Transcription
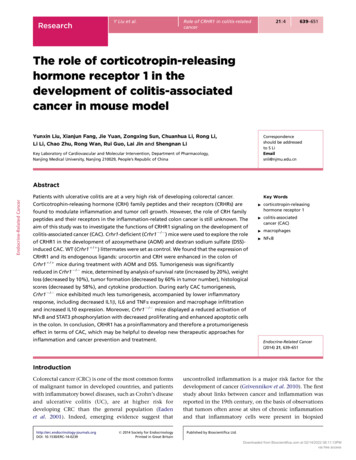
ResearchY Liu et al.Role of CRHR1 in colitis-relatedcancer21:4639–651The role of corticotropin-releasinghormone receptor 1 in thedevelopment of colitis-associatedcancer in mouse modelYunxin Liu, Xianjun Fang, Jie Yuan, Zongxing Sun, Chuanhua Li, Rong Li,Li Li, Chao Zhu, Rong Wan, Rui Guo, Lai Jin and Shengnan LiCorrespondenceshould be addressedto S LiEmailsnli@njmu.edu.cnKey Laboratory of Cardiovascular and Molecular Intervention, Department of Pharmacology,Nanjing Medical University, Nanjing 210029, People’s Republic of ChinaEndocrine-Related CancerAbstractPatients with ulcerative colitis are at a very high risk of developing colorectal cancer.Corticotrophin-releasing hormone (CRH) family peptides and their receptors (CRHRs) arefound to modulate inflammation and tumor cell growth. However, the role of CRH familypeptides and their receptors in the inflammation-related colon cancer is still unknown. Theaim of this study was to investigate the functions of CRHR1 signaling on the development ofcolitis-associated cancer (CAC). Crhr1-deficient (Crhr1K/K) mice were used to explore the roleof CRHR1 in the development of azoxymethane (AOM) and dextran sodium sulfate (DSS)induced CAC. WT (Crhr1C/C) littermates were set as control. We found that the expression ofCRHR1 and its endogenous ligands: urocortin and CRH were enhanced in the colon ofCrhr1C/C mice during treatment with AOM and DSS. Tumorigenesis was significantlyreduced in Crhr1K/K mice, determined by analysis of survival rate (increased by 20%), weightloss (decreased by 10%), tumor formation (decreased by 60% in tumor number), histologicalscores (decreased by 58%), and cytokine production. During early CAC tumorigenesis,Crhr1K/K mice exhibited much less tumorigenesis, accompanied by lower inflammatoryresponse, including decreased IL1b, IL6 and TNFa expression and macrophage infiltrationand increased IL10 expression. Moreover, Crhr1K/K mice displayed a reduced activation ofNFkB and STAT3 phosphorylation with decreased proliferating and enhanced apoptotic cellsin the colon. In conclusion, CRHR1 has a proinflammatory and therefore a protumorigenesiseffect in terms of CAC, which may be helpful to develop new therapeutic approaches forinflammation and cancer prevention and treatment.Key Words"corticotropin-releasinghormone receptor 1"colitis-associatedcancer (CAC)"macrophages"NFkBEndocrine-Related Cancer(2014) 21, 639–651IntroductionColorectal cancer (CRC) is one of the most common formsof malignant tumor in developed countries, and patientswith inflammatory bowel diseases, such as Crohn’s diseaseand ulcerative colitis (UC), are at higher risk fordeveloping CRC than the general population (Eadenet al. 2001). Indeed, emerging evidence suggest thathttp://erc.endocrinology-journals.orgDOI: 10.1530/ERC-14-0239q 2014 Society for EndocrinologyPrinted in Great Britainuncontrolled inflammation is a major risk factor for thedevelopment of cancer (Grivennikov et al. 2010). The firststudy about links between cancer and inflammation wasreported in the 19th century, on the basis of observationsthat tumors often arose at sites of chronic inflammationand that inflammatory cells were present in biopsiedPublished by Bioscientifica Ltd.Downloaded from Bioscientifica.com at 02/14/2022 08:11:13PMvia free access
Endocrine-Related CancerResearchY Liu et al.samples from tumors (Balkwill & Mantovani 2001). It isnow evident that inflammatory cells have powerfuleffects on tumor development. Early in the neoplasticprocess, cells such as neutrophils, macrophages, andlymphocytes are powerful tumor promoters, producingan attractive environment for tumor growth, facilitatinggenomic instability and promoting angiogenesis. Theinflammatory cells along with the chemokines andcytokines produced could regulate the growth, migration,and differentiation of all cell types and finally influencethe whole tumor organ (Shacter & Weitzman 2002, Karinet al. 2006, Lin & Karin 2007).Particular emphasis has been given on the roles ofthe master transcription factors such as nuclear factorkappa-light-chain-enhancer of activated B cells (NFkB)and STAT3 in the development of colitis-associated cancer(CAC). In immune cells, NFkB induces the transcriptionof genes that encode proinflammatory cytokines, whichcan act in a paracrine manner on mucosal epithelialcells (Greten et al. 2004). What is more, in tumorigeniccells, both NFkB and STAT3 control apoptosis and STAT3can also enhance proliferation (Grivennikov et al. 2009,Pickert et al. 2009). Another key player in apoptosis is theBCL2 family of proteins, which can be divided into eitheranti-apoptotic members (BCL2, BCL-XL, BCL-W, A1, andMCL1) or pro-apoptotic members (BAX, BID, BAD, BAK,BIC, BOK, BCL-XS, and HRK) members (Reed 1996, Grosset al. 1999). Many studies proposed that the relative levelsof the