Transcription
NEUROSURGICALFOCUSNeurosurg Focus 50 (5):E17, 2021Systematic review of charged-particle therapy forchordomas and sarcomas of the mobile spine and sacrumZach Pennington, BS,1 Jeff Ehresman, BS,1 Aladine A. Elsamadicy, MD,2 John H. Shin, MD,3C. Rory Goodwin, MD, PhD,4 Joseph H. Schwab, MD,5 and Daniel M. Sciubba, MD1Department of Neurosurgery, Johns Hopkins University School of Medicine, Baltimore, Maryland; 2Department of Neurosurgery,Yale University School of Medicine, New Haven, Connecticut; 3Department of Neurosurgery, Massachusetts General Hospital,Harvard Medical School, Boston, Massachusetts; 4Department of Neurosurgery, Duke University Medical Center, Durham,North Carolina; and 5Department of Orthopaedic Surgery, Massachusetts General Hospital, Harvard Medical School, Boston,Massachusetts1OBJECTIVE Long-term local control in patients with primary chordoma and sarcoma of the spine and sacrum is increasingly reliant upon en bloc resection with negative margins. At many institutions, adjuvant radiation is recommended;definitive radiation is also recommended for the treatment of unresectable tumors. Because of the high off-target radiation toxicities associated with conventional radiotherapy, there has been growing interest in the use of proton and heavyion therapies. The aim of this study was to systematically review the literature regarding these therapies.METHODS The PubMed, OVID, Embase, and Web of Science databases were queried for articles describing the useof proton, combined proton/photon, or heavy-ion therapies for adjuvant or definitive radiotherapy in patients with primarysarcoma or chordoma of the mobile spine and sacrum. A qualitative synthesis of the results was performed, focusing onoverall survival (OS), progression-free survival (PFS), disease-free survival (DFS), and disease-specific survival (DSS);local control; and postradiation toxicities.RESULTS Of 595 unique articles, 64 underwent full-text screening and 38 were included in the final synthesis. Allstudies were level III or IV evidence with a high risk of bias; there was also significant overlap in the reported populations, with six centers accounting for roughly three-fourths of all reports. Five-year therapy outcomes were as follows:proton-only therapies, OS 67%–82%, PFS 31%–57%, and DFS 52%–62%; metastases occurred in 17%–18% and acutetoxicities in 3%–100% of cases; combined proton/photon therapy, local control 62%–85%, OS 78%–87%, PFS 90%, andDFS 61%–72%; metastases occurred in 12%–14% and acute toxicities in 84%–100% of cases; and carbon ion therapy,local control 53%–100%, OS 52%–86%, PFS (only reported for 3 years) 48%–76%, and DFS 50%–53%; metastasesoccurred in 2%–39% and acute toxicities in 26%–48%. There were no studies directly comparing outcomes betweenphoton and charged-particle therapies or comparing outcomes between radiation and surgical groups.CONCLUSIONS The current evidence for charged-particle therapies in the management of sarcomas of the spine andsacrum is limited. Preliminary evidence suggests that with these therapies local control and OS at 5 years are comparable among various charged-particle options and may be similar between those treated with definitive charged-particletherapy and historical surgical cohorts. Further research directly comparing charged-particle and photon-based therapies is 2.FOCUS201059EKEYWORDS chordoma; carbon ion therapy; proton therapy; radiotherapy; local control; adjuvantn bloc resection with negative margins (R0 resection) improves local control (LC) and disease-freesurvival (DFS) in patients with chordoma and primary sarcomas of the spinal column and sacrum.1–5 R0resection may also improve overall survival (OS).1,6 Sur-gery has been the mainstay