Transcription
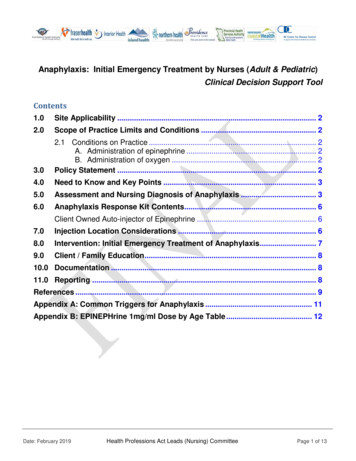
Anaphylaxis: Initial Emergency Treatment by Nurses (Adult & Pediatric)Clinical Decision Support ToolContents1.0Site Applicability . 22.0Scope of Practice Limits and Conditions . 23.02.1 Conditions on Practice . 2A. Administration of epinephrine . 2B. Administration of oxygen . 2Policy Statement . 24.0Need to Know and Key Points . 35.0Assessment and Nursing Diagnosis of Anaphylaxis . 36.0Anaphylaxis Response Kit Contents. 6Client Owned Auto-injector of Epinephrine . 67.0Injection Location Considerations . 68.0Intervention: Initial Emergency Treatment of Anaphylaxis . 79.0Client / Family Education . 810.0 Documentation . 811.0 Reporting . 8References . 9Appendix A: Common Triggers for Anaphylaxis . 11Appendix B: EPINEPHrine 1mg/ml Dose by Age Table . 12Date: February 2019Health Professions Act Leads (Nursing) CommitteePage 1 of 13
1.0 Site ApplicabilityIf anaphylaxis is suspected, based upon clinical presentation and possible exposure to atrigger, treatment should be provided as outlined in this document.All Acute, Community, Long Term Care sites and non-hospital settingsException: when an alternate practice standard/procedure, clinical decision support tool ormedical order is in effect for initial emergency treatment of anaphylaxis.Note: All nurses (RN, RPN and LPN) who immunize without an order must follow theDecision Support Tools (DST) – BC Communicable Disease Control Manual, Chapter 2:Immunization; Part 3 Management of Anaphylaxis in a Non-Hospital Setting established bythe BC Centre for Disease Control (BCCDC). The clinical direction in both of these documentsis identical.In this document client refers to patient, client or resident.2.0 Scope of Practice Limits and ConditionsThis decision support tool is intended for use by nurses.Following an assessment and nursing diagnosis of anaphylaxis, Registered Nurses (RN),Registered Psychiatric Nurses (RPN) and Licensed Practical Nurses (LPN) may carry out theinitial emergency management of anaphylaxis: regardless of the causative agent;without an order;across all healthcare settings (i.e. hospital and non-hospital)2.1 Conditions on PracticeA. Administration of epinephrinePrior to administering epinephrine for the emergency management of anaphylaxis:1) RN, RPN and LPN must follow this decision support tool.2) RPN and LPN must successfully complete additional education [AnaphylaxisInitial Emergency Treatment by Nurses (Adult & Pediatric). Available onLearning Hub]This education is recommended for RNs.B. Administration of oxygenHealth Authority/employer practice limits may apply.If available in the practice setting, prior to initiating oxygen therapy:1) LPNs must follow a decision support tool and complete additional education.3.0 Policy StatementClients who have been treated for anaphylaxis must have immediate follow up by a physicianor Nurse Practitioner.In the community, long term care and ambulatory settings, clients who have been treated foranaphylaxis must be transferred to hospital via ambulance.Date: February 2019Health Professions Act Leads (Nursing) CommitteePage 2 of 13
4.0 Need to Know and Key PointsAnaphylaxis occurs with exposure to a trigger (see Appendix A) in a susceptible individual.Onset of symptoms usually occurs in minutes but can occur hours after exposure to a trigger.Death from anaphylaxis may occur as a result of severe respiratory complications,cardiovascular collapse, or both.Early administration of intramuscular (IM) Epinephrine is first line treatment foranaphylaxis to prevent death and there is no known equivalent substitute.There is no contra-indication to epinephrine administration in anaphylaxis.Epinephrine: Acts on smooth muscle of the bronchial tree reducing bronchospasmCounteracts histamine-induced