Transcription
Blood Management and TransfusionPractice Handbook 2021ContentsAbbreviations and acronyms .3The Australian context.6Blood Management/Transfusion Nurse/Trainer/Safety Officer .6Blood Matters program .8History.8Current .8What provides structure and informs your practice? .9Australian Health Ministers’ Conference Statement on National Stewardship Expectations for the Supply ofBlood and Blood Products (Nov 2010) .9National Blood Authority Patient Blood Management Guidelines.9National Safety and Quality Health Service Standards – second edition . 10ANZSBT guidelines . 10Australian standard - AS 3864.2 - 2012 - Medical refrigeration equipment - For the storage of blood andblood products. 10Blood Management Committee (BMC)/Transfusion Governance Group (TGG)/Hospital TransfusionCommittee (HTC) or Patient Blood Management Committee (PBMC) . 11Resources . 12Guidelines and hospital circulars . 12International sites. 14Graduate Certificate in Transfusion Practice . 15Transfusion journals . 15Educational materials . 16Professional organisations: . 17ANZSBT and ANZTP . 17Membership of ANZTP Network . 17
ISBT and TP forum . 18Transfusion Practitioner (TP) Forum*. 18Lifeblood (The Blood Service) . 19Blood donation . 19Donors and blood donation. 19Testing . 19Test results. 20The decision to transfuse. 21Patient blood management (PBM) guidelines . 21Pre-transfusion testing . 21Blood types . 21Are they compatible?. 22Chart for red cell compatibility 3 ) . 22ABO component compatibility table (http://www.transfusion.com.au/blood basics/compatibility ) . 23Blood products . 24Fresh components . 24Fractionated plasma products. 24CSL Behring products . 25Synthetic blood clotting factors . 26Consent, refusal and medical treatment planning and decision act. 27Consumer information on consent for transfusion . 27Clinical audit. 29Tips for auditing. 29Haemovigilance. 30The Blood Matters’ Serious Transfusion Incidents Reporting (STIR) system . 30National Haemovigilance . 31Transfusion science and blood stewardship . 32Subcutaneous Immunoglobulin. 34Transfusion Handbook2
Abbreviations and acronymsThis list is a starting point for the abbreviations and acronyms used in blood transfusion, laboratory blood bank, theLifeblood and haematology, feel free to copy the list and add your own as you find them and those that areparticular to your health service.AABBABOACHSACSQHCAHMACAHPANHAnti DFNHIVHLAHPAHSANZHTCHTLVTransfusion Handbookan association founded in the United States in 1947 as the American Association of BloodBanks. In 2005, the association changed its name to AABB to reflect the changes in itsscope and operationsABO blood group systemAustralian Council on Healthcare StandardsAustralian Commission on Safety and Quality in HealthcareAustralian Health Ministers Advisory CouncilApproved Health ProviderAcute normolvolaemic haemodilutionRh D ImmunoglobulinAustralian and New Zealand Society of Blood TransfusionAustralian and New Zealand Transfusion ProfessionalsAustralian Society of Thombosis and HaemostasisAcute Transfusion ReactionBritish Committee for Standards in HaematologyOnline blood ordering and inventory systemOnline system for tracking, authorisation and review of immunoglobulin use (IVIg andSCIg)Blood Matters Advisory CommitteeBlood Management Committee: group of clinical and Lifeblood professionals that meet todiscuss transfusion issuesBlood Management Nurse/coordinatorBlood User Group: group of clinical and Lifeblood professionals that meet to discusstransfusion issuesCytomegalovirusDirect Antiglobulin TestDelayed Transfusion ReactionEmergency Blood Management PlanEthlenediaminotetraacetic acid: anticoagulant used in some blood tubesEnzyme-linked Immunosorbent Assay: commonly used analytical biochemistry assayused for detecting and quantifying soluble substances such as peptides, proteins,antibodies, and hormones.Food & Drug Administration (USA)Fresh Frozen PlasmaFebrile Non-Haemolytic Transfusion ReactionHaemoglobinHepatitis B virusHepatitis C virusHaemolytic disease of the foetus and newbornHuman Immunodeficiency virusHuman Leucocyte AntigenHuman Platelet AntigenHaematology Society of Australia and New ZealandHospital Transfusion CommitteeHuman T-cell Lymphotropic Virus: a group of human retroviruses that are associated withseveral serious conditions, including adult T-cell leukaemia/lymphoma3