of therapy for years as thesetumors are radioresistant and the doses required to improve LC were unacceptably toxic to local healthy tissues.Certain locations, such as the mobile spine, offer uniquechallenges given the often close approximation of tumorABBREVIATIONS CIRT carbon ion radiotherapy; CTC Common Toxicity Criteria; DFS disease-free survival; DSS disease-specific survival; LC local control;LFU last follow-up; MGH Massachusetts General Hospital; OS overall survival; PFS progression-free survival; PRISMA Preferred Reporting Items for SystematicReviews and Meta-Analyses; RBE relative biological effectiveness; RFS relapse-free survival.SUBMITTED December 14, 2020. ACCEPTED February 23, 2021.INCLUDE WHEN CITING DOI: 10.3171/2021.2.FOCUS201059. AANS 2021, except where prohibited by US copyright lawNeurosurg Focus Volume 50 May 20211Unauthenticated Downloaded 04/21/22 06:53 PM UTC
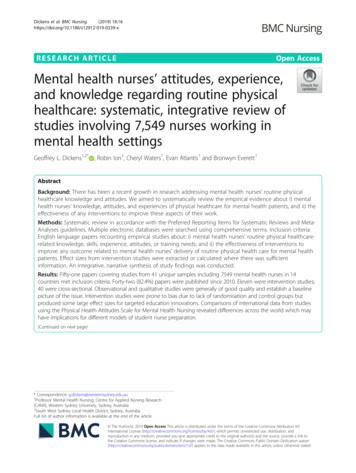
Pennington et al.and eloquent nervous tissue. In the latter part of the 20thcentury, though, more advanced radiation modalities became clinically available as adjuvant or definitive therapy, including focused photon radiotherapy modalities andcharged-particle therapies, notably proton therapy andcarbon ion radiotherapy (CIRT). Charged particles havesuperior behaviors in soft tissue that theoretically enablethem to provide more focused delivery of radiation energyto the target site with minimal off-target effects.Preliminary studies, such as those from the Massachusetts General Hospital (MGH),7,8 found that the additionof modern radiation therapy could improve LC in patientsoperated on for spinal chordoma. Importantly, LC ratesimproved even in patients with positive surgical margins.More recent evidence has suggested that adjuvant radiation with these advanced modalities may be even moreimportant to LC than surgical margins,9 perhaps due tothe presence of micrometastatic disease located immediately outside the tumor pseudocapsule. As such, thereis increased interest among spine surgeons, medical oncologists, and radiation oncologists in the use of protontherapy and hadron therapy as either definitive or adjuvantradiotherapy for patients with chordoma and sarcoma ofthe spinal column. In this study, we sought to systematically review the existing literature with a focus on radiation regimens, LC, DFS, progression-free survival (PFS),OS, and postradiotherapy complications. Our main objective was to compare the efficacy of proton, mixed proton/photon, and carbon ion radiotherapy in terms of the aboveoutcomes, focusing on LC, PFS, DFS, and OS at 5 yearsfollowing radiation treatment. We included both surgeryand radiation-only series to address the second question ofwhether definitive radiotherapy with charged particles canproduce 5-year LC, OS, DFS, and PFS rates similar to therates reported in historical surgical series.MethodsA literature search was conducted on November 13,2020, to identify all published reports of proton therapy,combined proton therapy/photon tomotherapy, and hadrontherapy for patients with primary chordoma or sarcoma ofthe mobile spine and sacrum. Queried databases includedPubMed/Medline, Embase, OVID Medline, and Web ofScience. We also queried the bibliographies of includedarticles to identify additional articles. The search queryfor the PubMed/Medline database was (“chordoma” OR“chondrosarcoma” OR “osteosarcoma” OR “osteogenicsarcoma” OR “Ewing sarcoma” OR “Ewing’s sarcoma”OR “Ewings sarcoma” OR “primary bone tumor” OR“primary vertebral tumor” OR “primary spine tumor”)AND (spine OR spinal OR vertebral OR vertebra ORvertebrae OR sacrum OR sacral) AND (“carbon ion” OR“hadron” OR “proton” OR “proton therapy” OR “carbonion therapy” OR “hadron therapy” OR “charged ion” OR“charged ion therapy”). The individual queries for eachdatabase are listed in the Appendix.Included studies had full-text English translations andincluded a minimum of 5 adult patients ( 16 years ofage) being treated for a primary sarcoma or chordoma ofthe mobile spine or sacrum. Articles had to provide pri2mary data on one of the following outcomes of interest:OS, PFS, disease-specific survival (DSS), DFS, LC, ratesof metastasis, and radiation-associated toxicities. Articleswere excluded if they pooled adult and pediatric patients,pooled spine/sacral lesions with lesions of other sites,pooled patients treated with pure photon regimens withthose receiving proton/charged-particle regimens, or presented nonprimary data (i.e., fit one of the following article types: commentary, opinion, perspective, systematicreview, narrative review). Articles were screened by tworeviewers (Z.P. and J.E.), with a third reviewer (D.M.S.)serving as referee in case of disagreement. Screening wasperformed using Covidence v2313 (Covidence) accordingto the Preferred Reporting Items for Systematic Reviewsand Meta-Analyses (PRISMA) statement.10We collected details about patient demographics (age,sex, median tumor clinical target volume), radiation treatment modality (protons, mixed protons and photons,CIRT, or other hadron therapy), dosing schema (total dose,fractionation, duration), and concomitant treatments givenwith radiation (including surgery, chemotherapy, and hyperthermia). All studies were case series and were deemedto have a high risk of bias.ResultsIn total, 595 unique articles were identified, of which 64underwent full-text screening and 36 were included in thefinal qualitative synthesis (Fig. 1).1,11–45 The most commonexclusion reasons were pooling of spine/sacrum lesionswith other lesion locations (n 14), the use of photon-onlyradiotherapy (n 9), and failure to report one of the outcomes of interest (n 3). Of the included articles, 8 examined proton-only therapy (Table 1),11,22, 33, 40–44 11 examinedcombined proton/photon radiotherapy (Table 2),1,12–20,4514 examined CIRT (Table 3),21,23–32, 34–36 and 3 examineda combination of proton radiotherapy and CIRT or another hadron therapy (Table 4).37–39 All included studieswere at high risk of reporting bias. All were level IV evidence based on the North American Spine Society Levelsof Evidence,46 except the study by Mima et al.37 (level IIIevidence). Most studies were published by five centers:the Heidelberg Ion Beam Therapy Center (n 3),21,31,34 theHyogo Ion Beam Medical Center in Japan (n 4),11,23, 37,39the MGH (n 9),1,13–17, 19, 20,22 the National Institute of Radiological Sciences in Chiba, Japan (n 10),23–29, 32, 33,36 andthe Paul Scherrer Institute (n 4).41–44 Unless otherwisestated, the results are reflective of adjuvant particle radiation before, after, or combined with surgery.Proton-Only SeriesAll 8 studies11,22, 33, 40–44 were small (5–116 patients). Themedian age was 50–71 years, the median follow-up was18–65 months, and patients were 55%–100% male. Excluding the study by Murray et al.,41 which separated chordoma and chondrosarcoma outcomes, the most commonpathologies were chordoma (67%–100% of patients) andchondrosarcoma (0%–33%). Five series11,22,42–44 describedoutcomes for only chordoma patients, and 0%–75% oflesions involved the mobile spine; 2 reported only outcomes for sacral chordoma.11,44 LC was 56%–68% at 5Neurosurg Focus Volume 50 May 2021Unauthenticated Downloaded 04/21/22 06:53 PM UTC
