Transcription
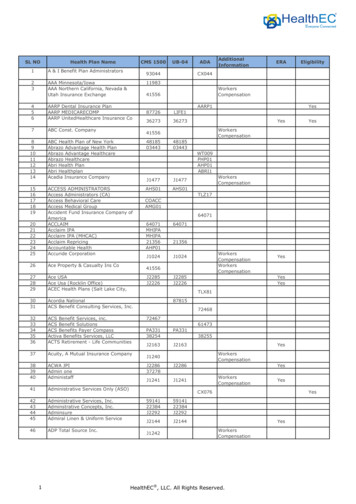
2021ComprehensiveFormularyAetna Medicare(List of Covered Drugs)GRP B2 Plus5 TierPLEASE READ: THIS DOCUMENT CONTAINS INFORMATIONABOUT THE DRUGS WE COVER IN THIS PLAN.This formulary was updated on 10/01/2020. For more recent information or other questions,please contact Aetna Medicare Member Services at 1-888-267-2637or for TTY users: 711, 8 a.m. to 9 p.m., E.S.T., Monday through Friday, or visitAetnaRetireePlans.com choose “Manage your prescription drugs”.Formulary ID Number: 21115 Version 8Updated 10/01/20
Table of contentsMail-order Pharmacy3What is the Aetna MedicareComprehensive Formulary?4Can the Formulary (drug list) change?4How do I use the Formulary?5What are generic drugs?5Are there any restrictions on my coverage?5What if my drug is not on the Formulary?6How do I request an exception to the AetnaMedicare Formulary?6What do I do before I can talk to my doctor aboutchanging my drugs or requesting an exception?7For more information7Aetna Medicare Formulary8Drug tier copay levels9Formulary key10Drug list10Index of Drugs90Enhanced drug list2110Updated 10/01/20
Aetna Medicare is a HMO, PPO plan with a Medicare contract. Enrollment in our plans depends oncontract renewal. Members who get “Extra Help” are not required to fill prescriptions at preferrednetwork pharmacies in order to get Low Income Subsidy (LIS) copays.See Evidence of Coverage for a complete description of plan benefits, exclusions, limitations andconditions of coverage. Plan features and availability may vary by service area.Mail-order PharmacyFor mail order, you can get prescription drugsshipped to your home through the networkmail-order delivery program. Typically,mail-order drugs arrive within 10 days. Youcan call 1-888-267-2637 (TTY: 711) 8 a.m. to9 p.m., E.S.T., Monday through Friday, if youdo not receive your mail-order drugs withinthis timeframe. Members may have theoption to sign up for automated mail-orderdelivery.ATTENTION: If you speak Spanish or Chinese,language assistance services, free of charge,are available to you. Call the number on yourID card.ATENCIÓN: Si habla español, tiene a sudisposición servicios gratuitos de asistencialingüística. Llame al número que figura en sutarjeta de 您的會員身分卡上的電話號碼。Note to existing members: Thisformulary has changed since last year.Please review this document to make surethat it still contains the drugs you take.When this drug list (formulary) refers to “we,”“us”, or “our,” it means Aetna Medicare. Whenit refers to “plan” or “our plan,” it meansAetna.This document includes a list of the drugs(formulary) for our plan which is current as of10/01/2020. For an updated formulary, pleasecontact us. Our contact information, alongwith the date we last updated the formulary,appears on the front and back cover pages.You must generally use networkpharmacies to use your prescription drugbenefit. Benefits, formulary, pharmacynetwork, and/or copayments/coinsurancemay change on January 1, 2022, and from timeto time during the year. You will receive noticewhen necessary.Updated 10/01/203
What is the Aetna MedicareComprehensive Formulary?A formulary is a list of covered drugs selectedby our plan in consultation with a team ofhealth care providers, which represents theprescription therapies believed to be anecessary part of a quality treatment program.We will generally cover the drugs listed in ourformulary as long as the drug is medicallynecessary, the prescription is filled at an AetnaMedicare network pharmacy, and other planrules are followed. For more information onhow to fill your prescriptions, please reviewyour Prescription Drug Schedule of CostSharing.Can the Formulary (drug list) change?Most