Transcription
Clinical PracticeGuidelinesforQualityPalliative Care4th edition
Publisher:National Coalition for Hospice and Palliative CareClinical Practice Guidelines for Quality Palliative Care, 4th editionCopyright 2018 National Coalition for Hospice and Palliative CareThis publication is copyrighted. We are making such material available in our efforts to advanceunderstanding of issues related to hospice and palliative care. No part of this publication may bereproduced, stored in a retrieval system, or transmitted in any form or by any means, mechanical,electronic, photocopying, recording or otherwise, without prior written permission of the publisher.Disclaimer: The National Coalition for Hospice and Palliative Care assumes no responsibility or liabilityfor any errors or omissions in the National Consensus Project’s Clinical Practice Guidelines for QualityPalliative Care, 4th edition. The information contained is provided on an “as is” basis with no guaranteesof completeness, accuracy, usefulness or timeliness and without any warranties of any kind whatsoever,express or implied. The information is intended for non-commercial use for the user who accepts fullresponsibility for its use. While the National Coalition for Hospice and Palliative Care has taken everyprecaution to ensure that the content is current and accurate, errors can occur.Adherence to these guidelines will not ensure successful treatment in every situation. Furthermore,these guidelines should not be interpreted as setting a standard of care, considered to be medicaladvice, or be deemed inclusive of all proper methods of care nor exclusive of other methods of carereasonably directed to obtaining the same results. The ultimate judgment regarding the propriety ofany specific therapy must be made by the physician and/or health care provider and the patient in lightof all the circumstances presented by the individual patient, and the known variability and biologicalbehavior of the disease. These guidelines reflect the best available data and information at the time theguidelines were prepared. The results of future studies may require revisions to the recommendationsin these guidelines to reflect new data or information.ISBN # 978-0-692-17943-7For information, contact:National Coalition for Hospice and Palliative CareP.O. Box 29709Richmond, VA ww.nationalcoalitionhpc.org/ncpSuggested Citation:National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality PalliativeCare, 4th edition. Richmond, VA: National Coalition for Hospice and Palliative Care; 2018. https://www.nationalcoalitionhpc.org/ncp.
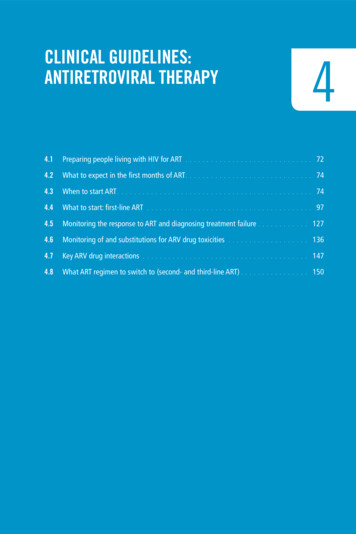
Table of ContentsForeword . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . iPalliative Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . iHistory of the National Consensus Project’s Guidelines . . . . . . . . . . . . . . . . . . . . . . iiiNCP Guidelines, 4th edition . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . vIntroduction to the 4th edition . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . viiSummary of Key Revisions in Each Domain . . . . . . . . . . . . . . . . . . . . . . . . . . . . viiiSystematic Review of Key Research Evidence . . . . . . . . . . . . . . . . . . . . . . . . . . . ixKey Concepts / Definitions . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . ixUsing the NCP Guidelines . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .xConclusion . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . xiAcknowledgments . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . xiiDomain 1: Structure and Processes of Care . . . . . . . . . . . . . . . . . . . . . . . . . 1Guideline 1.1Interdisciplinary Team . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .1Guideline 1.2Comprehensive Palliative Care Assessment . . . . . . . . . . . . . . . . . . . 2Guideline 1.3Palliative Care Plan . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .3Guideline 1.4Continuity of Palliative Care . . . . . . . . . . . . . . . . . . . . . . . . . . . 5Guideline 1.5Care Settings . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .5Guideline 1.6Interdisciplinary Team Education . . . . . . . . . . . . . . . . . . . . . . . . .6Guideline 1.7Coordination of Care and Care Transitions . . . . . . . . . . . . . . . . . . . .7Guideline 1.8Emotional Support to the Interdisciplinary Team . . . . . . . . . . . . . . . . .7Guideline 1.9Continuous Quality Improvement . . . . . . . . . . . . . . . . . . . . . . . . 7Guideline 1.10Stability, Sustainability, and Growth . . . . . . . . . . . . . . . . . . . . . . . 8Clinical and Operational Implications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 8Essential Palliative Care Skills Needed by All Clinicians . . . . . . . . . . . . . . . . . . . . . . .9Key Research Evidence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .9Practice Examples . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 9Domain 2: Physical Aspects of Care . . . . . . . . . . . . . . . . . . . . . . . . . . . .Guideline 2.1Global . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 13Guideline 2.2Screening and Assessment . . . . . . . . . . . . . . . . . . . . . . . . . . . 14Guideline 2.3Treatment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14Guideline 2.4Ongoing Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 15Clinical and Operational Implications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16Essential Palliative Care Skills Needed by All Clinicians . . . . . . . . . . . . . . . . . . . . . . 16Key Research Evidence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 16Practice Examples . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1713