Pennington et al.FIG. 1. PRISMA flow diagram for study queries.years and 62%–100% at the last follow-up (LFU). Fiveyear outcomes were OS 67%–82%, PFS 31%–57%, andDFS 52%–62%. Metastases occurred in 17%–18% by theLFU. Acute toxicities were seen in 3%–100% of patientswith National Cancer Institute Common Toxicity Criteria(CTC) events grade 3 noted in 0%–20%. Late toxicitiesoccurred in 34%–60%, with 0%–16% suffering toxicities grade 3. The median dose relative biological effectiveness (RBE) ranged from 70 to 74; most used fractions of1.8–2.2 RBE. No common outcomes were reported bythe 2 studies of nonsurgical patients.11,44 However, Aibe etal.11 reported the following 3-year outcomes: LC 82%, OS93%, PFS 90%, and DFS 81.9%.Mixed Proton/Photon SeriesEleven studies described combined proton/photon therapy.1,12–20,45 All series were small (11–126 patients) with amedian age of 39–70 years, sex makeup of 45%–63% male,and median follow-up of 12.9–99.6 months; 54%–100% ofpatients were treated for chordoma with 6 series1,12–14,19,20including only chordoma patients. The median dose was68.4–77.4 RBE, most commonly given in 1.8–2 RBEfractions. LC rates were 36%–98% (1 year), 18%–90% (2years), 84%–97% (3 years), 62%–85% (5 years), and 49%–58% (10 years). The OS rates were 93%–96% (2 years),87%–92% (3 years), 78%–87% (5 years), and 53%–63%(10 years). PFS was only reported by Chen et al.,13 whoreported 90% at 5 years and 80% at 10 years. DFS was68%–77% at 3 years and 61%–72% at 5 years. Metastasesoccurred in 12%–14% (3 years), 20%–27% (5 years), and8%–24% (LFU). Acute toxicities occurred in 84%–100%(2%–16% suffered toxicities CTC grade 3), and late tox-icities occurred in 10%–100% (0%–28% suffered toxicities CTC grade 3). Chen et al.13 and Kabolizadeh et al.19described nonsurgical patients. Both cohorts were fromthe MGH and used a median dose of 77.4 RBE deliveredin 1.8–2 RBE fractions. At 3 years, the OS was 89%–92%and DSS was 96%–97%. Metastasis was seen in 12%–14%and the OS at 5 years was 78%–82%.CIRT SeriesFourteen studies described CIRT.21,23–32, 34–36 Studieswere small (7–219 patients), with only 2 studies from theNational Institute of Radiological Sciences in Chiba, Japan, including more than 100 patients.23,27 The median agewas 54–67 years, patients were 48%–80% male, and themedian follow-up was 18–80 months. Except in the studyby Matsumoto et al.,47 in all treated patients (94%–100%)chordoma was the most common disease, with 12 studies including only chordoma patients.21,23–27, 29, 30, 32, 34–36 Themedian dose was 64–86 RBE given in 2.2–4.6 RBE fractions. LC rates were 90%–94% (1 year), 76%–85% (2years), 53%–95% (3 years), and 53%–100% (5 years). TheOS rates were 97%–100% (2 years), 59%–86% (3 years),and 52%–86% (5 years). The PFS rates were 90%–95% (1year), 70%–80% (2 years), 48%–76% (3 years), and 48%–94% (10 years). The DFS was 50%–53% at 5 years, andImai et al.27 reported a 10-year DFS of 31.3%. Metastases occurred in 7%–9% (1 year), 32%–52% (5 years), and2%–39% (LFU). Acute toxicities occurred in 26%–48%(0%–18% suffered CTC grade 3 events), and late toxicities occurred in 59%–89% (0%–21% suffered CTC grade 3 events). Eight studies examined strictly nonsurgicalpatients,23,26–30,32,35 and in 6 of these studies patients wereNeurosurg Focus Volume 50 May 20213Unauthenticated Downloaded 04/21/22 06:53 PM UTC
463% M; 58yrs; 43mos; NG100 spinal chrd; 57% M; 56LOC: 46 C, 4yrs; 65T, 12 L, 38 Smos; NGSnideret al.,201842§(IV)Staabet al.,201143§(IV)64% M; 50yrs; 64.7mos; 386cm339 cndr; LOC:11 C, 21 T,0 L, 1 S; 6pelvisMurrayet al.,202041§(IV)Demizu 28 spine chrdsarcoma;et al.,LOC: 8 C, 5201733*‡(IV)L, 2 L/S, 13 S66% M; 58Indelica- 34 chrd; 17cndr; LOC:yrs; 3.7to et al.,20 C, 10 T/L,yrs; NG201640(IV)21 SMurray 116 chrd; LOC: 60% M; 5750 C, 8 T, 13yrs; 64.7et al.,L, 45 Smos; 809202041§(IV)cm340 chrd; LOC:16 C, 3 T,1 T/L, 10 L,11 SNAOpOutcomeTD med 70.2 RBE (chrd NG; instrumenta70.2, cndr 72 RBE);tion in 47%frx NG; time NG; 28prRT; 23 