changes in drug coverage happen onJanuary 1, but we may add or remove drugs onthe Drug List during the year, move them todifferent cost sharing tiers, or add newrestrictions. We must follow Medicare rules inmaking these changes.Changes that can affect you this year: In thebelow cases, you will be affected by coveragechanges during the year: New generic drugs. We may immediatelyremove a brand name drug on our Drug Listif we are replacing it with a new generic drugthat will appear on the same or lower costsharing tier and with the same or fewerrestrictions. Also, when adding the newgeneric drug, we may decide to keep thebrand name drug on our Drug List, butimmediately move it to a different costsharing tier or add new restrictions. If youare currently taking that brand name drug,we may not tell you in advance before wemake that change, but we will later provideyou with information about the specificchange(s) we have made.4 If we make such a change, you or yourprescriber can ask us to make an exceptionand continue to cover the brand name drugfor you. The notice we provide you will alsoinclude information on how to request anexception, and you can also findinformation in the section below entitled“How do I request an exception to theAetna Medicare Formulary?” Drugs removed from the market. If theFood and Drug Administration (FDA) deems adrug on our formulary to be unsafe or thedrug’s manufacturer removes the drug fromthe market, we may immediately remove thedrug from our formulary and provide noticeto members who take the drug. Other changes. We may make otherchanges that affect members currentlytaking a drug. For instance, we may add ageneric drug that is not new to the market toreplace a brand name drug currently on theformulary or add new restrictions to thebrand name drug or move it to a differentcost sharing tier or both. Or we may makechanges based on new clinical guidelines. Ifwe remove drugs from our formulary, or addprior authorization, quantity limits and/orstep therapy restrictions on a drug or move adrug to a higher cost sharing tier, we mustnotify affected members of the change atleast 30 days before the change becomeseffective, or at the time the memberrequests a refill of the drug, at which timethe member will receive a 30-day supply ofthe drug. If we make these other changes, you oryour prescriber can ask us to make anexception and continue to cover the brandname drug for you. The notice we provideyou will also include information on how torequest an exception, and you can also findinformation in the section below entitled“How do I request an exception to theAetna Medicare Formulary?”Updated 10/01/20
Changes that will not affect you if you arecurrently taking the drug.Generally, if you are taking a drug on our 2021formulary that was covered at the beginning ofthe year, we will not discontinue or reducecoverage of the drug during the 2021 coverageyear except as described above. This meansthese drugs will remain available at the samecost sharing and with no new restrictions forthose members taking them for the remainderof the coverage year. You will not get directnotice this year about changes that do notaffect you. However, on January 1 of the nextyear, such changes would affect you, and it isimportant to check the Drug List for the newbenefit year for any changes to drugs.The enclosed formulary is current as of10/01/2020. To get updated information aboutthe drugs covered by our plan, please contactus. Our contact information appears on thefront and back cover pages.How do I use the Formulary?There are two ways to find your drug withinthe formulary:Medical ConditionThe formulary begins on page 10. The drugsin this formulary are grouped into