vasodilationIncreases cardiac outputReduces histamine releaseNote: Diphenhydramine (Benadryl) is NOT INDICATED in anaphylaxis.Antihistamines are not indicated as initial first line treatment in the emergency management ofanaphylaxis as there is no effect on respiratory or cardiovascular symptoms and they are oflittle clinical importance in life-threatening anaphylaxis based on current evidence.H1 antihistamines (e.g. Benadryl) relieve localized and less severe systemic allergic reactionsand the only useful clinical effect is the improvement of itch and hives.4, 13, 145.0 Assessment and Nursing Diagnosis of AnaphylaxisEarly recognition of anaphylaxis is essential to ensure timely intervention.Assess the client for signs and symptoms of anaphylaxis. These generally involve two or morebody systems. See Table 1 for clinical scenarios and body systems involved.IMPORTANT: Anaphylaxis can occur without presence of hives.Table 1: Clinical Scenarios and Body Systems Involved with Anaphylaxis.ClinicalScenarioSIGNS &SYMPTOMSOnsetMinutes toHours(1) No Clear Trigger(2) Suspected Trigger(new food, drug orimmunization) Skin/mucosal orboth Plus at least one ofthe following: RespiratoryCompromise Reduced BloodPressure orAssociatedSymptomsTWO OR MORE of thefollowing: Skin/mucosal RespiratoryCompromise Reduced BloodPressure or AssociatedS/S Persistent GI(3) Accidental Exposure toKnown Allergen(Same as column 2 or BP)REDUCED BLOODPRESSURE ONLY Child – Low Systolic ordecrease greater than 30% Adult – Systolic 90 ordecrease greater than 30%from baselineRefer to Image 1: World Allergy Organization Anaphylaxis Guideline Poster on page 4 of this document for adetailed description of signs and symptoms to inform the assessment and nursing diagnosis of anaphylaxis.Date: February 2019Health Professions Act Leads (Nursing) CommitteePage 3 of 13
Image 1: World Allergy Organization Anaphylaxis Guideline Poster(Adapted from Canadian Pediatric Society, 2018)Anaphylaxis must be distinguished from fainting (vasovagal syncope) and anxiety (panicattack). See Table 2: Signs and Symptoms of Anaphylaxis versus Fainting and Anxiety.Date: February 2019Health Professions Act Leads (Nursing) CommitteePage 4 of 13
Table 2: Signs and Symptoms of Anaphylaxis versus Fainting and iratoryCardiovascularGastrointestinalOtherDate: February 2019FaintingAnxietyA potentially life threatening allergicreaction that is rapid in onset andprogression of symptoms.Temporary unconsciousness Protective physiological statecaused by diminished bloodrecognized as fear,supply to the brain due toapprehension, or worrypainful stimuli or emotionalreaction. rapid onset and progression of sudden onset sudden onsetsymptoms occurs before, during or occurs before, during, or occurs minutes to hours aftershortly after trigger (e.g.shortly after trigger (e.g.exposure to triggersight of the needle)sight of the needle) recovery dependent on response recovery occurs within 1-2 recovery generally occursto treatmentminuteswithin 1-2 minutes localized subcutaneous (or sub pale palemucosal) swelling and tingling to excessive perspiration excessive perspirationface and mouth cold, clammy cold, clammy hives – may be delayed warm, itchy, red and blotchy labored breathing - hoarse voice, breathing normal or breathing rapid andthroat tightness, rapid breathing,shallow, irregular andshallow (hyperventilation)wheezing, coughing, nasallabored breath-holding inflaring, nasal and chestchildrencongestion rhinitis (stuffy or runny nose,itchy watery eyes and sneezing) shortness of breath, stridor,retractions, chest pain andcyanosis weak and rapid pulse slow, steady pulse rapid pulse hypotension alone after an decreased systolic and normal or elevatedexposure can representdiastolicsystolicanaphylaxis hypotension is less commonin