Transcription
Managing Flaresand IBD Symptomsa
What’s InsideWhat is a flare?. 2Factors that may affect flaresand how to avoid them. 3Missed medications and incorrect dosing. 3Non-steroidal anti-inflammatorydrugs (NSAIDs). 3Antibiotics. 4Smoking. 4Stress. 4Food. 5Treating flares. 6What will your doctor doto treat your flare?. 6Managing flares.7Managing symptom discomfort. 9Questions for your doctor.10IBD flares in children.12Coping with flares.13Talking with others. 15Complications.16Knowledge and support are power!.16The Crohn’s & Colitis Foundation provides information foreducational purposes only, which is current as of the printdate. We encourage you to review this educational materialwith your healthcare professional, as this information shouldnot replace the recommendations, and advice of yourdoctor. The Foundation does not provide medical or otherhealthcare opinions or services. The inclusion of anotherorganization’s resources or referral to another organizationdoes not represent an endorsement of a particular individual,group, company, or product.
Having an inflammatorybowel disease (IBD)often means living withconcerns lurking justunder the surface ofeveryday thoughts: Will my condition flare up? What can I do when it does? How will I cope?These concerns are very common for peoplewith Crohn’s disease and ulcerative colitis, alsoknown as IBD. Even with medical treatment, aperson with IBD is likely to experience periodsof time when symptoms become active.This brochure will help you manage your lifewith a disease that can at times be painful,uncomfortable, inconvenient, or embarrassing.For more information on IBD symptoms, medications, diet, surgery, or disease management,please visit the Crohn’s & Colitis Foundation’swebsite at www.crohnscolitisfoundation.org.1
What is a flare?A flare is the reappearance of disease symptoms. The most common symptoms of Crohn’sdisease and ulcerative colitis are: Frequent and/or urgent bowel movements Diarrhea Bloody stool Abdominal pain Nausea and vomiting Weight lossPeople may also report symptoms such asfatigue, lack of appetite, joint aches, body aches,rashes, and eye problems, including pain, redness, or loss of vision. The symptoms of IBD varyfrom person to person, and may change overtime. Your specific symptoms will depend onwhether you have Crohn’s disease or ulcerativecolitis and, in many cases, on the location of thedisease within your gastrointestinal (GI) tract.Crohn’s disease and ulcerative colitis arecharacterized by times of active disease (whensymptoms are present) and times of remission(when little or no symptoms are present).Medical treatment is aimed at bringing theconditions into a state of remission and keepingit that way for as long as possible.Crohn’s Disease FlareUlcerative Colitis FlareColonoscopy pictures courtesy of Raluca Vrabie, MD2
Factors that mayaffect flares and howto avoid themThere are several factors that may impacta flare and/or make symptoms worse,including: Missing IBD medications or taking theincorrect dose Non-steroidal anti-inflammatory drugs(NSAIDs) Antibiotics Smoking Stress FoodMissed medications and incorrectdosingMany people with IBD take medications ona regular basis, even when the disease is inremission. Flares can occur when medicationsare not taken as prescribed (for example,skipping doses, weaning off medications). Ifyou are taking your medications as prescribedand still experiencing flares, speak with yourdoctor. Your doctor may suggest changing thedose, frequency or type of medication. If youhave missed doses of your medications or havestopped your medications and are now experiencing symptoms, talk with your doctor beforerestarting or increasing your medications onyour own.Non-steroidal anti-inflammatorydrugs (NSAIDs)NSAIDs, which include aspirin, naproxen (Aleve ),and ibuprofen (Motrin , Advil , Nuprin ), maylead to inflammation of the bowel and makesymptoms worse. Therefore, for mild pain or to3