categoriesdepending on the type of medical conditionsthat they are used to treat. For example, drugsused to treat a heart condition are listed underthe category, “Cardiovascular”. If you knowwhat your drug is used for, look for thecategory name in the list that begins onpage 10. Then look under the categoryname for your drug.Alphabetical ListingIf you are not sure what category to lookunder, you should look for your drug in theIndex that begins on page 90. The Indexprovides an alphabetical list of all of the drugsincluded in this document. Both brand namedrugs and generic drugs are listed in theIndex. Look in the Index and find your drug.Next to your drug, you will see the pagenumber where you can find coverageinformation. Turn to the page listed in theIndex and find the name of your drug in thefirst column of the list.What are generic drugs?Our plan covers both brand name drugs andgeneric drugs. A generic drug is approved bythe FDA as having the same active ingredientas the brand name drug. Generally, genericdrugs cost less than brand name drugs.Are there any restrictions on mycoverage?Some covered drugs may have additionalrequirements or limits on coverage. Theserequirements and limits may include: Prior Authorization: Our plan requires youor your physician to get prior authorizationfor certain drugs. This means that you willneed to get approval from us before you fillyour prescriptions. If you don’t get approval,we may not cover the drug. Quantity Limits: For certain drugs, our planlimits the amount of the drug that we willcover. For example, our plan provides 30tablets per 30 days per prescription forrosuvastatin. This may be in addition to astandard one-month or three-month supply.Updated 10/01/205
Step Therapy: In some cases, our planrequires you to first try certain drugs totreat your medical condition before we willcover another drug for that condition. Forexample, if Drug A and Drug B both treatyour medical condition, we may not coverDrug B unless you try Drug A first. If Drug Adoes not work for you, we will then coverDrug B. You can ask us to make an exception andcover your drug. See below for informationabout how to request an exception.You can find out if your drug has anyadditional requirements or limits bylooking in the formulary that begins onpage 10. You can also get more informationabout the restrictions applied to specificcovered drugs by visiting our Website. Wehave posted online documents that explainour prior authorization and step therapyrestrictions. You may also ask us to send youa copy. Our contact information, along withthe date we last updated the formulary,appears on the front and back cover pages. You can ask us to cover a drug even if it isnot on our formulary. If approved, this drugwill be covered at a pre-determined costsharing level, and you would not be able toask us to provide the drug at a lower costsharing level.You can ask us to make an exception to theserestrictions or limits or for a list of other,similar drugs that may treat your healthcondition. See the section, “How do I requestan exception to the Aetna Medicareformulary?” on page 6 for informationabout how to request an exception.What if my drug is not onthe Formulary?If your drug is not included in thisformulary (list of covered drugs), youshould first contact Member Services andask if your drug is covered.If you learn that our plan does not cover yourdrug, you have two options: You can ask Member Services for a list ofsimilar drugs that are covered by our plan.When you receive the list, show it to yourdoctor and ask him or her to prescribe asimilar drug that is covered by our plan.6How do I request an exception to theAetna Medicare Formulary?You can ask us to make