prRT phRTTD med 74 RBE; frx NG; 57% R0/R1; 43%time NG; 90% prRTR2/biopsyonly; 10% prRT only; instruphRTmentation in43%TD med 70 RBE; frx64% R0/R1;NG; time NG; 85%36% R2/prRT only; 15% prRTbiopsy only; phRTinstrumentation in 41%TD med 74 RBE; frx40% R0/R1 rsxn;1.8–2 RBE; time NG;60% R2 rsxn;88% prRT; 12% phRT39% w/ instruprRT combomentationTD med 74 RBE; frx53% R0/R1; 47%1.8–2.0 RBE; 4 days/R2; 53% priorwk 8–10 wks; 78%instrumentaprRT; 22% prRT tionphRTTD med 73.8 RBE, preop 45% op, 55%50.4 RBE, frx 1.8; 5no opdays/wk 6 wks; concurrent nilotinib 200mg 2/day 56 daysNG; NG; NG; TD med 70.0 Gy; frx NG; 61% op, 39%NGtime NGno op22 high-riskchrd; LOC: 1T, 8 L, 13 SCoteet al.,201822†(IV)59% M; 65yrs; 44.8mos; NGTD 70.4 RBE, frx 2.233 chrd, 11 w/55% M; 71pre-RT surgiyrs; 37RBE, 5 days/wk cal spacermos; 284.46 wksplacement;cm3100% SRTRegimenAibeet al.201811*(IV)Pt Demogr:AuthorsSex; Med& YearAge; Med FU;(LOE) NeuropathologyMed CTVLC& Mets3-yr PFS89.6%& DFS81.9%2-yr 95%,2-yr medLFUPFS 58.277%,mos,med 61.5 90% ofmospts5-yr 70.7% 5-yr PFS30.7%3-yr 92.7%OSPFS, DFS,DSS, &/orRFSLC: 5-yr 63%81% 5 yrs; PFS 5-yrmed 103 mos;med 15757%, med63% LFU;mos82 mosmets: NGLC: 62% 5 yrs;80% 5 yrs DFS 5-yrmets: NG57%LC: 55.9% 5 yrs; 67.3% 5 yrs DFS 5-yrmets: 17.9%51.7%LFU; LR:38.5% LFULC: 4-yr 58%,4-yr 72%PFS med 1.7mets: 14%;yrs; DFS:LR: 35% med57%; DSS1.7 yrs4-yr 72%LC: 67.9% 5 yrs; 81.6% 5 yrs DFS 5-yrmets: 17.2%62.1%LFU; LR:32.8% LFU5-yr 55.6%;mets: NGLC: NG; mets:NG3-yr LC: 81.8%;mets 11.8%;med time tomets 28 mosTABLE 1. Series describing outcomes for patients treated with proton-only regimensNGNGOverall: 8% grd 3;skin: 6% grd 3;mucositis: 2%grd 3Overall: 2.5%; 0%grd 3; post-RTneurop 2.5%NGNGNGNot separatedfrom skull baseoutcomesNGNGToxicityLateCONTINUED ON PAGE 5 »Overall: 5% grd 3; 1secondary malignancy, 1 vertebralfrac requiring opOverall: 5% grd 3;sacral frx: 3% grd3; GI: 2% grd 3Chrd cndr pooled;overall: 33.5%;7.7% grd 3Chrd cndr pooled;overall: 33.5%;7.7% grd 3Overall: 16% grd 3; 2secondary cancerNot separated fromskull base outcomesOverall: 64%, 3% Overall: 58%, 6%grd 3; skin: 32%grd 3; pain: 43%grd 2, 2% grd 3;grd 2; sacral frac:GI: 2% grd 3; GU:9% grd 2, 5% grd5% grd 2; pain:3; GI: 5% grd 2, 2%47% grd 2; other:grd 3; GU: 5% grd9% grd 22; neurop: 5% grd 2RT toxicity notRT toxicity not sepaseparated fromrated from nilotinibnilotinib toxicitytoxicityAcuteNGNGNGNGVolRespPennington et al.Neurosurg Focus Volume 50 May 2021Unauthenticated Downloaded 04/21/22 06:53 PM UTC
C cervical spine; chrd chordoma; cndr chondrosarcoma; CTV clinical target volume; demogr demographic; frac fracture; frx fraction; FU follow-up; GI gastrointestinal toxicity; grd grade; GU genitourinarytoxicity; L lumbar spine; LOC location; LOE level of evidence; LR local recurrence; med median; mets metastasis; NA not applicable; neurop post-RT neuropathy; NG not given; phRT photon radiotherapy;prRT proton radiotherapy; pt patient; R0 complete tumor removal on macroscopic and microscopic histology; R1 complete tumor removal on macroscopic but not microscopic examination; R2 tumor identified onboth macroscopic and microscopic examination; resp response; rsxn resection; RT radiotherapy; S sacrum; T thoracic spine; TD total dose; unresec unresectable; Vol volumetric; decrease; increase.* Hyogo Ion Beam Medical Center.† Massachusetts General Hospital.‡ Paul Scherrer Institute group.