reduce a fever, it is generally recommended thatpeople with IBD take acetaminophen (Tylenol )rather than an NSAID.AntibioticsAntibiotics are good for treating bacterialinfections, but they also alter the bacteriathat normally live in the intestine. Changes inthe balance of intestinal bacteria may causediarrhea (for example, antibiotic-associateddiarrhea) or may lead to excessive growth ofspecific bacteria that can cause inflammation.If you are taking an antibiotic and experience aflare of your IBD symptoms, it is importantto inform your doctor.SmokingSmoking cigarettes not only raises the risk fordeveloping Crohn’s disease, it also can triggerflares. People with Crohn’s disease who smoketend to have more disease activity, moresurgery, and a greater need for medications tocontrol their disease. Crohn’s disease patientswho have quit smoking report having fewerflare-ups and a reduced need for medicationsto control their disease.Surprisingly, the risk of developing ulcerativecolitis is decreased in current smokers compared with people who have never smoked. Thenumerous potential harmful health effects ofsmoking (e.g., cancer, heart disease) largely outweigh any benefits of smoking for people withulcerative colitis.StressIt is important to understand that physical andemotional stress do not cause IBD. However,stressful situations or strong emotions may impact IBD symptoms. For those people with IBDwho know that stress can be problematic, it maybe helpful to be prepared for this reaction andto learn some stress-management techniques.See page 9 for stress reduction techniques.4
FoodAlthough diet does not cause or cure IBD, paying attention to your diet may help you reducesymptoms, replace lost nutrients, and promotehealing. However, no one type of food or beverage aggravates symptoms for all people withCrohn’s disease or ulcerative colitis. Therefore,each person with IBD will need to determinewhich foods impact symptoms and which donot. Keeping a food journal may help you trackhow your diet relates to your symptoms.Abdominal pain and fever can cause loss ofappetite and weight loss. Diarrhea and rectalbleeding can rob the body of fluids, nutrients,and electrolytes. A well-balanced diet is necessary to prevent nutritional deficiency.In general, when experiencing a flare, it is bestto avoid greasy and fried foods, which cancause gas and diarrhea. Some people find thatfoods high in fiber, such as fruits, vegetablesand whole grains, can be problematic. Ratherthan eliminating these necessary foods fromyour diet, it may be helpful to eat onlythoroughly-cooked fruits and vegetables. Youmay also want to avoid foods that are likely tocause gas, such as beans, cabbage, broccoli,caffeine, and carbonated drinks. Eating smaller,more frequent meals may be helpful.Alcohol intake, whether moderate or in excess,may also make symptoms worse. Alcoholabstinence may not be required, but moderationis advised.If you find that particular foods affect yourIBD symptoms, talk to your doctor ordietitian. A registered dietitian can help youto plan a diet that works for you. If youneed resources to help you find a dietitian,contact the Foundation’s IBD Help Center atinfo@crohnscolitisfoundation.org.5
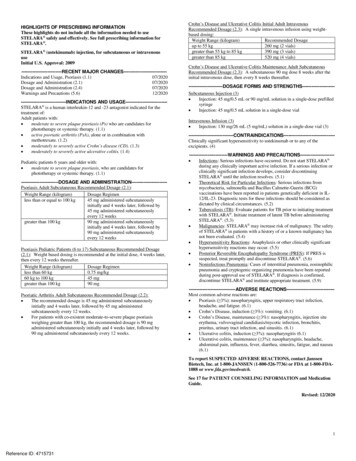
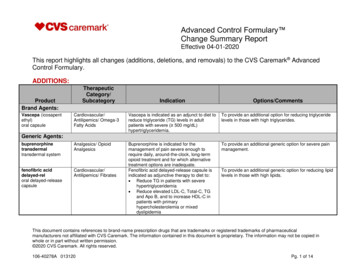
For more information about diet and nutrition,please read our Diet and Nutrition brochureavailable at www.crohnscolitisfoundation.org.Treating flaresWhat will your doctor do to treatyour flare?Often the first step is for your doctor to dosome testing to find out if your flare is due toinflammation in the intestine or something else(infection, scar tissue, medication side effect).Your doctor may recommend blood work, stooltesting, colonoscopy/upper endoscopy, or aCT scan, MRI or x-ray to find out why you havedeveloped new symptoms.Having disease flares may be a sign that achange in medication is needed. Your doctormay recommend the following: Corticosteroids, which have anti-inflammatoryproperties, can be used in the short termto get you back into remission (little to nodisease activity). Repeated and long-term useof steroids is not ideal disease management,and typically means that your current medication is not working and that a new therapyshould be tried.6