OTQOTTTTIVAEDvCJDVHIMSTransfusion HandbookHaemolytic Transfusion ReactionIncorrect Blood Component TransfusedInternational Society of Blood TransfusionIntravenous ImmunoglobulinJurisdictional Blood CommitteeKey Performance IndicatorAustralian Red Cross LifebloodMaximum Blood Ordering ScheduleMemorandum of UnderstandingNeonatal Alloimmune ThrombocytopeniaNational Association of Testing Authorities, Australia: is the national accreditation body forlaboratories in Australia.Nucleic Acid TestingNational Blood AuthorityNational Blood Management System: the system used by Lifeblood to monitor both donorand inventory information.National Blood Service (UK)National Blood Supply Contingency PlanNational Blood Transfusion CommitteeNational Health and Medical Research CouncilNational Health Service (UK)Normal immunoglobulinNational Safety, Quality Health Service StandardsPatient Blood ManagementPost-Transfusion PurpuraRoyal College of Pathologists of AustralasiaRh blood group: a complex group of antigens, second in importance only to the ABO bloodgroup in the field of transfusion medicine.Society for the Advancement of Blood ManagementSubcutaneous immunoglobulinSerious Hazards of Transfusion (UK)Serious Transfusion Incident ReportTransfusion-Associated Circulatory OverloadTransfusion-Associated Graft Versus Host DiseaseTherapeutic Goods AdministrationTransfusion Governance GroupTransfusion Medicine ServiceTransfusion NurseTransfusion ProfessionalTransfusion Outcomes Research CollaborativeTransfusion-Related Acute Lung InjuryTransfusion Research UnitTransfusion Safety OfficerTransfusion Quality OfficerTransfusion TrainerTransfusion-Transmitted InfectionsVictorian Admitted Episodes Datasetvariant Creutzfeldt-Jakob DiseaseVictorian Health Incident Management System4
VIDGVTISWBITWHOTransfusion HandbookVictorian Immunohaematology Discussion GroupVictorian Transplantation and Immunogenetics ServiceWrong Blood in TubeWorld Health Organization5
IntroductionThe Australian contextThe National Blood Authority (NBA) is a statutory agency within the Commonwealth Government’s health portfoliothat manages and coordinates arrangements for the supply of blood and blood products and services on behalf ofthe Commonwealth and jurisdictional governments. The NBA reports to the Health Minister and the JurisdictionalBlood Committee (JBC).The National Blood Authority (NBA) Stewardship Program is aimed at supporting jurisdictions and health providersto implement the requirements of the Australian Health Ministers’ Statement on National Stewardship Expectationson the Supply of Blood and Blood Products (the Stewardship Statement), issued on 12 November 2010.The JBC is the conduit between governments and the NBA. Representation from all jurisdictions provides positionson: blood policy, demand, supply planning and product distribution funding and evidence-based approaches to emerging products services and technologiesIt oversees the NBA’s role in blood supply contracting.Australia has only one fresh product supplier, Australian Red Cross Lifeblood (Lifeblood), whereas fractionatedproducts are managed through contracts with the successful tenders and include Australian and internationalsuppliers e.g. intravenous immunoglobulin, haemophilia products. Lifeblood then distributes these products tohealth services.The budget for blood and blood products is cost shared between the Commonwealth government at 63 per centand jurisdictional governments at 37 per cent collectively.At a jurisdictional level, blood budgets are distributed in a variety of ways, centrally controlled by the local jurisdictional health department, devolved to health services/pathologies where the proportional dollar value is attributed according todesigned usage/population figure or partially devolved which is a mix of central and devolved funding. Where funding is devolved, it is to publichealth services, not private. In jurisdictions with a devolved blood budget it is only the state portion that isdevolved.Regardless of the funding model applied at the jurisdictional level, blood product costs are not passed onto theAustralian health consumer, as per the National Stewardship agreement.Blood Management/Transfusion Nurse/Trainer/Safety OfficerWithin each state and territory, there are a number of clinicians, primarily nurses, working in the area of quality andsafety for blood management and transfusion practice. These positions have a variety of names and are oftensupported by jurisdictional programs. In Victoria, these clinical specialists (professionals) are supported by theBlood Matters team, who also provide support to roles in Tasmania, Australian Capital Territory (ACT) andNorthern Territory (NT), through Memorandums of Understanding (MoU). In New South Wales, support is providedby Blood Watch (Clinical Excellence Commission) and South Australia it is BloodSafe. Western Australia andQueensland programs are no longer centrally coordinated; however, there are many roles within each of thesestates.Blood Matters has a Transfusion Nurse and Patient Blood Management Education Coordinator (both 0.6 FTE) toprovide support for these professional roles and help direct activities within Victoria. Each state, dependant on thespecific structure of these programs, offers a similar service.Transfusion Handbook6
