloodpressure if it is high.yy Taking medicines if theyare prescribed.In addition, people can increasetheir chances of living longerand reduce damage to theirhearts and brains by knowing thewarning signs of heart attack andstroke and by understanding theimportance of calling 911 for helpright away when these signs occur.yy Participating in team-basedcare and collaborativepractice agreements.Health care professionals alreadyplay a critical role in reducing heartdisease and preventing stroke inthe United States, but more can bedone. Pharmacists specifically havea unique opportunity to have aneffect on outcomes associated withheart disease and stroke. Communitypharmacists can help by beingproactive in identifying the needsof their patients and taking actionto influence healthy behaviors.yy Embracing qualityimprovement initiatives.People can also reduce their risk by:Pharmacists can have a positiveeffect on population health by:yy Checking and keeping theirblood pressure and cholesterollevels under control.yy Creating community awarenessabout heart disease and stroke.yy Talking with health careprofessionals like doctors andnurses about their blood pressure.people who are not adheringto prescribed drug treatments,helping patients take theirmedications correctly, andscreening for uncontrolled andundiagnosed high blood pressure.yy Providing patient care servicessuch as encouraging lifestylemodifications and selfmanagement, counselingyy Using clinical protocols.yy Supporting e-prescribing withbidirectional messaging betweenpharmacist and prescriber toimprove medication management.yy Participating in continuingeducation programs.yy Getting certifications in chronicdisease management.About This Resource GuideThe Centers for Disease Control andPrevention’s (CDC’s) Division forHeart Disease and Stroke Preventionrecognizes the contribution thatcommunity pharmacists can maketo improve population health. CDCdeveloped this publication, Usingthe Pharmacists’ Patient Care Processto Manage High Blood Pressure: AResource Guide for Pharmacists, as acall to action to use the Pharmacists’Patient Care Process2 as a way toIntroduction 1
prevent and manage high bloodpressure through team-based care,with the goal of reducing heartdisease and stroke in the UnitedStates. It compiles informationabout current resources andemerging practices, as well as toolsand examples that pharmacistscan use to help them improvehealth outcomes associatedwith cardiovascular disease.Pharmacists are encouraged topartner with their state or localhealth departments, communityhealth workers, doctors, andother health care professionalsto understand the prevalenceof high blood pressure in theircommunities and learn how tohelp people manage this condition.CDC believes that by doing so,pharmacists will ultimately beable to practice their professionat the top of their training, whichwill help improve cardiovascularhealth in the United States.This resource guide also providesan overview of high blood pressure,a discussion of the importanceof accurate measurements,and guidance on how to take apatient’s blood pressure. The finalsection outlines the five stepsof the Pharmacists’ Patient CareProcess and provides suggestionson how these steps can beapplied to managing high bloodpressure. References and web linksfor resources that support thesuggested actions are also provided.CDC acknowledges that thescope of services associated withmanaging high blood pressurewill vary among pharmacists andpharmacy practices—from thebasics of screening to blood pressuremonitoring to comprehensivemanagement. Thus, the actionstaken and the resources usedwill also vary, depending on thescope of the services provided.Introduction 2
Pharmacists’ Patient Care ProcessOverviewIn 2014, the Pharmacists’ PatientCare Process was released by theJoint Commission of PharmacyPractitioners, and it is endorsed by13 national pharmacy organizations.2This process promotes a consistentapproach to patient care deliveryin any pharmacy practice setting.Multiple strategies are beingused to support and promoteuse of the Pharmacists’ PatientCare Process. For example, it hasbeen incorporated into the 2016Accreditation Council for PharmacyEducation (ACPE) accreditationstandards and key elements for theprofessional program in pharmacyleading to the Doctor of Pharmacydegree, and continuing educationproviders are being encouragedto include it in educationalprograms for pharmacists. ThePharmacists’ Patient Care Processis also being incorporated intothe ASHP accreditation standardfor postgraduate year one (PGY1)pharmacy residency programs andthe ASHP accreditation standardfor postgraduate year two (PGY2)pharmacy residency programs.Joint Commission of Pharmacy Practitionersyy Academy of Managed Care Pharmacyyy American Society of Consultant Pharmacistsyy Accreditation Council forPharmacy Educationyy American Society ofHealth-System Pharmacistsy American Association ofColleges of Pharmacyyy National Alliance of StatePharmacy Associationsy American College of Apothecaries