Check drug levels to see if you havedeveloped antibodies (resistance) toyour medication. Medication changes, which can includeincreasing current medication dosage,adding another medication to your regimen,or switching your medication entirely.For a current, up-to-date list of all FDAapproved medications for Crohn’s disease andulcerative colitis, please visit the Foundation’sonline IBD Medication guide:www.ibdmedicationguide.org. Additionalinformation is available in our UnderstandingIBD Medications and Side Effects brochure atwww.crohnscolitisfoundation.org.Managing flaresYou cannot completely prevent flare-ups ofCrohn’s disease or ulcerative colitis. However,in addition to taking your medications regularlyand eating a well balanced diet, the followingtips are recommended to help you manageyour disease during flares and remission: See your doctor regularly. Remember thatthe management of your disease is a partnership between yourself and your healthcareteam. Therefore, it is important to stay inclose communication with them. During timesof remission, you will probably visit your doctor every six months. During times of flares,you may visit more often. You should contactyour doctor any time you have questions orconcerns about symptoms or treatment. Follow recommended guidelines forIBD-related tests and procedures. Withproper treatment and disease monitoring,you will maximize your chances for goodhealth, decrease the likelihood of missingsigns of additional disease, and identifypossible side effects of treatment. Ask your7
doctor how often you should get IBD-relatedtests and procedures (e.g., colonoscopies,routine blood work, etc.). Monitor and track your disease. It is important to track your disease between medicalappointments so that you and your doctorcan see how IBD is impacting your life anddetermine if any changes need to be made.The Crohn’s & Colitis Foundation has a Symptom Tracker that you can find on the Foundation’s website to track your symptoms and jotdown questions for your next provider visit. Consider taking a multi-vitamin or mineralsupplement. Because Crohn’s disease andulcerative colitis can impair the body’s abilityto absorb vitamins, minerals, and other nutrients, it is important to get tested for vitaminand mineral deficiencies. As always, be sureto consult your doctor about which supplements are recommended (and safe) for youto take. Exercise. A regular exercise routine can improve overall health, and may be particularlybeneficial for people with IBD. Engaging inregular physical activity can reduce stress andmaintain and/or improve bone strength. Someresearch has also shown that exercise relievesdepression and boosts the body’s immunesystem. If having IBD limits the amount andintensity of exercise you can undertake, keepin mind that even low-intensity activities, liketaking a 30-minute walk three times a week,can produce results. Talk to your doctor todetermine an exercise program that works foryou. If your symptoms make mobility difficult,find ways to be active at home. Quit smoking. Smoking can make the symptoms of IBD worse and can make it moredifficult to treat. Reduce your stress. Stress reduction techniques can help you to stay calm and maintainperspective. There are numerous stress8
management techniques—no one method hasproven more effective than another. Each person needs to find their own healthy balance.Try an approach that appeals to you; if thatdoesn’t work, don’t despair. Try another. Hereare some frequently used techniques formanaging stress:»» Biofeedback»» Relaxation and breathing exercises»» Practicing yoga or tai chi»» Hypnotherapy»» Cognitive behavioral therapy»» Meditation»» Books, recordings, guided imagery, etc.Managing symptom discomfortWhen symptoms are flaring, you may experience a variety of uncomfortable or painfulsymptoms. Here are some tips to help youcope with the discomfort: Practice good anal hygiene by showering witha hand shower or using a perianal cleansingproduct (Balneol ).9
To reduce anal irritation, use a moisttowelette/wipe instead of bathroom tissue. Apply an all-purpose skin protectant(Vitamin A&D ointment, Desitin ) at night torelieve irritation of the skin around the anus. For anal soreness or painful bowel movementsdue to an anal fissure or fistula, bathe in warmsalt water or use a sitz bath. To help manage diarrhea, anti-diarrheal medications, such as Imodium or Pepto-Bismol ,may be effective. However, never take any ofthese drugs without consulting your healthcare provider. For joint-related discomfort, doctors mayrecommend resting the affected joint as wellas the occasional use of moist heat. Rangeof-motion exercises, as demonstrated by aphysical therapist, may also be helpful. To reduce the irritation of small mouth ulcers(also known as canker sores), medicinalmouth washes may be helpful, along witha balanced diet and a multivitamin/mineralsupplement. To help manage the symptoms of pain,experts recommend acetaminophen (Tylenol )as the safest option for IBD patients. Consultwith your healthcare provider about theappropriate pain management options. Remember to take care of yourself. Get plentyof sleep, eat well, and take time to rechargeand reduce stress when you need it.Questions for your doctorCrohn’s disease and ulcerative colitis arecomplex conditions. During a flare, you may beoverwhelmed and forget to ask critical questions of your doctor. To help you get the mostout of your doctor visit, the Crohn’s & ColitisFoundation has compiled a list of questionsyou might want to ask at the time of a flare:10