Lifeblood also has Transfusion Nurse roles covering all states and territories, with their focus being on facilitatingspecialist blood product support.Reference: Bielby, L., Akers, C., Francis, S., Darby, S., Campbell, L., Hollis, L., Quested, B. and Hogan, C. (2016), The role of the transfusionsafety coordinator in Australia. VOXS, 11: 118 –125. doi:10.1111/voxs.12201Transfusion Handbook7
Blood Matters programHistoryThe Blood Matters project commenced in April 2002, with the formation of a consortium composed of the thenVictorian Department of Human Services, Peter MacCallum Cancer Institute, The Royal Melbourne Hospital andwhat was then the Blood Service, now Lifeblood. This consortium developed and tested tools and processes toimprove transfusion practice in hospitals.The Blood Matters project was expanded in 2003 to include an additional 12 public hospitals in a Blood MattersBreakthrough Collaborative project; using a project methodology developed by the Institute for HealthcareImprovement in the United States. These hospitals further tested and developed transfusion interventions over an18-month period.The interventions included: improving clinician and patient awareness and knowledge of blood product use improving clinical decision making enhancing the blood administration process by making all successful practical improvement strategies availableto other hospitals in Victoria and TasmaniaAs part of the Blood Matters project, the transfusion nurse (TN) role was es tablished in metropolitan and majorregional hospitals. To support those in the role, the Blood Matters Consortium project developed a postgraduateCertificate in Transfusion Practice. The Better Safer Transfusion (BeST) program was established in 2004continuing the work of the Blood Matters project and in 2008 changed its name to the Blood Matters Program. In2009, further funding was sought to provide workforce in the area of transfusion improvement to regional and ruralhealth services, with a focus on cancer services. A transfusion trainer (TT) role was established. Currently 43health services in Victoria employ a specialist clinician to undertake blood management and transfusionimprovement.CurrentThe Blood Matters program is a joint initiative of the Planning, Funding and Monitoring Branch, Health andWellbeing Division, Department of Health and Human Services, Victoria, and Australian Red Cross Lifeblood. Thegoal of the program is to support and enhance best practice in all aspects of blood management encompassingpatient blood management (PBM), the stewardship of blood and blood products and transfusion practice, forimproved patient outcomes in Victorian health services. Tasmania, the ACT, and the NT collaborate with BloodMatters regularly through MoU.The Blood Matters program is supported by a secretariat including a program manager, data and informationmanagers, a transfusion nurse, a PBM education coordinator and two project roles. One project targets transfusionscience aspects of blood management and transfusion practice (evolving from the red cell wastage project) and theother assisting health services implement subcutaneous immunoglobulin (SCIg) programs. Blood Matters issupported by a multidisciplinary advisory committee (BMAC).Transfusion Handbook8
What provides structure and informs your practice?The following statements, guidelines, and standards are pivotal to providing the structure and evidence for practice.Australian Health Ministers’ Conference Statement on National StewardshipExpectations for the Supply of Blood and Blood Products (Nov 2010)The Australian Health Ministers’ Conference has determined that a clear statement is needed on governments’stewardship expectations for the providers of blood and blood products within the health sector. Stewardship, inthis context, means responsible, sustainable and appropriate use of blood and blood ional Blood Authority Patient Blood Management GuidelinesThe National Blood Authority (NBA) has funded and managed the development of a series of evidence-basedPatient Blood Management (PBM) Guidelines, comprising six modules.All the modules are intended to assist and guide health-care professionals in making clinical decisions whenmanaging patients in the following clinical situations: Module 1 Critical Bleeding/Massive Transfusion Module 2 Perioperative – including pre, intra and postoperative of patients undergoing surgery or invasiveprocedures, particularly those in which blood loss is anticipated. Module 3 Medical – including patients with acute or chronic medical conditions requiring haematologicalintervention. Module 4 Critical Care Module 5 Obstetrics and Maternity for managing pregnant and postpartum women. Module 6 Neonatal and Paediatrics for blood management in neonatal and paediatric patients.These guidelines are currently under review.Transfusion Handbook9