an exception to ourcoverage rules. There are several types ofexceptions that you can ask us to make. You can ask us to cover a formulary drug ata lower cost sharing level if this drug is noton the specialty tier. If approved this wouldlower the amount you must pay for yourdrug. You can ask us to waive coveragerestrictions or limits on your drug. Forexample, for certain drugs, our plan limitsthe amount of the drug that we will cover. Ifyour drug has a quantity limit, you can askus to waive the limit and cover a greateramount.Generally, we will only approve your requestfor an exception if the alternative drugsincluded on the plan’s formulary, the lowercost sharing drug or additional utilizationrestrictions would not be as effective intreating your condition and/or would causeyou to have adverse medical effects.You should contact us to ask us for an initialcoverage decision for a formulary, tiering orutilization restriction exception. When yourequest a formulary, tiering or utilizationrestriction exception you should submit astatement from your prescriber orphysician supporting your request.Updated 10/01/20
Generally, we must make our decision within72 hours of getting your prescriber’ssupporting statement. You can request anexpedited (fast) exception if you or yourdoctor believe that your health could beseriously harmed by waiting up to 72 hoursfor a decision. If your request to expedite isgranted, we must give you a decision no laterthan 24 hours after we get a supportingstatement from your doctor or otherprescriber.What do I do before I can talk to mydoctor about changing my drugs orrequesting an exception?As a new or continuing member in our planyou may be taking drugs that are not on ourformulary. Or, you may be taking a drug thatis on our formulary but your ability to get it islimited. For example, you may need a priorauthorization from us before you can fill yourprescription. You should talk to your doctor todecide if you should switch to an appropriatedrug that we cover or request a formularyexception so that we will cover the drug youtake. While you talk to your doctor todetermine the right course of action for you,we may cover your drug in certain casesduring the first 90 days you are a member ofour plan.For each of your drugs that is not on ourformulary or if your ability to get your drugs islimited, we will cover a temporary 30-daysupply. If your prescription is written for fewerdays, we’ll allow refills to provide up to amaximum 30 day supply of medication. Afteryour first 30-day supply, we will not pay forthese drugs, even if you have been a memberof the plan less than 90 days.If you are a resident of a long-term carefacility, we will allow you to refill yourprescription until we have provided you with a31-day transition supply, consistent withdispensing increment, (unless you have aprescription written for fewer days). We willcover more than one refill of these drugs forthe first 90 days you are a member of ourplan. If you need a drug that is not on ourformulary or if your ability to get your drugs islimited, but you are past the first 90 days ofmembership in our plan, we will cover a31-day emergency supply of that drug (unlessyou have a prescription for fewer days) whileyou pursue a formulary exception.If you experience a change in your setting ofcare (such as being discharged or admitted toa long-term care facility), your physician orpharmacy can request a one-timeprescription override. This one-time overridewill provide you with temporary coverage (upto a 30-day supply) for the applicable drug(s).For more informationFor more detailed information about yourplan's prescription drug coverage, pleasereview your Evidence of Coverage and otherplan materials.If you have questions about our plan, pleasecontact us. Our contact information, alongwith the date we last updated the formulary,appears on the front and back cover pages.If you have general questions about Medicareprescription drug coverage, please callMedicare at 1-800-MEDICARE(1-800-633-4227) 24 hours a day/7 days aweek. TTY users should call 1-877-486-2048.Or, visit http://www.medicare.gov.Updated 10/01/207