§ National Institute of Radiological Sciences, Chiba, Japan.Initial in 4/5; Overall: 100%; 20% Overall: 60%; 0% grd9–72% grd 3; pain: 3, 20% grd 3, iliac(med 48%)100% grd 2–3;frac; skin: 20% grdLFUskin: 60% grd 2;2; GI: 20% grd 1GI: 20% grd 3PFS med 18 mos;DSS 18mosLC: 100%; mets: Med 180%mosNATD 70 RBE; frx 2.5 RBE;41 days w/ 39 –42 ChyperthermiaTran5 unresec chrd; 100% M; 67et al.,LOC: 100% Syrs; 18202044§mos; NG(IV)OpOutcomeRTRegimenPt Demogr:AuthorsSex; Med& YearAge; Med FU;(LOE) NeuropathologyMed CTVTABLE 1. Series describing outcomes for patients treated with proton-only regimens» CONTINUED FROM PAGE 4LC& MetsOSPFS, DFS,DSS, &/orRFSVolRespAcuteToxicityLatePennington et al.treated at the National Institute of Radiological Sciences,23,26–29,32 so much of the data from these sources werefrom a similar and likely overlapping set of nonsurgicalpatients treated at the National Institute of RadiologicalSciences. Five-year outcomes were LC 72%–100%, OS52%–86%, and DFS 50%–53%. Metastasis occurred in14%–36% by the LFU.23,26–30, 32,35Other SeriesIn the 3 remaining series, 2 reported pooled outcomesfor patients treated with proton therapy and CIRT,37,39 and1 series described patients treated with helium, neon, orcombination helium/neon-based therapies.38 All 3 seriesstudied sacral chordoma; the median patient age was 61–72 years, and 48%–86% of patients were male. The median dose was 70.4–79.2 RBE given in fractions of 2–4.4RBE over a period of 4 weeks to 61 days. Only 5-year OS(85%–100%) and rates of metastases at the LFU (14%–29%) were reported by more than 1 study.38,39 Both studies from the Hyogo Ion Beam Medical Center employeda surgical spacer implanted posterior to the rectum to reduce dosing to the anus and rectum, whereas the study ofSchoenthaler et al.38 treated a mixture of surgical and nonsurgical patients. Only Tsugawa et al.39 reported outcomesfor nonsurgical patients.DiscussionRecent evidence has begun to suggest that adjuvant radiation9 may be the most significant predictor of LC in primary sarcomas of the spine and sacrum. The reasons forthis are at present unknown; however, preliminary histology-based studies suggest it may be due to micrometastaticdisease outside of the tumor capsule.48 Additionally, somelesions are not amenable to surgery, meaning that definitiveradiotherapy may be the only option. Given the radioresistance of primary bone sarcomas to conventional radiation,there is great interest in the utility of charged-particle therapies for the definitive or adjuvant management of theselesions. Previous reviews focusing on chordoma and chondrosarcoma of the skull base have found these modalitiesto produce high rates of OS and LC of up to 5 years. Here,we provide a similar analysis of the efficacy of these treatment methods in the mobile spine and sacrum. Relative tothe reported rates for skull base lesions, we find that OSand LC rates are lower. However, given the findings frompopulation-level studies,49 it is possible that these differences may be due to the overall better prognosis of skullbase lesions relative to those of the spine/sacrum.Of particular interest are the reported efficacies of thevarious radiation modalities as definitive therapies. Theavailable data are severely limited. Of those studies including only nonsurgical patients, LC is similar for patientstreated with protons (82% at 3 years)11 and CIRT (72%–100% at 5 years). OS is likewise similar for combined photon/proton radiotherapy and CIRT at 5 years (78%–82%vs 52%–86%). Of note, statistical comparisons were notpossible given the significant overlap in the reported studypopulations. Despite this, Mima et al.37 directly comparedoutcomes between proton and hadron therapy for sacralchordoma and saw no significant differences in LC, PFS,Neurosurg Focus Volume 50 May 20215Unauthenticated Downloaded 04/21/22 06:53 PM UTC