National Safety and Quality Health Service Standards – second editionIn 2011, the first edition of the Australian Commission on Safety and Quality in Healthcare National Safety andQuality Health Service (NSQHS) Standards were released to drive the implementation of safety and qualitysystems and improve the quality of health care in Australia. The NSQHS Standards provide a nationally consistentstatement about the level of care consumers can expect from health services. Health services have been assessedto these standards since January 2013.The second edition was released November 2017 and health services will be assessed to these new standardsfrom January 2019. The second edition addresses gaps identified in the first edition and actions have beenconsolidated and streamlined to make them clearer and easier to implement and reduce duplication.The Blood and Blood Product standard has been renamed the Blood Management standard. The revised standardhas added important aspects of patient blood management, acknowledging patients’ blood is a valuable andunique resource that should be conserved and managed well. This standard aims to ensure that safe, appropriate,effective, and efficient blood systems are in place to minimise risk associated with the use of blood products.The Transfusion Governance Group (TGG), often known as the Blood Management Committee (BMC), HospitalTransfusion Committee (HTC) or Patient Blood Management Committee (PBMC) play a very important role in thehealth service to ensure that all actions for the standards are addressed and met. This group develops andoversees systems to identify and coordinate actions to improve the quality of practice across the range of activitiesrelating to blood and blood products.Rural or small metropolitan health services may not have access to the expertise available in larger, metropolitansites; therefore, the model should be varied so that the outputs still occur. In lieu of a specific committee or group,hospital transfusion governance oversight may occur by adding transfusion as an agenda item on an existingclinical governance committee such as a clinical review, risk management or infection control committee. A teamshould be formed; however, it may only consist of two people with regular contact that ensures the direction andobjectives set by the transfusion governance group or equivalent, are implemented. Important individuals may beeducators and/or those in quality/risk roles.Information on the National Safety Quality Health Service Standards and the accreditation process is available condedition/ANZSBT guidelinesThe Australian & New Zealand Society of Blood Transfusion (ANZSBT) have developed a suite of guidelines,which can be access via the following link: htmlGuidelines that will be of particular benefit to you are: Administration of blood products, 3rd edition, 2018 Transfusion and immunohaematology laboratory practice, 1st edition, revised January 2020 Prevention of transfusion-associated graft-versus-host disease (TAGVHD), January 2011Australian standard - AS 3864.2 - 2012 - Medical refrigeration equipment For the storage of blood and blood productsThe objective of this Standard is to safeguard recipients of blood transfusions by ensuring that blood and bloodproducts are properly and safely stored at the required temperature in refrigeration equipment or walk -in roomsspecifically manufactured for the purpose.The Standard consists of two parts: Part 1: Manufacturing requirements Part 2: User-related requirements for care, maintenance, performance verification and calibration.Transfusion Handbook10