yy National Association ofBoards of Pharmacyy American College ofyy National Community ClinicalPharmacy Pharmacists Associationy American Pharmacists AssociationIn addition, the process is being usedas a framework for the developmentof structured electronic patient caredocuments that pharmacists canshare electronically with other healthcare professionals. Quality measuresrelated to the use of the Pharmacists’Patient Care Process are beingconsidered by the Pharmacy QualityAlliance as part of its quality measuredevelopment process. At theindividual practice level, pharmacistsare encouraged to embraceboth the foundational elementsand the specific five steps of thePharmacists’ Patient Care Process.As part of this process, pharmacistsuse a patient-centered approachin collaboration with other healthcare professionals on a patient’shealth care team to optimizepatient health and medicationoutcomes.2 An essential first step inthis approach is the establishmentof a patient-pharmacist relationshipthat supports engagement andeffective communication withpatients, families, and caregiversthroughout the process. At the coreof the process, pharmacists also mustdocument activities and continuallyPharmacists’ Patient Care Process 3
collaborate and communicatewith doctors, other pharmacists,and other health care professionalsto provide safe, effective, andcoordinated care (Figure 1). Thisprocess is further enhanced bythe use of information technologysystems that allow for efficient andeffective documentation of activitiesand communication among allindividuals involved in patient care.Figure 1. Pharmacists’ Patient Care ProcessPharmacists use a patient-centered approachin collaboration with other providers on thehealth care team to optimize patient healthand medication outcomes.Pharmacists’ Patient Care ProcessCollaborate Communicate DocumentUsing principles of evidence-based practice, pharmacists:Collect: The pharmacist assures the collection of the necessarysubjective and objective information about the patient inorder to understand the relevant medical/medicationhistory and clinical status of the patient.Assess: The pharmacist assesses theinformation collected and analyzes the clinicaleffects of the patient’s therapy in the contextof the patient’s overall health goals in orderto identify and prioritize problems andachieve optimal care.Plan: The pharmacist develops anindividual patient-centered care plan,in collaboration with other health careprofessionals and the patient or caregiver that isevidence-based and cost-effective.Follow-up:Monitor mentImplementPlanImplement: The pharmacist implements the care plan incollaboration with other health care professionals and the patientor caregiver.Follow-up: Monitor and Evaluate: The pharmacist monitors and evaluatesthe effectiveness of the care plan and modifies the plan in collaboration withother health care professionals and the patient or caregiver as needed.Source: Joint Commission of Pharmacy Practitioners. The Pharmacists’ Patient Care Process.Pharmacists’ Patient Care Process 4
Using the Pharmacists’Patient Care Processto Manage HighBlood PressureThe primary objective of thisguide is to align the efforts ofpharmacists with current nationalinitiatives designed to improve thecardiovascular health of the UnitedStates by controlling blood pressureamong the adult population. ThePharmacists’ Patient Care Processis recommended as a strategy toachieve this goal, in collaborationwith doctors and other healthcare professionals through teambased care. The success of theseefforts will depend largely onthree factors: the adoption of apopulation health perspective,the use of health informationtechnology to improve medicationmanagement, and the sustainabilityof cardiovascular pharmacy services.Adopting a PopulationHealth PerspectiveAlthough the Pharmacists’ PatientCare Process is designed to beindividualized, the current andevolving health care environmentcalls for all health care practitionersto also adopt a population healthperspective. Pharmacists must seekto understand the epidemiologyof cardiovascular disease in thepopulations they serve and toprovide services in ways that reducechronic disease and promotehealth and wellness.3,4 Becauseof their combination of access,skills, and services, pharmacistsare uniquely positioned andqualified to respond to the healthneeds of their communities.Accessing Patient InformationThe Pharmacists’ Patient CareProcess is largely dependenton collecting necessary patientinformation. Pharmacists mustcollate information submitted bypatients (e.g., medical history forms);obtained from direct interactionswith other health care professionals(e.g., by phone, fax, or in person);obtained electronically from theinterconnectivity of the pharmacyand patients’ electronic healthrecords (EHRs); and obtained throughdirect, face-to-face interactionswith patients. Pharmacists areencouraged to start where theyare with the resources they haveand begin moving their practicetoward the most efficient processfor collecting patient information.In many cases, this change willrequire developing formal datasharing agreements with doctors,hospitals, and health care systems.5Sustaining CardiovascularPharmacy ServicesShort-term and long-term successdepends on payment models thatsustain the use of the Pharmacists’Patient Care Process for themanagement of high blood pressure.Although resolving the paymentand reimbursement issues thatface clinical pharmacy practice arebeyond the scope of this resourceguide, pharmacists are encouragedto partner with payers, health careproviders, and peers to explore,discuss, and learn about existingand emerging payment models.6Pharmacists’ Patient Care Process 5