6Pt Demogr:Sex; MedAge; Med FU;NeuropathologyMed CTV24 unresecchrd; LOC: 2C, 1 T, 2 L,19 S54% M; 70yrs; 56mos; 198cm3NG; 64 yrs;46 mos;255 cm320 chrd; LOC: 1 45% M; NG;CheneyC, 3 L, 16 S1.8 yrs;et al.,NG201414*(IV)NG; 54 yrs;Chowdhry 50 chrd; 28cndr; 3 ost;12.9 mos;et al.,11 otherNG201615*(IV)sarcoma;LOC: T/LNG; NG; 48DeLaney 29 chrd; 14cndr; 1 ost; 6mos; NGet al.,other; LOC:200916*(IV)11 T, 13 L,26 SChenet al.,201313*(IV)Beddok et 41 chrd; LOC:100% Sal., 202112(IV)Austin et Recurrent55% M; 39al., 199345lesions; 10yrs; NG;(IV)chrd; 1 cndr;76.1 cm3LOC: 100% CAuthors& Year(LOE)NA15 R0/R1, 15R2, 11 noopNGOpOutcomeOSLC: 79% LFU;mets: 13.5%3 yrs; 19.5%5 yrsNGNGPFS, DFS,DSS,&/or RFS91.7% 3 DFS: 3-yr 77.2%;yrs;DSS 5-yr78.1%72.0%, 3-yr5 yrs95.7%, 5-yr81.5%; PFS3-yr 90.4%,5-yr 79.8%NGNGLC: 36% 1 yr;NG18% 2 yrs;mets: NG; LR:100% LFU;64% 1 yrLC: 90% 2 yrs; 96% 275% 5 yrs;yrs;mets: 11%80% 52 yrs; 27%yrs5 yrs; LR:19.5% LFULC& MetsTD med 70.2 RBE; 70% R0; 15% LC: NG; mets:frx NG; time NG;R1/R2;15% med10% got nilotinib15% biopsy10.7 mosw/ RTonlyTD med 70.2 RBE; 16 ops,LC: NG; mets:86.9% 5NGfrx NG; time NG;margin NG;NG; LR:yrs7.5 Gy 90Y or 1052 no op10.3% LFUGy 192Ir duralplaque in 10/68TD med 76.6 RBE; 8 R0; 17 R1; LC: 98% 1 yr;98% 1RFS: 94% 1 yr;frx 1.8 RBE;12 R2;84% 3 yrs;yr;68% 3 yrs;time: 2 wks13 biopsy78% 5 yrs;87%63% 5 yrspreop (S) or 6only; inmets: NG; LR:3 yrs;wks (spine); 7.5strumenta18% LFU87% 5Gy 90Y or 10 Gytion in 16yrs192Ir dural plaquein 3 pts, 2 pts,respectivelyTD med 77.4 RBE;frx 1.8–2 RBE; 5days/wk med60 daysTD med 68.4 RBE;frx 1.8–2 RBE;med 38 RBE; 5days/wk 7–8wksTD 70–73.8 RBE;frx 1.8–2 RBE;med 64 days;28 prRT/phRTcombo; 13 phRTonlyRTRegimenTABLE 2. Series outcomes for patients treated with combined proton/photon therapy regimensToxicityNGLateCONTINUED ON PAGE 7 »Overall: 10%; 31% 6yrs; 28% grd 3 6yrs; neurop: 4% grd3; sacral frac: 2% grd3; GU: 2% grd 3; GI:2% grd 3Overall: 1 grd 3;sacral frac: 1grd 3NGNGOverall: NG; neurop: Overall: NG; neurop:11.7%7.1% grd 2 5 yrs;19.1% 6 yrs, 8 yrsNGOverall: 100%; 7%Overall: 82–100%; 4%grd 3; skin:grd 3; skin: 45%;100%; 7% grd 3;GU: 14–19%; pain:neurop: 17% grd34% grd 1; 7% grd 2;1; pain: 54% grd2% grd 31; 2.4% grd 2; GU:5–15% grd 1Overall: NG; skin:Overall: 100%; 0% grdNG; mucositis: 3; 8 sacral frac;8.3%; GI: 17–29%skin: 100% grd 1–2;GU: 8.3%; GI: 16.7%;neurop 13%NGAcuteNGNGNGNGNGVolRespPennington et al.Neurosurg Focus Volume 50 May 2021Unauthenticated Downloaded 04/21/22 06:53 PM UTC
Neurosurg Focus Volume 50 May 202162% M; 53.2yrs; 47mos; NG126 chrd; LOC:16 T, 40 L,71 SOst osteosarcoma.* Massachusetts General Hospital.Rotondoet al.,20151*(IV)Parket al.,200620*(IV)63% M; 58yrs; 99.6mos; NG93.3% 2yrsRFS: 51.9% 2yrsLC: 96.9% 3 yrs; 89.1% 3 DSS: 97.2% 385.4% 5 yrs;yrs;yrs; 89.4%5 yrsmets: 11.7%81.9%3 yrs; 20.2%5 yrs5 yrsLC: 58% 2 yrs;LR: 63.2%;mets: NG84% 5RFS: 64% 5 yrs;yrs;52% 8 yrs65% 8yrsOSPFS, DFS,DSS,&/or RFSTD med 73 RBE;5 R0; 16 R1/2; LC: 71.7% 5 yrs; 82.5%DFS: 60.5% 5frx med 39 RBE;6 no op57.5% 10 yrs;5 yrs;yrs; 48.6%med 67 daysmets: 24%62.5%10 yrsmed 86 mos;10 yrsLR: 41% LFUTD med 72.4 RBE; 27% R0; 45% LC: 62% 5 yrs;81% 5NGfrx 1.8–2 RBE;R1; 24%49% 10 yrs;yrs;11–25 daysR2; 5%mets: 23% 553%preop 10–11unknownyrs; 37% 1010 yrsdays postop; 7yrspts w/ 10 Gy 90Y& 4 w/ 42 Gy192I intraop duralplaqueNATD med 77.4 RBE;frx 1.8–2 RBE;NG27 chrd; LOC:100% SNGTD med 70 RBE; frx2 RBE; 7 wks;14 prRT only;5 prRT/phRTcomboHollidayet al.,201518(IV)LC& Mets8 R0; 17 R1; LC: 81% 5 yrs;12 R2;74% 8 yrs;13 biopsymets: 8%only; instrumentation in 16OpOutcome13 chrd postM: 47%; NG;rsxn; 6 cndr34.5 mos;post-rsxn;NGLOC: 6mobile spine;13 S53% M; 67Kaboliza- 40 unresecchrd; LOC: 9yrs; 50deh et al.,C, 1 T, 3 L,mos; 174201719*(IV)27 Scm3RTRegimenTD med 76.6 RBE(w/ 7.5 Gy 90Y or10 Gy 192Ir duralplaque in 3 pts);frx 1.8 RBE; 2wks preop (S) or6 wks (spine)Pt Demogr:Sex; MedAge; Med FU;NeuropathologyMed CTV29 chrd; 14NG; NG; 7.3cndr; 1 ost; 6yrs; NGother; LOC:11 T, 12 L,27 SDeLaneyet al.,201417*(IV)Authors& Year(LOE)TABLE 