Could any condition other than my diseasebe causing my symptoms? What tests do I need to take to get to theroot of my symptoms? How often should I get these tests done?Should it be during the time of a flare-upor on a routine basis? What parts of my digestive system areaffected? How will we know if my medication needsto be adjusted? When should I expect to see results? What are the potential side effects ofthe medication? What should I do if Inotice them? What should I do if the symptoms return? If I cannot see my doctor right away, are thereany over-the-counter medication options thatcan assist with my prescribed medication?If so, which ones? What symptoms are considered anemergency? How will I know if I need a differentmedication?11
Should I change my diet or take nutritionalsupplements? If so, can my doctor recommend a dietitian or any specific nutritionalsupplements? Do I need to make any other lifestyle changes? When should I come back for a follow-upappointment?IBD flares in childrenUnderstanding and coping with IBD flares isdifficult for many adults, but it can be especiallyproblematic for children and adolescents.Parents face a challenging task when helpingtheir children come to terms with their illnessand adapt to a situation that sets them apartfrom their peers.Children and adolescents may suffer fromdepression or anxiety as a result of theirdisease. Emotional support from a counselor,psychologist, or support group may help.It is also important to advise teachers and theschool nurse about the disease, to ensure yourchild has adequate bathroom access, and thathis/her teachers and school administrators areprepared to deal with issues that arise.12
Many of the same IBD medications used inadults are used in children. But some of thesemedications have special considerations whentaken by children, mostly related to potentialside effects. Discuss all medications prescribedfor your child, including possible side effects,with your child’s physician and other healthcareproviders.Kids and teens can find information andsupport by visiting www.justlikemeIBD.organd .Coping with flaresHaving Crohn’s disease or ulcerative colitis impact much more than just your physical health- it can also have a profound impact on yourmental health and emotional wellbeing. Findingstrategies to help you cope with daily life withyour disease is essential.Difficulties may arise in your personal relationships, work, ability to travel, or sense of independence. It is not uncommon to develop strongemotions about the disease. You may be angry,fearful, uncertain, or anxious. You may wonderhow your body can betray you by making youlose control over such a basic function as abowel movement. You may feel embarrassment,or become apprehensive about leaving home.It is important not to let your fears and worriesovertake your life. There are somepractical steps you can take to ease your mind: Put together an emergency kit. This mightinclude spare underwear, an extra pair ofpants, a packet of baby wipes, toilet tissue,panty liners, and deodorizer. Even if you neverneed to use these supplies, just knowing theyare there may free your mind and allow you toengage more fully in life.13