Aetna Medicare FormularyThe comprehensive formulary that begins onpage 10 provides coverage informationabout the drugs covered by our plan. If youhave trouble finding your drug in the list, turnto the Index that begins on page 90.The first column of the chart lists the drugname. Brand name drugs are capitalized (e.g.,SYNTHROID) and generic drugs are listed inlower-case italics (e.g., levothyroxine).The information in the Requirements/Limitscolumn tells you if Aetna Medicare has anyspecial requirements for coverage of your drug.QLQuantity LimitsPAPrior AuthorizationSTStep TherapyLALimited AccessMOMail-order DeliveryB/DPart B vs. D Prior AuthorizationQL: Quantity Limits. For certain drugs, ourplan limits the amount of the drug that we willcover. For example, our plan provides 30tablets per 30 days per prescription forrosuvastatin.LA: Limited Access. These prescriptions maybe available only at certain pharmacies. Formore Information, consult your PharmacyDirectory or call Aetna Member Services at1-888-267-2637 (TTY: 711), 8 a.m. to 9 p.m.,E.S.T., Monday through Friday.MO: Mail Order. For certain kinds of drugs, youcan use CVS Caremark Mail Service Pharmacy.Generally, the drugs available through mailorder are drugs that you take on a regularbasis, for a chronic or long-term medicalcondition. The drugs available through ourplan’s mail-order service are marked as “MO”in our Drug List. For more information, consultyour Pharmacy Directory or call Aetna MemberServices at 1-888-267-2637 (TTY: 711), 8 a.m.to 9 p.m., E.S.T., Monday through Friday.B/D: Part B versus Part D. This prescriptiondrug has a Part B versus Part D administrativeprior authorization requirement. This drugmay be covered under Medicare Part B or Ddepending upon the circumstances.Information may need to be submitteddescribing the use and setting of the drug tomake the determination.PA: Prior Authorization. Our plan requires youor your provider to get prior authorization forcertain drugs. This means that you will needto get approval from us before you fill yourprescriptions. If you don't get approval, wemay not cover the drug.ST: Step Therapy. In some cases, our planrequires you to first try certain drugs to treatyour medical condition, before we will coveranother drug for that condition. For example,if Drug A and Drug B both treat your medicalcondition, we may not cover Drug B unlessyou try Drug A first. If Drug A does not workfor you, we will then cover Drug B.8Updated 10/01/20
Drug tier copay levelsThis 2021 comprehensive formulary is a listingof brand-name and generic drugs. AetnaMedicare’s 2021 formulary covers most drugsidentified by Medicare as Part D drugs, andyour copay may differ depending upon thetier at which the drug resides.The copay tiers for covered prescriptionmedications are listed below. Copay amountsand coinsurance percentages for each tiervary by Aetna Medicare plan. Look in the 2021Prescription Drug Benefits Chart (ThePrescription Drug Schedule of Cost Sharing)that was included in your Evidence ofCoverage (EOC) packet.Copay tierType of drugTier 1Preferred Generic DrugsTier 2Generic DrugsTier 3Preferred Brand DrugsTier 4Non-Preferred Brand DrugsTier 5Specialty DrugsYou may have drug coverage in theCoverage Gap StageThere are four “drug payment stages” of