2. Series outcomes for patients treated with combined proton/photon therapy regimens» CONTINUED FROM PAGE 6Overall: NG; sacralfrac: 1 grd 3AcuteNGLateOverall: 13% grd 3; Acute & late toxicitieswound infection:pooled8–13% grd 3;sacral frac: 5%grd 3; neurop:3% grd 3; GI: 1%grd 3; 1 secondary malignancyNot separated from opcomplicationsOverall: NG; 25 sacralfrac; neurop: 8%; GU:5%; GI: 3%Overall: 16% 5 yrs; 19%8 yrs; grd 3 10%5 yrs; 13% 8 yrs;RT-induced sarcomain 1; neurop: 2 grd3; GU: 4% grd 3; 6%sacral frac (4% grd 2,2% grd 3); GI: 2% grd3; other: 4% grd 1NGToxicityOverall: 84%; 16% grd 3;skin: 68% grd1, 16% grd 2;esophagitis: 21%grd 1–2Med max Overall: NG; GI:43.2%; med10–23%; mucosi 20% 6tis: 13%mos; 36%1 yr; 55%2 yrs; 64%36–60 mosNGNot separated fromop complicationsNGNGVolRespPennington et al.7Unauthenticated Downloaded 04/21/22 06:53 PM UTC
880% M; 66 yrs;30 mos; 556cm368% M; 66Imai et al., 188 unresecchrd; no prioryrs; 62 mos;201627‡(IV)radiation; nomean 345cm3instrumentation; LOC:100% S72% M; 66 yrs;Imai et al., 95 unresecchrd; 11 w/42 mos; 370201126‡(IV)prior op;cm3LOC: 100% S76% M; 66 yrs;Imai et al., 38 unresecchrd; 8 w/80 mos; 523201025‡(IV)prior op;cm3LOC: 100% SImai et al., 30 chrd; LOC:100% S200424‡(IV)219 chrd w/o69% M; 67 yrs;Demizuprior op;56 mos; NGet al.,LOC: 100% S202123†‡§(IV)68% M; 61 yrs;60 mos; 182cm3Pt Demogr: Sex;Med Age; MedNeuropathology FU; Med CTVBostel et 68 chrd; LOC:al., 202021*100% S(IV)Authors& Year(LOE)14 R0/R1rsxn; 26R2 rsxn;28 no opOpOutcomeTD 67.2 RBE in 143;NA70.4 RBE in 75;79.2 RBE in 1; frx2.2–4.4 RBE; 4days/wk 4 wksTD med 70.4 RBE; all 0 R0; 2 R1;pts had 16 frx; 4.43 R2; 2RBE; 4 days/wk unknown;4 wks23 no opTD 54.8 RBE in 1;3 R1 rsxn; 264.0 RBE in 1;R2 rsxn; 370.4 RBE in 29;unknown73.6 RBE in 7; allrsxn; 30had 16 frx; 4 days/no opwk 4 wksTD 54.8 RBE in 1 pt;NA64.0 RBE in 1 pt;73.6 RBE in 7 pts;86 RBE in 86 pts;all had 16 frx; 4days/wk 4 wksTD 64.0 RBE in 1 pt;NA67.2 RBE in 106pts; 70.4 RBE in74 pts; 73.6 RBEin 7 pts; all pts had16 frx; 4 days/wk 4 wksTD med 66 RBE;60 RBE in 16; 63RBE in 2; 64 RBEin 14; 66 RBE in14; frx 3–4 RBE;NG; 22 w/ phRT;46 CIRT aloneRTRegimenTABLE 3. Series describing outcomes for patients treated with CIRTOSPFS, DFS,DSS, &/orRFS86% 5 yrsNGPFS 76% 3yrs; 54%5 yrsLC: 77.2% 5 yrs; 81.1% 5 yrs; DFS: 50.3%52.0% 10 yrs;66.8%5 yrs,LR: 22%; mets:10 yrs;31.3% 1032% 5 yrs; medpostrecuryrstime to mets 34rence:mos52% 3 yrs,52% 5 yrsLC: 88% 5 yrs;mets: NG; LR:6.3% med 35mosLC: 95% 3 yrs;86% 5 yrs;89% 5 yrs;med 70mets: 39%mosLFU; med timeto mets 40 mosLC: 90% 1 yr;97% 1 yr;PFS 90% 180% 2 yrs;97% 2 yrs;yr; 80% 265% 3 yrs; 53%yrs; 65%86% 3 yrs;5 yrs; mets: 9%74% 5 yrs3 yrs;1 yr; 19% 2 yrs;53% 529% 3 yrs; 52%yrs5 yrs; LR: 46%med 25 mosLC: 72% 5 yrs;84% 5 yrs PFS 48% 5mets: 9%;yrsLR: 18% ®ional/distantin 27%LC: 96% 5 yrs;52% 5 yrs94% 5 yrsmets: 7% 1 yr;23% LFULC& MetsNGNGNGNGNGNGVolRespOverall: 59%; 21%grd 3; 49%sacral frac (16%w/ grd 3); neurop: 9%; 5% grd 3; GI: 3% (bothgrd 2); skin: 9%(all grd 1)Overall: 6% grd 3;myositis: grd 3 in3; pain: grd 3 in 2;skin: grd 2 in 2LateNGOverall: NG; skin:7% grd 3CONTINUED ON PAGE 9 »Overall: 89%; 3.2% grd 3;neurop: 11% grd1, 7% grd 2, 3%grd 3; skin: 89%grd 1, 6% grd 2,2% grd 3–4; GI:2% grd 1Overall: NG; skin:4% grd 3; 4% grd4; GI: 2% grd 1Overall: NG; skin:13% grd 3; GI:3% grd 3; neurop: 20% grd 3Overall: 26%;Overall: 5%; 5% 13% grd 3;grd 3; skin: 4%skin: 7% grd 3;grd 3; 1 sacral4% grd 4; neuro
nEURoSURGIcAl FocUS Neurosurg Focus 50 (5):E17, 2021 E n bloc resection with negative margins (R0 resec- tion) improves local control (LC) and disease-free survival (DFS) in patients with chordoma and pri-mary sarcomas of the spinal column and sacrum.1–5 R0 resection may also improve overall survival (OS).1,6