children shock nausea, vomiting, diarrhea nausea nausea abdominal pain or cramping dysphagia (difficulty swallowing) drooling in children anxious or feeling of “impending fearfulness fearfulnessdoom” light-headedness light-headedness sudden lack of energy dizziness dizziness(lethargy) in children numbness, weakness numbness, weakness quietness or sleepiness in sometimes accompanied tingling around lips andchildrenby brief clonic seizurespasm in the hands and headache, light-headedness oractivityfeet associated withdizzinesshyperventilation decreased level ofconsciousness uterine crampsNOTE: Bolded text indicates symptoms specific to pediatric clients.Health Professions Act Leads (Nursing) CommitteePage 5 of 13
6.0 Anaphylaxis Response Kit Contents Copy of this Decision Support Tool 4 ampoules of EPINEPHrine 1mg/mL 4 – 1 mL syringes Needles (25 to 27 gauge)o4 - 1 incho4 - 1½ inch Alcohol swabsCheck medication vials and equipment. Replace if outdated.Client Owned Auto-injector of EpinephrineA client’s own auto-injector of epinephrine may be used to administer epinephrine in situationswhere a delay in administration of epinephrine may occur (e.g. kit not readily available).Clinical judgement is required.Note: EpiPen delivers 0.3 mg of epinephrine and EpiPen Junior delivers 0.15 mg ofepinephrine.7.0 Injection Location ConsiderationsThe correct site of intramuscular (IM) administration of epinephrine is ALWAYS the vastuslateralis located at the middle third of the lateral thigh [See image 1].Image 1: Vastus Lateralis Injection SiteNotes: If immunization/medication has been administered to both legs, give epinephrine IM at least2.5 cm (1 inch) from original injection site. Administration of epinephrine through the clothing is acceptable in emergency situations.Date: February 2019Health Professions Act Leads (Nursing) CommitteePage 6 of 13
8.0Intervention: Initial Emergency Treatment of AnaphylaxisASSESS client for signs & symptoms of anaphylaxisCirculation, Airway, Breathing (CAB) Skin, Mental Status and GIRemove/Stop the offending agent/drug (if possible)Adults (14 years and older)0.5 mg (of 1 mg/mL)IM vastus lateralisChildren under 14 years0.01 mg/kg (of 1mg/mL) to max 0.5 mg/doseIM vastus lateralis See Appendix A for dose by ageCALL Code Blue or 911RE-ASSESS CABPlace in Recumbent Position / Elevate Legs (if possible)Perform SimultaneouslyADMINISTEREPINEPHrine Intramuscular (IM) OnlyADMINISTER Oxygen for Hypoxia (If available)Goal: SpO2 above 92%CONTINUOUS OBSERVATIONVITAL SIGNS Q5 Minutes until Transfer of CareREPEAT EPINEPHrine (IM) Q5 Minutes PRN x 2 dosesfor ongoing signs and symptoms of anaphylaxis(to a maximum of 3 total doses)Adults (14 years and older)0.5 mg (of 1 mg/mL)IM vastus lateralisChildren under 14 years0.01 mg/kg (of 1mg/mL) to max 0.5 mg/doseIM vastus lateralis See Appendix B for dose by ageINITIATE IV Access (if possible)DO NOT ADMINISTER EPINEPHrine via IV RouteDOCUMENT & PROVIDE HANDOVER to CODE TEAM or PARAMEDICS Time of onset and nature of symptomsInterventions provided including timing and amount of epinephrineResponse to treatmentDate: February 2019Health Professions Act Leads (Nursing) CommitteePage 7 of 13
9.0Client / Family EducationClients who have experienced anaphylaxis and their families should receive educationincluding: Information on anaphylaxis being a potentially life threatening allergic reaction Avoiding triggers The emergency steps to take in case of anaphylaxis: Carry your prescribed epinephrine auto-injector Administer prescribed epinephrine auto-injector immediately If in a hospital, long term care home or other institution: summon help If in the community, or at home: call an ambulance Follow up with your physician, nurse practitioner, allergist or other appropriate resource to: Develop an