Obtain an “I Can’t Wait” card from theCrohn’s & Colitis Foundation. This card,available with Foundation membership,may provide help when asking to use publicrestrooms. To become a member, call800-932-2423. When you leave home, plan your itineraryin advance and learn where the rest roomsare located in restaurants, shopping areas,and on public transportation. Knowing wherethe bathrooms are can ease anxiety andreduce stress. A bathroom location app onyour phone can help you find bathrooms inthe area. Be sure a trusted friend or co-worker isaware of your issues and can be called uponfor help in case of a difficult or embarrassingsituation. Symptoms of IBD may be more active atcertain times of the day. For example, youmay find that you need to stay close to a bathroom after getting up in the morning, or inthe evening after eating. Knowing when yoursymptoms are likely to occur can help youorganize your daily routines to accommodateyour bathroom needs. Fatigue can be another symptom of a flare. Itmay be manageable or it may be debilitating.Those who suffer from severe fatigue willneed to find ways to manage their energy.For example, know your limitations and takenaps when needed. If you must attend afunction, set aside time before or after theevent to rest. Your doctor may recommendspecific vitamins to help with energy. Create a support network of people whocan be called upon to help out during difficulttimes. These people should understand theserious nature of your disease and be readyto take you to the hospital or doctor if necessary. They may also be called upon to take14
care of tasks you are temporarily unable tohandle, such as childcare, grocery shopping,and others. Speak with your employer about the FamilyMedical Leave Act in the event you need totake unpaid medical leave from work or needaccommodations in the workplace. Ensure educational equity for your childby securing reasonable accommodationas needed for elementary, secondary, andpost-secondary school students. Talk to theschool’s guidance counselor and make him/her aware of your child’s needs. For information on school accommodation (504) plansvisit www.crohnscolitisfoundation.org.Talking with othersWe know that it can be difficult and even embarrassing to talk about having IBD, but sharingwhat you’re going through is important to helpyou create a support network. You may wantto consider discussing your illness with yourfriends and family, and, possibly, your workcolleagues or boss. How open you want to beand how much you want to explain is up to youand what you are comfortable with. Some sortof disclosure may make life easier, especiallyduring times when your disease flares up.15
Crohn’s disease and ulcerative colitis can takea toll, both physically and emotionally, and youwill need to attend to both. The emotionalneeds surrounding a chronic illness differ fromperson to person. Most people find it helpful tohave support from others.If you are feeling overwhelmed emotionally byyour IBD, there are mental health professionals,such as psychologists or social workers, whocan help. Feeling worried, sad, or isolated isnot uncommon in people living with a chronicillness like IBD. A mental health professionalmay help you process your emotions, gain newperspectives, and ease the social and emotional burdens of IBD.ComplicationsCertain conditions require immediate medicalattention. These include: inability to hold down liquids from nausea,vomiting, or pain rectal bleeding with clots of bloodin your stool constant pain high fever (above 100.3 F)Speak with your doctor about these conditionsso that you know what to look for and canrespond accordingly.Knowledge and supportare power!Find the answers you need to help control yourIBD by joining the Crohn’s & Colitis Foundation:16
Local Education and Support ProgramsThe Foundation has chapters across thecountry covering all 50 states. Visit our websiteat www.crohnscolitisfoundation.org to findlocal programs, support groups, and events. Power of TwoThe Foundation’s Power of Two programallows patients seeking guidance on a specificissue to speak with another peer within theIBD community who can share their experienceand provide support. To find out more, emailpowerof2@crohnscolitisfoundation.org. Irwin M. and Suzanne R. Rosenthal IBDResource Center (IBD Help Center)The IBD Help Center is a free service designedto provide you with disease-specific information, guidance, and support. Our InformationSpecialists can be reached by calling 888-MYGUT-PAIN (888-694-8872) Monday throughFriday, 9 a.m. to 5 p.m. EST, or by e-mailinginfo@crohnscolitisfoundation.org. Crohn’s & Colitis Foundation OnlineCommunityThe Foundation hosts a free websitewhere patients can get the support theyneed in managing their condition. They’llparticipate in discussion boards, share orread personal stories, and much more.The Crohn’s & Colitis Community is waitingfor people just like you. Join today atwww.crohnscolitiscommunity.org. I’ll Be DeterminedI’ll Be Determined is here to help patientsand caregivers learn more about Crohn’sdisease and ulcerative colitis, and the choicesavailable for managing them. The site offerstools and resources, perspectives from IBDpatients and experts, and a chance to connectwith others. www.ibdetermined.org.17