aMedicare Prescription Drug Plan. How muchyou pay for a Part D drug depends on whichdrug payment stage you are in. Your plan mayinclude supplemental coverage for somedrugs during the Coverage Gap stage of theplan. Look in the 2021 Prescription DrugBenefits Chart (Prescription Drug Schedule ofCost Sharing) that was included in your EOCpacket. The Prescription Drug Benefits Chartwill tell you if your plan provides coverage inthe gap, and how much you will pay forcovered drugs. If you need assistance findingthis information, call the number on the backof your ID card.Updated 10/01/209
Key*Drug nameDrug tierRequirements/LimitsUPPERCASE Brand-nameprescription drugs1, 2, 3, 4, 5 Copay tier levelQL Quantity LimitPA Prior AuthorizationST Step TherapyLA Limited AccessMO Mail-order DeliveryB/D Part B vs. Part DLowercase italics GenericmedicationsDrug nameDrug tier Requirements/LimitsANALGESICSGOUTallopurinol tabs1MOcolchicine2QL (120 EA per 30 days) MOfebuxostat2ST MOMITIGARE3QL (60 EA per 30 days) MOprobenecid2MOprobenecid/colchicine2MOcelecoxib caps 400mg2QL (30 EA per 30 days) MOcelecoxib caps 100mg, 200mg, 50mg2QL (60 EA per 30 days) MOdiclofenac potassium2QL (120 EA per 30 days) MOdiclofenac sodium dr2MOdiclofenac sodium er2MOdiclofenac c2MOetodolac er2MOFENOPROFEN CALCIUM CAPS400MG4MOfenoprofen calcium tabs2MOflurbiprofen tabs 100mg2MOibu tabs 600mg, 800mg2ibuprofen2MOketoprofen er2MOketoprofen caps 50mg2ketoprofen caps 25mg2NSAIDSMO* You can find information on what the symbols and abbreviations on this table mean by going topage 8.10Updated 10/01/20
Drug nameDrug tier Requirements/Limitsketorolac tromethamine inj 15mg/ml, 230mg/ml, 60mg/2mlQL (20 ML per 30 days) PA MOketorolac tromethamine tabs 10mg2QL (20 EA per 30 days) PA MOmeclofenamate sodium2MOmeloxicam1MOnabumetone2MOnaproxen dr2MONAPROXEN SODIUM CR TABS375MG4MOnaproxen sodium er tabs 500mg2MOnaproxen sodium tabs 275mg,550mg2MOnaproxen/esomeprazole magnesium5MOnaproxen tabs1MOnaproxen Obuprenorphine transdermal patch2QL (4 EA per 28 days) PA MOfentanyl transdermal patch2QL (10 EA per 30 days) PA MOHYSINGLA ER3QL (30 EA per 30 days) PA MOMETHADONE HCL INJ5PAmethadone hcl oral soln2QL (450 ML per 30 days) PA MOmethadone hcl tabs2QL (90 EA per 30 days) PA MOmethadone hcl conc2QL (90 ML per 30 days) PA MOmorphine sulfate er cp24 (genericAvinza) 120mg, 30mg, 45mg, 60mg,75mg, 90mg2QL (30 EA per 30 days) PA MOmorphine sulfate er cp24 (genericKadian) 100mg, 10mg, 20mg, 30mg,40mg, 50mg, 60mg, 80mg2QL (60 EA per 30 days) PA MOmorphine sulfate er tbcr 100mg,200mg, 30mg, 60mg2QL (60 EA per 30 days) PA MOmorphine sulfate er tbcr 15mg2QL (90 EA per 30 days) PA MOTRAMADOL HCL ER CP24 100MG,200MG, 300MG4QL (30 EA per 30 days) PA MOOPIOID ANALGESICS, LONG-ACTINGUpdated 10/01/2011
Drug nameDrug tier Requirements/Limitstramadol hcl er tb242QL (30 EA per 30 days) PA MOacetaminophen/codeine tabs2QL (180 EA per 30 days) MOacetaminophen/codeine soln2QL (2700 ML per 30 days) MObutorphanol tartrate nasal soln2QL (5 ML per 30 days) MObutorphanol tartrate inj 1mg/ml2butorphanol tartrate inj 2mg/ml2MOCODEINE SULFATE TABS 30MG4QL (180 EA per 30 days)CODEINE SULFATE TABS 15MG,60MG4QL (180 EA per 30 days) MOendocet tabs 325mg; 10mg, 325mg;2.5mg, 325mg; 5mg, 325mg; 7.5mg2QL (180 EA per 30 days)fentanyl citrate oral transmucosallozenge5QL (120 EA per 30 days) PA MOhydrocodone bitartrate/acetaminophen soln 325mg/15ml;7.5mg/15ml2QL (2700 ML per 30 days) MOhydrocodone bitartrate/acetaminophen tabs 300mg; 10mg,300mg; 5mg, 300mg; 7.5mg2QL (180 EA per 30 days) MOhydrocodone/acetaminophen tabs325mg; 10mg, 325mg; 5mg, 325mg;7.5mg2QL (180 EA per 30 days) MOhydrocodone/ibuprofen tabs 10mg;200mg, 5mg; 200mg, 7.5mg; 200mg2QL (150 EA per 30 days) MOhydromorphone hcl tabs2QL (180 EA per 30 days) MOhydromorphone hcl liqd2QL (600 ML per 30 days) MOHYDROMORPHONE HCL INJ 1MG/ML, 4MG/ML4B/D MOhydromorphone hcl inj 10mg/ml2B/Dhydromorphone hcl inj 2mg/ml2B/D MOHYDROMORPHONEHYDROCHLORIDE PF INJ 1MG/ML4B/DHYDROMORPHONEHYDROCHLORIDE PF INJ 4MG/ML4B/D MOhydromorphone hydrochloride pf inj2mg/ml, 50mg/5ml2B/Dlorcet2QL (180 EA per 30 days)lorcet hd2QL (180 EA per 30 days)OPIOID ANALGESICS, SHORT-ACTING12Updated 10/01/20