Blood Management Committee (BMC)/Transfusion Governance Group(TGG)/Hospital Transfusion Committee (HTC) or Patient Blood ManagementCommittee (PBMC)The role of the Committee is to ensure that blood and blood products are used appropriately, safely, effectively andefficiently in accordance with national standards and guidelines. It is also a key driver of change as PBM principlesand strategies are adopted. (PBM Committee handbook, Lifeblood, 2014)This requires commitment of the health service management and clinical/laboratory staff to a PBM/ transfusioninfrastructure including a Committee.Not all health services will need to have a stand alone Committee, however all health services should havestructures and processes in place that fulfil the role and function of a Committe. A key responsibility of theCommittee is risk management. The primary role of a Committee is to provide an active forum for communicationbetween staff directly involved in clinical and laboratory-based PBM/blood transfusion activities, to providesolutions, feedback and education in relation to identified problems, and to ensure that transfusion practice accordswith best practice.Vicotrian health services should refer to the Hospital Circular 01/2018 Health Service Blood ManagementCommittees which cn be accessed via the Blood Matters webpage. apeutics/bloodmatters/ /link.aspx? id 48A7A451B920402D8A025BD2140B13DF& z zTransfusion teamThe ‘team’ expedites work determined by the committee and responds to transfusion issues that arise betweencommittee meetings, and therefore needs to have membership with relevant expertise.The team may include a BMN/TN/TT/TSO, transfusion scientist, transfusion registrar, medical champion andquality/risk representative.The medical champion may vary depending on the work areas of the transfusion team and committee, for example:a cardiac anaesthetist for cardiac-related work, an intensivist or a haematologist. Ideally, the medical champion hasa full-time or permanent appointment in the organisation for continuity.The quality/risk management representative is a valued member because they understand national standards,systems in their organisation and how to achieve hospital-wide change in practice. This knowledge is important fortransfusion improvement activities and to ensure the BMC/TGG/HTC/PBMC is embedded and visible within thequality systems of the organisation.The team should meet at regular intervals, however work should proceed between meetings and this may be moreas a ‘virtual’ team; collaborating and communicating as a single entity on the directions set by the committee, or onissues arising between committee meetings. The BMN/TN/TT/TSO may have a major coordination role for thisteam, if it is not taken up by a senior manager in the organisation.Transfusion Handbook11
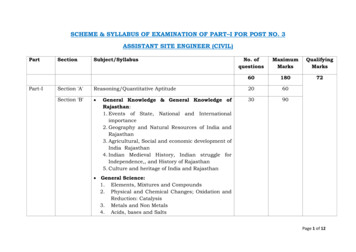
ResourcesGuidelines and hospital circularsThe following list includes current Australian guidelines, standards and Victorian Department Health and HumanServices hospital circulars available to inform your practice. Full versions of the guidelines, standards and circularscan be found at the website links.TitleWebsiteYear ofpublicationNational Blood Authority patient bloodmanagement guidelines (Modules 6Australian and New Zealand Society of Bloodtransfusion (ANZSBT)/ Australian College ofNursing (ACN)—Guidelines for theAdministration of blood products 3 rd edition es.htmlANZSBT— Guidelines for transfusion andimmunohaematology laboratory practice, 1 stedition, elines.html2020ANZSBT—Prevention of TransfusionAssociated Graft-versus -host disease delines.html2011Guidelines for the management of haemophiliain 2016Immunoglobulin Product Authorisation 019An update of consensus guidelines forWarfarin reversal, on behalf of theAustralasian Society of Thrombosis l2013Department of Health & Human Services —Hospital circular on traceability of blood andblood products odmatters/ /link.aspx? id 48A7A451B920402D8A025BD2140B13DF&z apeutics/bloodmatters/ /link.aspx? id 845A74FC5A6D4FA983917D5BA0DCC565&z z2018Department of Health & Human Services —Hospital Circular 01/2018: Health ServiceBlood Management Committees (Replaces07/2002 – Hospital transfusion committees)Department of Health & Human Services —Department of Human Services Victoria:Victorian health service’s Emergency BloodManagement Plan (EBMP)Transfusion Handbook2018202012
Department of Health & Human Services —Hospital Circular 10/2013: SubcutaneousImmunoglobulin (SCIg)National Safety Quality Health ServiceStandards Second edition – BloodManagement icstherapeutics/bloodmatters/ /link.aspx? id D69874CA8E60453C93451443077AE8B7& z -edition/Australian Standard -AS 3864v2-2012 tion equipment – for the storage ofau/Standards/AS-3864-2-2012blood and blood products-user –related1600491/requirements for c
Transfusion Handbook 2 ISBT and TP forum . Australian Red Cross Lifeblood (Lifeblood), whereas fractionated products are managed through contracts with the successful tenders and include Australian and international suppliers e.g. intravenous immunoglobulin, haemophil