Camp OasisThe Crohn’s & Colitis Foundation’s Camp Oasisis a co-ed residential summer camp program.Its mission is to enrich the lives of childrenwith IBD by providing a safe and supportivecamp community. For more information, visitwww.crohnscolitisfoundation.org or call theIBD Help Center. MembershipBy joining the Crohn’s & Colitis Foundation,you’ll get:»» News, educational programs, and supportiveservices from your local chapter»» An “I can’t wait” card (may provide helpwhen asking to use a public restroom)»» A chance to contribute to research to finda cure for these challenging diseasesThe Crohn’s & Colitis Foundation sponsorsevents to increase awareness and raise fundsto find a cure for Crohn’s disease and ulcerativecolitis. Contact your local chapter or visitwww.crohnscolitisfoundation.org to find anevent nearest you.18
spin4 crohn’s & colitis curesUse your #power2cure in an exciting newway to connect with the IBD community—participate in a high-energy spin4 crohn’s &colitis cures event near you! With inspirationalinstructors and fun playlists to keep youmotivated, these indoor cycling relays are trulya #partyonabike. Teams of up to four peopleeach ride for a 30-minute session, andevery teammate receives plenty of swag!The events generate awareness of Crohn’sdisease and ulcerative colitis, and raise fundsto support groundbreaking IBD research andpatient services. Learn more at www.spin4.org. Take Steps is the Crohn’s & Colitis Foundation’s national walk program. Take Steps enables patients and families to raise money forcrucial research and to build awareness aboutCrohn’s disease and ulcerative colitis. Visitwww.cctakesteps.org for more information.19
Team ChallengeTeam Challenge is the Foundation’s endurance training and fundraising program. Withoptions including running, walking, triathlon,cycling, and hiking, there are unlimited waysto challenge yourself while raising vital fundsto cure these diseases. Each of our trainingprograms are created by expert coaches tosuit all experience levels, and you’ll be joinedby a supportive community of teammateswho share the common goal of ending Crohn’sdisease and ulcerative colitis. For moreinformation on our destination events, orto participate in your own event throughour Race In Orange program, visitwww.ccteamchallenge.org.20
About the Crohn’s &Colitis FoundationEstablished in 1967, the Crohn’s & Colitis Foundation is the leading non-profit organizationfocused on both research and patient supportfor inflammatory bowel diseases (IBD). TheFoundation’s mission is to cure Crohn’s diseaseand ulcerative colitis, and to improve the qualityof life for the estimated 3 million Americansliving with IBD.For over 50 years, we have been inspiring andengaging patients and caregivers in the country’s largest IBD community, and helping todramatically accelerate the pace of researchby breaking down traditional barriers topatients, data, funding, and collaborations. Wealso provide extensive educational resourcesfor patients and their families, medical professionals, and the public.We can help! Contact us ts:Reviewers:Sushila Dalal, MD, Karen Edelblum, PhD,Rajesh Shah, MD, Sasha Taleban, MD,and Raluca Vrabie, MD.Contributors:Pamela Bergantino, Theresa McQuillanDeCrescenzo, Carolyn Grazinger, Julie Merritt,and Heidi YorkDesign & Layout:Rubicon Design Associates
This educational brochure is supported bya medical education grant from TakedaPharmaceuticals U.S.A, Inc. Additional supportis provided through the Crohn’s & Colitis Foundation’s annual giving program and donors.733 Third AvenueSuite 510New York, NY e Crohn’s & Colitis Foundation is a nonprofit organizationthat relies on the generosity of private contributions toadvance its mission to cure Crohn’s disease and ulcerativecolitis, and to improve the quality of life of children andadults affected by these diseases.6/2019
taking a 30-minute walk three times a week, can produce results. Talk to your doctor to determine an exercise program that works for you. If your symptoms make mobility difficult, find ways to be active at home. Quit smoking. Smoking can make the symp-toms of IBD worse and c