Drug nameDrug tier Requirements/Limitslorcet plus tabs 325mg; 7.5mg2QL (180 EA per 30 days)morphine sulfate tabs2QL (180 EA per 30 days) MOMORPHINE SULFATE INJ 10MG/4ML PF, 25MG/ML PF, 2MG/ML PF,4MG/ML PF, 50MG/ML, 5MG/ML PF,8MG/ML PFB/Dmorphine sulfate iv inj 0.5mg/ml,10mg/ml, 1mg/ml, 4mg/ml, 8mg/ml2B/Dmorphine sulfate pf inj 1mg/ml2B/D MOmorphine sulfate oral soln100mg/5ml2QL (180 ML per 30 days) MOmorphine sulfate oral soln 10mg/5ml, 220mg/5mlQL (900 ML per 30 days) MOnalbuphine hcl inj 10mg/ml, 20mg/ml 2MOoxycodone hcl caps2QL (180 EA per 30 days) MOoxycodone hydrochloride oral conc2QL (180 ML per 30 days) MOoxycodone hydrochloride soln2QL (900 ML per 30 days) MOoxycodone hydrochloride tabs 30mg2QL (120 EA per 30 days) MOoxycodone hydrochloride tabs 10mg,15mg, 20mg, 5mg2QL (180 EA per 30 days) MOoxycodone/acetaminophen tabs2325mg; 10mg, 325mg; 2.5mg, 325mg;5mg, 325mg; 7.5mgQL (180 EA per 30 days) MOoxycodone/aspirin tabs 325mg;4.835mg2QL (180 EA per 30 days) MOoxymorphone hydrochlorideimmediate release tabs2QL (180 EA per 30 days) MOtramadol hcl tabs 50mg2QL (240 EA per 30 days) MOtramadol hydrochloride/acetaminophen2QL (240 EA per 30 days) MOtramadol hydrochloride tabs 100mg2QL (120 EA per 30 days) MOANESTHETICSLOCAL ANESTHETICSlidocaine hcl inj 0.5%, 1%, 1.5%, 2%,4%2lidocaine hydrochloride pf inj 1%, 2%2ANTI-INFECTIVESANTI-INFECTIVES - MISCELLANEOUSalbendazole5Updated 10/01/20MO13
Drug name14Drug tier Requirements/LimitsALINIA5MOamikacin sulfate2MOatovaquone2PA MOaztreonam2MOCAYSTON5PA LAchloramphenicol inj 1gm2clindamycin hcl caps 300mg, 75mg2MOclindamycin hydrochloride caps150mg2MOclindamycin palmitate hcl2MOclindamycin phosphate/dextrose2clindamycin phosphate inj300mg/2ml, 9000mg/60ml2clindamycin phosphate inj600mg/4ml, 900mg/6ml2CLINDAMYCIN/SODIUM CHLORIDE4colistimethate inj2PA MOdapsone tabs 100mg, 25mg2MODAPTOMYCIN INJ 350MG5daptomycin inj 500mg5MOEMVERM5QL (12 EA per 365 days) MOertapenem2MOgentamicin sulfate pediatric2MOgentamicin sulfate/0.9% sodiumchloride inj 1.2mg/ml; 0.9%, 1mg/ml;0.9%, 2mg/ml; 0.9%2gentamicin sulfate/0.9% sodiumchloride inj 1.6mg/ml; 0.9%2MOgentamicin sulfate inj 40mg/ml2MOimipenem/cilastatin2MOisotonic gentamicin2MOivermectin2MOlinezolid tabs2QL (56 EA per 28 days) PA MOlinezolid oral susp5QL (1800 ML per 28 days) PA MOLINEZOLID INJ 600MG/300ML; 0.9%4PAlinezolid inj 600mg/300ml2PAmeropenem inj 500mg2meropenem inj 1gm2Updated 10/01/20MOMO
Drug nameDrug tier Requirements/Limitsmethenamine hippurate2MOMETHENAMINE MANDELATE4MOmetronidazole in nacl 0.79%2metronidazole caps 375mg2MOmetronidazole tabs 250mg, 500mg2MOneomycin tabs2MOnitrofurantoin macrocrystals2MOnitrofurantoin monohydrate2MOnitrofurantoin oral suspension2MOparomomycin caps2MOpentamidine isethionate inj2pentamidine isethionate inhalationsolr2B/Dpraziquantel2MOSIVEXTRO INJ5SIVEXTRO TABS5MOstreptomycin sulfate inj2MOSULFADIAZINE4MOsulfamethoxazole/trimethoprim ds1MOsulfamethoxazole/trimethoprim tabs1MOsulfamethoxazole/trimethoprim inj,susp2MOSYNERCID5tinidazole2MOtobramycin nebu 300mg/5ml2QL (280 ML per 56 days) PAtobramycin sulfate inj 1.2gm, 10mg/ml, 40mg/ml2tobramycin sulfate inj 1.2gm/30ml,80mg/2ml2MOtrimethoprim tabs1MOVANCOMYCIN HCL INJ 0.9%;1GM/200ML4vancomycin hcl inj 100gm, 10gm2vancomycin hydrochloride caps125mg2QL (120 EA per 30 days) MOvancomycin hydrochloride caps250mg5QL (240 EA per 30 days) MOUpdated 10/01/2015