High Blood PressureOverviewOne in three Americans hashigh blood pressure (also calledhypertension), and it is morecommon among some populationgroups, including African Americansand adults older than 60.7 Highblood pressure is the second mostcommon reason for U.S. adultsto visit their doctors, and it isresponsible for more than 34 millionoffice visits each year.8 In 2016, theestimated direct and indirect cost ofhigh blood pressure in the UnitedStates was 48.6 billion.1 Chronichigh blood pressure can cause heartdisease, stroke, kidney disease, andblindness.7 In 2016, the economiccosts of heart disease and strokewere estimated at 316.6 billion,including 193.1 billion in directmedical expenses and 123.5 billionin indirect costs.1to reduce premature disease anddeath from cardiovascular disease.Studies have shown that a 12- to13-point reduction in blood pressureamong those with high bloodpressure can reduce the number ofheart attacks by 21%, strokes by 37%,and all deaths from cardiovasculardisease by 25%.9The U.S. Preventive Services TaskForce recommends that cliniciansscreen adults 18 years or older forhigh blood pressure.10,11 Studies haveshown that clinical, economic, andquality-of-life outcomes improvewhen pharmacists routinely screenpatients for blood pressure controland medication adherence as part ofteam-based care.12Goals and TreatmentBlood pressure should be measuredby health care professionals in everyclinical encounter for adults aged18 or older.12 Lifestyle modificationand self-management counselingshould be provided to patientswith high blood pressure. Cliniciansshould also help patients set bloodpressure goals and should prescribeBenefits of Blood PressureScreening and ControlOf the 34 million Americans whohave uncontrolled high bloodpressure, about 11 million (1 in3) are not aware that they havethis condition and are not takingmedication to control it.8 Controllingblood pressure with medications isone of the most cost-effective waysHigh Blood Pressure 6
medications based on the mostcurrent hypertension treatmentprotocols and guidelines. Routineoffice visits should be scheduledto synchronize medication therapyand monitor high blood pressureand treatment efforts.13,14 A teambased disease managementprogram should be used totrack and monitor patients withhigh blood pressure and helpprevent and manage comorbidconditions such as diabetes.15,16Barriers to Achieving BloodPressure GoalsStudies have found that severalbarriers can prevent people frommeeting their blood pressuregoals,17–25 including the following:yy Clinical inertia.yy Medication cost.yy Lack of awareness.yy Lack of access to care.yy Medication side effects.yy Medication nonadherence.yy Masked high blood pressure.yy White coat high blood pressure.yy Lack of standardizedtreatment protocols.yy Inaccurate blood pressuremeasurements.yy Challenges in making healthylifestyle changes.yy Beliefs and attitudes about highblood pressure.Importance of MeasuringBlood Pressure AccuratelyThe control of blood pressure beginswith an accurate measurementleading to a correct diagnosis,effective treatment, routinemonitoring, and medicationadherence. For more than a century,the mercury sphygmomanometerwas the gold standard for measuringblood pressure.26 A combination ofnew technology (i.e., electronic ordigital equipment) and concernsfor the environment has led to thereplacement of this device. However,the accuracy of new technology andthe prevalence of white coat andmasked high blood pressure haveraised concern about the quality ofblood pressure measurements.26Inaccurate blood pressuremeasurements have significantpublic health implications becauseminor errors can result in themisdiagnosis of millions of people.According to one analysis, a 5 mm Hgunderestimate of blood pressurecould lead to 21 million people beingmislabeled as having high normalblood pressure ratherthan high blood pressure, resultingin a missed opportunity formedication treatment.26 Similarly,a 5 mm Hg overestimate couldresult in 27 million people beingHigh Blood Pressure 7