Table of ContentsDomain 3: Psychological and Psychiatric Aspects of Care . . . . . . . . . . . . . . . . . 20Guideline 3.1Global . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 20Guideline 3.2Screening and Assessment . . . . . . . . . . . . . . . . . . . . . . . . . . . 21Guideline 3.3Treatment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 22Guideline 3.4Ongoing Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 23Clinical and Operational Implications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 23Essential Palliative Care Skills Needed by All Clinicians . . . . . . . . . . . . . . . . . . . . . . 23Key Research Evidence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 24Practice Examples . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 24Domain 4: Social Aspects of Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26Guideline 4.1Global . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 26Guideline 4.2Screening and Assessment . . . . . . . . . . . . . . . . . . . . . . . . . . . 27Guideline 4.3Treatment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28Guideline 4.4Ongoing Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 28Clinical and Operational Implications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29Essential Palliative Care Skills Needed by All Clinicians . . . . . . . . . . . . . . . . . . . . . . 29Key Research Evidence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 29Practice Examples . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 30Domain 5: Spiritual, Religious, and Existential Aspects of Care . . . . . . . . . . . . . .Guideline 5.1Global . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 32Guideline 5.2Screening and Assessment . . . . . . . . . . . . . . . . . . . . . . . . . . . 33Guideline 5.3Treatment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 34Guideline 5.4Ongoing Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3432Clinical and Operational Implications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 35Essential Palliative Care Skills Needed by All Clinicians . . . . . . . . . . . . . . . . . . . . . . 35Key Research Evidence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 35Practice Examples . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 35Domain 6: Cultural Aspects of Care . . . . . . . . . . . . . . . . . . . . . . . . . . . .Guideline 6.1Global . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 38Guideline 6.2Communication and Language . . . . . . . . . . . . . . . . . . . . . . . . . 39Guideline 6.3Screening and Assessment . . . . . . . . . . . . . . . . . . . . . . . . . . . 40Guideline 6.4Treatment . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 41Clinical and Operational Implications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 42Essential Palliative Care Skills Needed by All Clinicians . . . . . . . . . . . . . . . . . . . . . . 42Key Research Evidence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 42Practice Examples . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4338
Table of ContentsDomain 7: Care of the Patient Nearing the End of Life . . . . . . . . . . . . . . . . . .Guideline 7.1Interdisciplinary Team . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 45Guideline 7.2Screening and Assessment . . . . . . . . . . . . . . . . . . . . . . . . . . . 46Guideline 7.3Treatment Prior to Death . . . . . . . . . . . . . . . . . . . . . . . . . . . . 47Guideline 7.4Treatment During the Dying Process and Immediately After Death . . . . . . 47Guideline 7.5Bereavement . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 4845Clinical and Operational Implications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 49Essential Palliative Care Skills Needed by All Clinicians . . . . . . . . . . . . . . . . . . . . . . 49Key Research Evidence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 50Practice Examples . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 50Domain 8: Ethical and Legal Aspects of Care . . . . . . . . . . . . . . . . . . . . . . .Guideline 8.1Global . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 52Guideline 8.2Legal Considerations . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 53Guideline 8.3Screening and Assessment . . . . . . . . . . . . . . . . . . . . . . . . . . . 55Guideline 8.4Treatment and Ongoing Decision-Making . . . . . . . . . . . . . . . . . . . 5652Clinical and Operational Implications . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 57Essential Palliative Care Skills Needed by All Clinicians . . . . . . . . . . . . . . . . . . . . . . 57Key Research Evidence . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 57Practice Examples . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 57Appendix I: Glossary . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 60Appendix II: Tools and Resources . . . . . . . . . . . . . . . . . . . . . . . . . . . . .70Domain 1: Structure and Processes of Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . 70Domain 2: Physical Aspects of Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 71Domain 3: Psychological and Psychiatric Aspects of Care . . . . . . . . . . . . . . . . . . . . . 74Domain 4: Social Aspects of Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 75Domain 5: Spiritual, Religious, and Existential Aspects of Care . . . . . . . . . . . . . . . . . . 76Domain 6: Cultural Aspects of Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 77Domain 7: Care of the Patient Nearing the End of Life . . . . . . . . . . . . . . . . . . . . . . 78Domain 8: Ethical and Legal Aspects of Care . . . . . . . . . . . . . . . . . . . . . . . . . . . 79Appendix III: Contributors . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 85
Table of ContentsAppendix IV: Scoping Review . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .87Scoping Review Methodology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 87Review and Inclusion Process . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 90Domain 1: Structure and Processes of Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . 90Domain 2: Physical Aspects of Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 113Domain 3: Psychological and Psychiatric Aspects of Care . . . . . . . . . . . . . . . . . . . . 126Domain 4: Social Aspects of Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 132Domain 5: Spiritual, Religious, and Existential Aspects of Care . . . . . . . . . . . . . . . . . 136Domain 6: Cultural Aspects of Care . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 142Domain 7: Care of the Patient Nearing the End of Life . . . . . . . . . . . . . . . . . . . . . 152Domain 8: Ethical and Legal Aspects of Care . . . . . . . . . . . . . . . . . . . . . . . . . . 158Appendix V: Endorsing and Supporting Organizations . . . . . . . . . . . . . . . . . . 165A systematic review of the evidence for the NCP Guidelines, 4th edition, was conducted by theRAND Evidence-based Practice Center. The complete findings are published online in the Journalof Pain and Symptom Management (doi: 10.1016/j.jpainsymman.2018.09.008).
ForewordIndividuals who are seriously ill need care that is seamless acrosssettings, can rapidly respond to needs and changes in healthstatus, and is aligned with patient-family preferences and goals.Patients of all ages, living in all areas of the country, have unmetcare needs that cause a burden on families and the US health caresystem.In this document, seriousillness is defined as “a healthcondition that carries a highrisk of mortality and eithernegatively impacts a person’sdaily function or quality oflife or excessively strains theircaregiver” (Kelley and BollensLund, 2018).Providing “crisis-care” to individuals with a serious illness whoseongoing care needs are poorly managed has resulted in increasedhealth care spending that does not necessarily improve quality oflife. Care of individuals with serious illness is often “marked byinadequate symptom control and low patient and family perceptionsof the quality of care; and potentially discordant with personal goals and preferences.”1 Patients withserious illness and their family caregivers are seldom able to have their care needs reliably met, leadingto symptom exacerbation crises and emergency department visits and/or repeated hospitalizations.2Palliative CarePalliative care focuses on expert assessment and management of pain and other symptoms, assessmentand support of caregiver needs, and coordination of care. Palliative care attends to the physical, functional,psychological, practical, and spiritual consequences of a serious illness. It is a person- and family-centeredapproach to care, providing people living with serious illness relief from the symptoms and stress of anillness. Through early integration into the care plan for the seriously ill, palliative care improves quality oflife for the patient and the family.Palliative care is: Appropriate at any stage in a serious illness, and it is beneficial when provided along with treatmentsof curative or life-prolonging intent. Provided over time to patients based on their needs and not their prognosis. Offered in all care settings and by various organizations, such as physician practices, health systems,cancer centers, dialysis units, home health agencies, hospices, and long-term care providers. Focused on what is most important to the patient, family, and caregiver(s), assessing their goals andpreferences and determining how best to achieve them. Interdisciplinary to attend to the holistic care needs of the patient and their identified family andcaregivers.Palliative care principles and practices can be delivered by any clinician caring for the seriously ill,and in any setting. All clinicians are encouraged to acquire core skills and knowledge regarding palliativecare and refer to palliative care specialists as needed. Analogous to the management of hypertensionand heart disease by primary clinicians who may turn to cardiologyspecialists and clinical practice guidelines for consultation orNote: Words bolded in redmanagement of more complex cases, specialist level palliativeare defined in the Glossary.Clinical Practice Guidelines for Quality Palliative Care, 4th editioni