Drug nameDrug tier Requirements/LimitsVANCOMYCIN HYDROCHLORIDEINJ 1.25GM, 1.5GM, 250MG,500MG/100ML4vancomycin hydrochloride inj 1gm,5gm, 750mg2vancomycin hydrochloride inj 500mg2VANCOMYCIN INJ BISOME5B/Damphotericin b2B/D MOcaspofungin acetate inj 70mg2caspofungin acetate inj 50mg5fluconazole2fluconazole in nacl 200mg; 0.9%2fluconazole in sodium chloride400mg; 0.9%2flucytosine5MOgriseofulvin microsize2MOgriseofulvin ultramicrosize2MOitraconazole2PA MOketoconazole tabs 200mg2PA MOmicafungin inj 50mg2micafungin inj 100mg5MYCAMINE INJ 50MG4MYCAMINE INJ 100MG5NOXAFIL5QL (630 ML per 30 days) MOnystatin tabs 500000unit2MOposaconazole dr5QL (93 EA per 30 days) MOterbinafine hcl tabs2QL (90 EA per 365 days) MOvoriconazole tabs2MOvoriconazole inj2PAvoriconazole oral susp2PA MOatovaquone/proguanil hcl2MOchloroquine phosphate2MOMOMOANTIMALARIALS16Updated 10/01/20
Drug nameDrug tier Requirements/LimitsCOARTEM4MOmefloquine hcl2MOprimaquine phosphate2MOquinine sulfate2PA MOabacavir2MOAPTIVUS SOLN5APTIVUS CAPS5MOatazanavir sulfate caps 150mg,300mg2MOatazanavir sulfate caps 200mg5MOCRIXIVAN4MOdidanosine caps 200mg, 250mg,400mg2MOEDURANT5MOefavirenz caps2MOefavirenz tabs5MOEMTRIVA3MOfosamprenavir calcium5MOFUZEON5INTELENCE TABS 25MG4INTELENCE TABS 100MG, 200MG5MOINVIRASE TABS5MOISENTRESS HD5MOISENTRESS PACK3MOISENTRESS TABS5MOISENTRESS CHEW 25MG3MOISENTRESS CHEW 100MG5MOlamivudine soln 10mg/ml2MOlamivudine tabs 150mg, 300mg2MOLEXIVA4MOnevirapine er tb24 100mg2nevirapine er tb24 400mg2nevirapine susp2nevirapine tabs2MONORVIR PACK, ORAL SOLN4MOPIFELTRO5MOANTIRETROVIRAL AGENTSUpdated 10/01/20MO17
Drug nameDrug tier Requirements/LimitsPREZISTA SUSP5QL (400 ML per 30 days) MOPREZISTA TABS 75MG4QL (480 EA per 30 days) MOPREZISTA TABS 150MG5QL (240 EA per 30 days) MOPREZISTA TABS 800MG5QL (30 EA per 30 days) MOPREZISTA TABS 600MG5QL (60 EA per 30 days) MORESCRIPTOR TABS 200MG4MOREYATAZ CAPS 150MG,200 MG,PACK5MOritonavir2MORUKOBIA5SELZENTRY SOLN5SELZENTRY TABS 25MG3SELZENTRY TABS 75MG5SELZENTRY TABS 150MG, 300MG5MOstavudine2MOtenofovir tabs2MOTIVICAY PD4TIVICAY TABS 10MG3MOTIVICAY TABS 25MG, 50MG5MOTROGARZO5LATYBOST4MOVIDEX EC CAPS 125MG4MOVIDEX PEDIATRIC4MOVIRACEPT TABS5MOVIREAD5MOzidovudine2MOabacavir sulfate/lamivudine2MOabacavir O5MOANTIRETROVIRAL COMBINATION AGENTS18Updated 10/01/20
Drug nameDrug tier ETRA TABS 100MG; 25MG4MOKALETRA TABS 200MG; 2MOODEFSEY5MOPREZCOBIX5MOSTRIBILD5MOSYMFI5MOSYMFI LO5MOSYMTUZA5MOTEMIXYS5MOTRIUMEQ5MOTRUVADA5QL (30 EA per 30 days) MOcycloserine5MOethambutol hydrochloride tabs400mg2MOisoniazid tabs1MOisoniazid inj2isoniazid syrp2MOPASER4MOPRETOMANID4QL (30 EA per 30 days) PAPRIFTIN4MOpyrazinamide2MOrifabutin2MOrifampin inj2rifampin caps2MORIFATER4MOSIRTURO TABS 20MG5PASIRTURO TABS 100MG5PA LATRECATOR4MOacyclovir sodium inj 50mg/ml2B/Dacyclovir caps 200mg2MOANTITUBERCULAR AGENTSANTIVIRALSUpdated 10/01/2019
Drug nameDrug tier Requirements/Limitsacyclovir susp 200mg/5ml2MOacyclovir tabs 400mg, 800mg2MOadefovir dipivoxil2QL (30 EA per 30 days) MOBARACLUDE4MOentecavir2QL (30 EA per 30 days) MOEPCLUSA5PAEPIVIR HBV SOLN4MOfamciclovir tabs 500mg2QL (21 EA per 30 days) MOfamciclovir tabs 125mg, 250mg2QL (60 EA per 30 days) MOganciclovir inj 500mg/10ml, 500mg2B/DHARVONI TABS5PAlamivudine tabs 100mg2MOMAVYRET5PAoseltamivir phosphate caps 30mg2QL (168 EA per 365 days) MOoseltamivir phosphate c
Aetna Medicare (List of Covered Drugs) GRP B2 Plus 5 Tier PLEASE READ: THIS DOCUMENT CONTAINS INFORMATION ABOUT THE DRUGS WE COVER IN THIS PLAN. This formulary was updated on 10/01/2020. For more recent information or other questions, please