misdiagnosed with high bloodpressure, which would expose themto unnecessary treatment and thepotential for adverse events.26 Theseconcerns are compounded by theeffects of white coat and maskedhigh blood pressure and the fact thatthe indirect measurement of bloodpressure is the only practical way toidentify high blood pressure.26Common sources of error in bloodpressure measurements includehuman errors (e.g., incorrect cuffsize, improper body positioning,inadequate rest period, terminaldigit preference, lack of repeatmeasurements), patient factors(e.g., recent caffeine, decongestant,or nicotine use; talking during themeasurement), and device-relatedfactors (e.g., failure to properly use,inspect, maintain, or calibrate adevice validated by the AmericanNational Standards Institute,Association for the Advancementof Medical Instrumentation, orInternational Organization forStandardization).26 Pharmacistsshould be aware of these problems,and efforts are ongoing toaddress them. Resource 1 offersrecommendations for improvingthe accuracy of blood pressuremeasurements for self-monitoringblood pressure devices, includingpharmacy kiosks. Resource 2offers guidance for pharmacistson how to measure a patient’sblood pressure correctly.Resource 1. How to Improve the Accuracy of Self-Monitoring Blood Pressure DevicesFor Home Monitors, Pharmacists Should:For Pharmacy Kiosks, Pharmacists Should:yy Recommend monitors with the following features:automated; upper arm cuff; validated by ANSI, AAMI,or ISO;* memory storage capacity; accuracy checkedby doctor, pharmacist, or nurse after purchase.27yy Only use clinically validated blood pressure kiosksand routinely calibrate and maintain them.yy Instruct patient through verbal and visualcommunication on correct body position andoperating procedures for the device, includingroutine calibration and maintenance.28yy Evaluate appropriate use of monitor, reviewstored blood pressure measures, and assessmedication adherence at time of refill ofantihypertensive medication.29yy Encourage patient to use kiosk at time of refill of antihypertensive medication. Instruct patient throughverbal and visual communication oncorrect body position and operating proceduresfor the device.yy Implement technology to automatically transmitdata from kiosk to pharmacy computer system.30–33yy Evaluate blood pressure measures, assess medicationadherence, and take action as appropriate.*American National Standards Institute, Association for the Advancement of Medical Instrumentation, or International Organization for Standardization.High Blood Pressure 8
Resource 2. How to Monitor and Record Blood Pressure*Before you measure a patient’s bloodpressure, note that differences betweenleft arm and right arm (or “interarm”)blood pressure are common. Severalstudies have been done to determinethe “normal” variation between theright and left arms. In general, anydifference of 10 mm Hg or less isconsidered normal and not a cause forconcern. Some studies have shownthat the average interarm systolic bloodpressure difference is significantlyhigher in patients with coronary arterydisease. For this reason, it’s a good ideato discuss differences higher than10 mm Hg with a patient’s primarycare provider.When you take a patient’s bloodpressure for the first time, it’srecommended that you take it in botharms. If the patient is taking his or herblood pressure at home, readings areeasier to take in the nondominant arm.If the patient’s home blood pressurereadings are different from thosetaken in the pharmacy, discuss thisdifference with the patient’s primarycare provider.Many factors affect blood pressure.Interarm differences emphasize theimportance of measuring bloodpressure in both arms initially toprevent misdiagnosis of high bloodpressure. If one arm consistently hashigher blood pressure than the other,that arm should be used to measurethe patient’s blood pressure.Make sure the cuff fits.Measure around the patient’s upperarm and choose a monitor with thecorrect size cuff.Make sure the patient is still.Patients should not smoke,drink caffeinated beverages, orexercise within 30 minutes beforemeasurement.Make sure the patient sits correctly.Patients should sit with their backstraight and supported. Their feetshould be flat on the floor, and theirlegs should not be crossed. Their armsshould be supported on a flat surface(such as a table) with the upper armat heart level. Make sure the middle ofthe cuff is placed directly above theeye of the elbow. Check the monitor’sinstructions for an illustration ofappropriate use.Take multiple readings.Each time you take a patient’s bloodpressure, take two or three readings1 minute apart, and record all the results.Measure at the same time daily.It’s important to take the readingsat the same time each day, such asmorning and evening.Accurately record all results.Record all readings, including the dateand time taken. Share blood pressurerecords with other members of thepatient’s health care team.Understand the readings.Optimal blood pressure is less than120/80 mm Hg (systolic pressure is lessthan 120 and diastolic pressure is lessthan 80). Read Understanding BloodPressure Readings to learn moreabout what the numbers mean.Consult the patient’s primarycare provider if you get severalhigh readings.A single high reading of blood pressureis not an immediate cause for alarm.However, if you get a high reading,take the patient’s blood pressureseveral times, make sure the monitoris working properly, and consult thepatient’s primary care provider todiscuss next steps. When the systolic(top number) reading is 180 or higheror the diastolic (bottom number)reading is 110 or higher, emergencymedical treatment is required forevaluation and treatment. SeeHypertensive Crisis.Watch the How to Measure BloodPressure video.An instructional video isavailable online.*Adapted from American Heart Association’s How to Monitor and Record Your Blood Pressure website.High Blood Pressure 9