Forewordcare is available for consultation, teaching, research, and care of the most complex patients living witha serious illness. Specialist level palliative care is delivered through an interdisciplinary team with theprofessional qualifications, training, and support needed to deliver optimal patient- and family-centeredcare.Recognizing the changes to the practice of palliative care in all care settings, the National ConsensusProject for Quality Palliative Care defines palliative care as follows:Beneficial at any stage of a serious illness, palliative care is an interdisciplinary care delivery systemdesigned to anticipate, prevent, and manage physical, psychological, social, and spiritual suffering tooptimize quality of life for patients, their families and caregivers. Palliative care can be delivered inany care setting through the collaboration of many types of care providers. Through early integrationinto the care plan of seriously ill people, palliative care improves quality of life for both the patientand the family.In addition, specific definitions of palliative care are applicable depending on the audience and contextwithin which the definition is used:The 2015 Dying in America: Improving Quality and HonoringIndividual Preferences Near the End of Life report definespalliative care as, “Care that provides relief from pain andother symptoms, supports quality of life, and is focused onpatients with serious advanced illness and their families.Palliative care may begin early in the course of treatment fora serious illness and may be delivered in a number of waysacross the continuum of health care settings, including in thehome, nursing homes, long-term acute care facilities, acutecare hospitals, and outpatient clinics.”3 The report explicitlystates that care outcomes are optimized when palliative carebegins early after the diagnosis of a serious illness, is deliveredat the same time as curative or disease-modifying treatments,and is available in all settings where patients and families needcare.4The Centers for Medicare and Medicaid Services definespalliative care as, “patient and family centered care thatoptimizes quality of life by anticipating, preventing, andtreating suffering. Palliative care throughout the continuumof illness involves addressing physical, intellectual, emotional,social, and spiritual needs and to facilitate patient autonomy,access to information, and choice.”5The Center to Advance Palliative Care and the AmericanCancer Society developed a definition of palliative care (basedon public opinion research), “Palliative care is specializedmedical care for people with serious illness. It focuses onproviding relief from the symptoms and stress of a seriousillness. The goal is to improve quality of life for both the patientand the family.iiThe Institute of Medicine(IOM) offers the followingdefinitions (2015):Specialty palliative care:“Palliative care that isdelivered by health careprofessionals who arepalliative care specialists, suchas physicians who are boardcertified in this specialty;palliative-certified nurses; andpalliative care-certified socialworkers, pharmacists, andchaplains.”Primary palliative care (alsoknown as generalist palliativecare): “Palliative care thatis delivered by health careprofessionals who are notpalliative care specialists, suchas primary care clinicians;physicians who are diseaseoriented specialists (such asoncologists and cardiologists);and nurses, social workers,pharmacists, chaplains,and others who care forthis population but are notcertified in palliative care.”Clinical Practice Guidelines for Quality Palliative Care, 4th edition
ForewordPalliative care is provided by a team of palliative care doctors, nurses, social workers and others whowork together with a patient’s other doctors to provide an extra layer of support. It is appropriateat any age and at any stage in a serious illness and can be provided along with curative treatment.”6Specialist palliative care provides an added layer of support towards maximizing patient and family qualityof life during serious illness. Palliative care knowledge and skills, however, should be core competenciesfor all health professionals serving seriously ill patients and their families and caregivers.HospiceHospice is a specific type of palliative care provided to individuals with a life expectancy measured inmonths, not years. Hospice teams provide