anaphylaxis action plan including self-administration of epinephrine Obtain medical identification (e.g. MedicAlert ) Undergo testing to confirm triggers Explore ways that sensitivities to triggers may be reducedSuggested client teaching resources: Health Link BC. (2018) Severe Allergic Reaction (Anaphylaxis) Food Allergy Canada. (2017) Allergic Reactions Could You Save a Life10.0 Documentation Document the following in the health record: Assessment Nursing diagnosis of the condition Interventions carried out Client’s response Follow-up actions, transfer of care and client teachingEnter client allergy status as per employer policies to ensure communication to otherproviders.11.0 ReportingSuspected anaphylaxis adverse reactions related to drug or immunization administration arereported as required by employer policy: Patient Safety Learning System (PSLS) or equivalent (as required) Long Term Care settings must report adverse event to licensing body (as required) If the trigger for anaphylaxis is the result of an immunization, complete the following:Date: February 2019 BCCDC Worksheet for Events Managed as Anaphylaxis Following Immunization BCCDC Adverse Event Following Immunization (AEFI) Case Report FormHealth Professions Act Leads (Nursing) CommitteePage 8 of 13
References1. Simons, F.E. et al. (2011). World Allergy Organization guidelines for the assessment andmanagement of anaphylaxis. World Allergy Organization Journal. 4:13-37. Retrievedfrom http://www.waojournal.org/content/4/2/132. Simons, F.E. et al. (2015). 2015 Update of the evidence base: World Allergy Organizationanaphylaxis guidelines. World Allergy Organization Journal. 8:32. Retrieved 10.1186/s40413-015-0080-13. Campbell, R.L., Kelso, J.M. Anaphylaxis: acute diagnosis. UpToDate. Retrieved April 19th,2017 from ediagnosis?source see link4. Campbell, R.L., Kelso, J.M. Anaphylaxis: emergency treatment. UptoDate. Retrieved June 8,2018 from gencytreatment?source search result&search anaphylaxis&selectedTitle 2 1505. BC Centre for Disease Control. (2013). Section V – Management of Anaphylaxis in a NonHospital Setting. Communicable Disease Control Immunization Program. Vancouver:BC Centre for Disease Control. Retrieved from id/CD%20Manual/Chapter%202%20-%20Imms/SectionV Anaphylaxis.pdf6. Canadian Society of Allergy and Clinical Immunology. (2016). Anaphylaxis in Schools andOther Settings 3rd Edition Revised. Canadian Society of Allergy and Clinical Immunology.Retrieved from xis-3rd-editionrevised.pdf7. College of Registered Nurses of British Columbia. (2017). Scope of Practice for RegisteredNurses. Vancouver: College of Registered Nurses of British Columbia. Retrieved esources/433ScopeforRegisteredNurses.pdf8. College of Registered Psychiatric Nurses of British Columbia. (2017). Scope of Practice forRegistered Psychiatric Nurses: Standards, Limits and Conditions. Vancouver: College ofRegistered Psychiatric Nurses of British Columbia. Retrieved Feb-13-2017.pdf?v 4109. College of Licensed Practical Nurses of British Columbia. (2017). Scope of Practice forLicensed Practical Nurses. Vancouver: College of Licensed Practical Nurses of BritishColumbia. Retrieved from ocuments/Scope-of-Practice-ONLINE.aspx10. Health Canada. (2016). Food Allergies: Information for Consumers. Retrieved -aa/index-eng.php11. Epinephrine. (n.d.). In Lexicomp. Retrieved from https://online.lexi.com/lco/action/home12. Muraro, A. et al. (2014). Anaphylaxis: guidelines from the European Academy of Allery andClinical Immunology. Allergy. 29: 1026-1045. Retrieved .12437/fullDate: February 2019Health Professions Act Leads (Nursing) CommitteePage 9 of 13