How to Use the Pharmacists’ Patient CareProcess to Manage High Blood PressureAlthough the Pharmacists’ PatientCare Process can be used to addressany disease, this guide is designedto show pharmacists how to helppatients manage high bloodpressure. This section describes eachof the five steps of the Pharmacists’Patient Care Process and suggestsspecific actions that pharmacistscan take. These actions will vary inapplication and intensity dependingon the patient care service provided.This section also provides referencesand web links for resources thatsupport the suggested actions.For all of the services they provide,pharmacists should recognize that aholistic, patient-centered approachcan be beneficial. Patients with highblood pressure often have otherconditions, such as diabetes andhigh cholesterol. Pharmacists usingthe Pharmacists’ Patient Care Processto address high blood pressureshould prioritize their serviceswhile also working to address allof their patients’ medication needsand health problems, rather thanfocusing solely on one condition.Although the primary goalmay be to manage high bloodpressure, pharmacists should alsoconsider the whole patient.The five steps of the Pharmacists’Patient Care Process are:yy Step 1: Collect.yy Step 2: Assess.yy Step 3: Plan.yy Step 4: Implement.yy Step 5: Follow-Up: Monitorand Evaluate.Step 1: CollectThe first step in the Pharmacists’Patient Care Process as it relates to themanagement of high blood pressureis to collect the necessary medical,medication, and lifestyle history ofthe patient, as well as informationfrom physical assessments andbiometric tests. This information(e.g., blood pressure measurements)can be collected by the patient, thepharmacist, or other health careprofessionals. When possible, thisinformation should link to the patients’EHR.5 Possible data points to collect(based on the services provided) arelisted here, along with references andweb links where appropriate.COLLECTThe pharmacist assures thecollection of necessary subjectiveand objective informationabout the patient in order tounderstand the relevant medical/medication history and clinicalstatus of the patient. Informationmay be gathered and verifiedfrom multiple sources, includingexisting patient records, thepatient, and other health careprofessionals. This processincludes collecting:A current medicationlist and medication usehistory for prescription andnonprescription medications,herbal products, and otherdietary supplements.Relevant health data that mayinclude medical history, healthand wellness information,biometric test results, andphysical assessment findings.Patient lifestyle habits,preferences and beliefs, healthand functional goals, andsocioeconomic factors thataffect access to medicationsand other aspects of care.How to Use the Pharmacists’ Patient Care Process to Manage High Blood Pressure 10
Medical Historyyy Age.yy Sex.yy Race.yy Fall risk.34,35yy Heart age.36yy Blood pressure.yy Immunization status.yy Past surgeries and procedures.yy Current diagnoses, treatmentplans, and therapy goals.yy Family medical history(e.g., heart disease, stroke,diabetes, high cholesterol).Results of Physical Assessmentand Biometric Testsyy Body mass index: Body massindex calculator.yy Resting heart rate: Medical History and PhysicalExam for High Heart Rate. Medical History and PhysicalExam for Slow Heart Rate.yy Presence of edema (swelling).yy Understanding laboratory testsand Chemistry Panels.yy Adverse events.Note: Laboratory tests shouldbe based on patient- andmedication-specific factors.yy Adherence and persistence.37Medication Historyyy Attitude, beliefs, and medicationtaking behaviors.yy Current blood pressure: PhysicalExam for High Blood Pressure.yy Name.yy Laboratory tests (e.g., Electrolytes,Lipid Profile, Liver Panel, RenalPanel, Hemoglobin A1c, BasicMetabolic Panel, ComprehensiveMetabolic Panel).yy Route.yy Dose.yy Purpose.yy Frequency.yy Administration time.yy Awareness and knowledge ofmedications.yy Pharmacist Drug Adherence Workup Tool (DRAW).Note: Other medications, over-the-counterproducts, and dietary supplements shouldalso be reviewed.yy Effectiveness.How to Use the Pharmacists’ Pati
to prescribed drug treatments, helping patients take their medications correctly, and screening for uncontrolled and undiagnosed high blood pressure. . Resource Guide for Pharmacists, as a call to action to use the Pharmacists’ Patient Care Process. 2. as a w