patients and families with expert medical care, emotional, andspiritual support, focusing on improving patient and family quality of life.To be eligible to receive hospice under the Medicare or Medicaid hospice benefit, adult patients musthave a defined, time-limited prognosis (certified by two physicians as six months or less if the diseasefollows its usual course) and desire care focused on comfort, foregoing insurance coverage for furtherterminal disease-directed curative treatment efforts. The Patient Protection and Affordable Care Act of2010 contained provisions allowing pediatric patients to receive disease-modifying treatment while alsoreceiving hospice services.Nearly 50% of Medicare decedents received hospice in 2016,7 most of which was provided in communitysettings, primarily the patient’s chosen residence, which includes home, nursing homes and otherresidential facilities, as well as skilled nursing facilities.8 Hospice is also available to Medicaid recipientsin most states and is covered as part of many commercial health plans.History of the National Consensus Project’s GuidelinesSeventeen years ago, leaders from across the country gathered to discuss the development of consensusguidelines for quality palliative care so that patients with serious illness who were not hospice-eligiblecould access palliative care. Representatives of hospice and palliative care organizations collaborated inthe development of the first edition of the National Consensus Project’s Clinical Practice Guidelines forQuality Palliative Care (NCP Guidelines), which described core concepts and structures and processesnecessary for quality palliative care, including eight domains of practice.The first edition of the NCP Guidelines, published in 2004, presented a blueprint for excellence inthe delivery of palliative care. For the first time outside of hospice, teams had a framework to guidethe development of quality palliative care services. Since that time, palliative care has continued togrow and evolve, necessitating updated NCP Guidelines in 2009 and 2013. The second edition of theNCP Guidelines, published in 2009, reflected the tremendous growth and transformation in the field ofhospice and palliative care, acknowledging the diverse array of models and approaches to care for thiscomplex population. The third edition of the NCP Guidelines, published in 2013, emphasized continuity,consistency, and quality of care.Clinical Practice Guidelines for Quality Palliative Care, 4th editioniii
ForewordThe NCP Guidelines, 4th edition, are organized into 8 domains:Domain 1: Structure and Processes of CareThe composition of an interdisciplinary team is outlined, including the professional qualifications,education, training, and support needed to deliver optimal patient- and family-centered care. Domain1 also defines the elements of the palliative care assessment and care plan, as well as systems andprocesses specific to palliative care.Domain 2: Physical Aspects of CareThe palliative care assessment, care planning, and treatment of physical symptoms are described,emphasizing patient- and family-directed holistic care.Domain 3: Psychological and Psychiatric AspectsThe domain focuses on the processes for systematically assessing and addressing the psychological andpsychiatric aspects of care in the context of serious illness.Domain 4: Social Aspects of CareDomain 4 outlines the palliative care approach to assessing and addressing patient and family socialsupport needs.Domain 5: Spiritual, Religious, and Existential Aspects of CareThe spiritual, religious, and existential aspects of care are described, including the importance of screeningfor unmet needs.Domain 6: Cultural Aspects of CareThe domain outlines the ways in which culture influences both palliative care delivery and the experienceof that care by the patient and family, from the time of diagnosis through death and bereavement.Domain 7: Care of the Patient Nearing the End of LifeThis domain focuses on the symptoms and situations that are common in the final days and weeks of life.Domain 8: Ethical and Legal Aspects of CareContent includes advance care planning, surrogate decision-making, regulatory and legal considerations,and related palliative care issues, focusing on ethical imperatives and processes to support patientautonomy.ivClinical Practice Guidelines for Quality Palliative Care, 4th edition
ForewordNCP Guidelines, 4th editionThe goal of the 4th edition of the National Consensus Project’s Clinical Practice Guidelines for QualityPalliative Care (NCP Guidelines) is to improve access to quality palliative care for all people with seriousillness regardless of setting, diagnosis, prognosis, or age. The NCP Guidelines are intended to encourageand guide health care organizations and clinicians (including no
Clinical Practice Guidelines for Quality Palliative Care, 4th edition i Foreword Individuals who are seriously ill need care that is seamless across settings, can rapidly respond to needs and changes in health status, and is aligned with patient-family preferences and goals . Patients of