13. Sheikh, A., Broek, V.T., Brown, S.G.A. and Simons, F.E.R. (2007). H1‐antihistamines for thetreatment of anaphylaxis: Cochrane systematic review. retrieved on June 8, 2018 11/j.1398-9995.2007.01435.x14. Australasian Society of Clinical Immunology and Allergy (2017). Acute management ofanaphylaxis. Retrieved on June 8, 2018 apers/ASCIA Guidelines Acute Management Anaphylaxis 2017 Updated.pdf15. Medication Administration: Subcutaneous Injection. (2017, November). In Elsevier clinicalskills. Retrieved Personalization/Home?VirtualName interiorhealth-canada16. Medication Administration: Intramuscular Injection. (2018, May). In Elsevier clinical skills.Retrieved Personalization/Home?VirtualName interiorhealth-canada17. Canadian Pediatric Society. (2018) Position statement Emergency treatment of anaphylaxis ininfants and children. Retrieved August 15, 2018 ency-treatment-anaphylaxisDate: February 2019Health Professions Act Leads (Nursing) CommitteePage 10 of 13
Appendix A: Common Triggers for AnaphylaxisThe true global rate of occurrence of anaphylaxis from all triggers in the general population isunknown because of under-recognition by patients and caregivers and under-diagnosis byhealthcare professionals.1Numerous nursing and health care activities expose patients to common triggers for anaphylaxis.Below are some selected common triggers for anaphylaxis. Triggers for individuals can varywidely and the below list is not exhaustive.FoodEnvironmentMedications / Other Peanuts Tree nuts Soy Horse Non-steroidal anti-inflammatories (including ASA) Seafood Latex Biologic medications including immunizations Shellfish Chemotherapy Milk Radiocontrast media (x-ray dye) Eggs Dextrans Mustard Substances found in illicit drugs Wheat Blood and Blood Products Sesame Latex GlovesDate: February 2019Venom fromstinging insectsAntibiotics especially β lactams (includingpenicillins, cephalosporins, carbapenems)Health Professions Act Leads (Nursing) CommitteePage 11 of 13
Appendix B: EPINEPHrine 1mg/ml Dose by Age TableNOTE:Use dose by weight whenever possible.Dose by Age(Dosing is 0.01 mg/kg to maximum of 0.5 mg)AgeDose in mgVolume (1 mg/mL)2-6 months0.07 mg0.07 mL7-12 months0.1 mg0.1 mL13 months - 4 years0.15 mg0.15 mL5 years0.2 mg0.2 mL6-9 years0.3 mg0.3 mL10-13 years0.4 mg0.4 mLGreater than or equal to 14 years0.5 mg0.5 mLDate: February 2019Health Professions Act Leads (Nursing) CommitteePage 12 of 13
Adapted from:Vancouver Coastal Health & Providence Health Care Professional Practice. (September 2017) Anaphylaxis:Initial Emergency Treatment Decision Support Tool. (Draft)Developed by:Paula Araujo, Regional Practice Leader, Clinical Process, Interior HealthCathy Czechmeister, Lead, Professional Practice Strategy - Nursing, Northern HealthSheila Gordon-Payne, Lead, Professional Practice Strategy – Nursing, Northern HealthMelina Kason, Practice Consultant, Professional Practice, Island HealthReviewed by:Dr. Monika Naus MD FRCPC, Medical Director, Communicable Diseases and Immunization Service, BC Centrefor Disease ControlDr. Scott B. Cameron MD, PhD, FRCPC, Clinical Instructor, Division of Allergy & Immunology, Department ofPediatrics, University of British ColumbiaChristine Halpert, Senior Practice Leader, Communicable Diseases and Immunization Service, BC Centre forDisease ControlStephanie Meier, Public Health Resource Nurse, Communicable Diseases and Immunization Service, BCCentre for Disease ControlBC Provincial Health Authorities Representatives from Fraser Health, Interior Health, Vancouver Coastal Health,Provincial Health Services Authority, Providence HealthEndorsed by:British Columbia Chief Nursing Officer CouncilDate: February 2019Health Professions Act Leads (Nursing) CommitteePage 13 of 13
Antihistamines are not indicated as initial first line treatment in the emergency management of anaphylaxis as there is no effect on respiratory or cardiovascular symptoms and they are of little clinical importance i