pro-apoptotic protein BAX and anti-apoptoticprotein BCL2 within a cell determine whether the celllives or dies in response to apoptotic signaling (Oltvai et al.1993, Reed 1994).Corticotrophin-releasing hormone (CRH) familyneuropeptides perform many physiological and pathophysiological functions. This family consists of CRH andCRH-related peptides, urocortin (UCN1), UCN2 (stresscopin-related peptide), and UCN3 (stress-copin) (Vaughanet al. 1995). They develop their biological activitiesthrough two G-protein-coupled receptors, CRH receptor1 (CRHR1) and CRH receptor 2 (CRHR2). CRH and UCN1have a high affinity to CRHR1, whereas UCN2 and UCN3exclusively bind to CRHR2 (Vaughan et al. 1995). BothCRHRs and their ligands distribute extensively in the CNS(Van Pett et al. 2000) and the periphery site includingimmune tissues and inflammatory sites (Radulovic et al.1999). In the CNS, CRH modulates the synthesis andrelease of adrenocorticotropic hormone, which in turnstimulates the production of glucocorticoids, exertinganti-inflammatory effects (Bateman et al. 1989). However,recent findings have revealed that large quantities ofhttp://erc.endocrinology-journals.orgDOI: 10.1530/ERC-14-0239q 2014 Society for EndocrinologyPrinted in Great BritainRole of CRHR1 in colitis-relatedcancer21:4640peripheral CRH-related peptides function as proinflammatory factors (Webster et al. 1998, Elenkov & Chrousos1999, Zhu et al. 2011). Our previous data also demonstrated that UCN1 could increase lipopolysaccharide(LPS)-induced endothelial permeability by disrupting theVE-cadherin–b-catenin complex (Wan et al. 2013). Besides,UCN1 was found to increase pulmonary vascular permeability via mast cell infiltration and activation (Wuet al. 2006), and that mast cell activation and degranulation induced by UCN1 was mediated by increasingintracellular calcium concentration, which could beblocked by a selective CRHR1 antagonist (Wu et al.2008). These proinflammatory actions of CRH familyand its receptors are involved in a series of inflammatorydiseases, including rheumatoid arthritis (Kohno et al.2001), Hashimoto’s thyroiditis (Scopa et al. 1994), and UC.Early in 1990s, the CRH family and the receptors werefound in the gastrointestinal system and were reportedto be implicated in the actions of colitis (van Tol et al. 1996).In 1995, it was proved that CRH was present in the colonicmucosa of patients with UC and acted as a proinflammatory agent modulating the intestinal immune system(Kawahito et al. 1995). Furthermore, UCN1 was found tobe synthesized and secreted in plasma cells, which wascorrelated with the severity of inflammation in colonicmucosa with UC (Saruta et al. 2004). In addition, in themouse model of DSS-induced colitis, CRHR1 deficiency wasobserved to contribute to the relief of intestinal inflammation (Im et al. 2010). Taken together, these studiessuggest that activation of CRHR1 by CRH or UCN1 exertsan effect of exacerbating intestinal inflammation. However, none of these earlier studies examined the detailedeffects of CRHR1 on colitis-associated tumorigenesis.In this study, we sought to investigate the role ofCRHR1 in the regulation of tumorigenesis in a mousemodel of CAC.Materials and methodsHuman colorectal tissue specimensHuman colon samples were obtained from subjectsenrolled in the First Affiliated Hospital of Nanjing MedicalUniversity (Nanjing, China). Colon mucosal biopsieswere collected at the time of colonoscopy and storedin formalin. Matched mucosal biopsies were obtainedand sent to the pathology department for routinehistological evaluation. Histological examination from atotal of seven subjects diagnosed with colorectal carcinoma were analyzed.Published by Bioscientifica Ltd.Downloaded from Bioscientifica.com at 02/14/2022 08:11:13PMvia free access
Y Liu et al.ResearchRole of CRHR1 in colitis-relatedcancerAnimal modelsABDay05 1045 5025 30AOM 3% DSS H2O 3% DSS H2O 3% DSS80H2OmRNA/β-actinEndocrine-Related CancerCrhr1 heterozygote (Crhr1C/K) mice (129-Crhrtm1Klee) werepurchased from The Jackson Laboratory (Bar Harbor, ME,USA) and their genetic background is 129S4/SvJae andC57BL/6. Crhr1-deficient (Crhr1K/K) mice and their WT(Crhr1C/C) littermates (M and F, 8–12 weeks) wereobtained from heterozygous breedings. All mice werehoused under controlled conditions (temperature 22 8C;12 h light:12 h darkness cycle; lights on at 0700 h) andwere given free access to standard laboratory pelletformula and tap water. Crhr1C/C and Crhr1K/K micewere used for experiments while Crhr1K/C were used forfurther production and excessive mice were discarded. Allexperiments were carried out in accordance with theofficial recommendations of the Chinese CommunityGuidelines. CAC was induced as described previously(Greten et al. 2004). Briefly, mice were injected i.p. with10 mg/kg azoxymethane (AOM; Sigma) on day 0 and after5 days, received drinking water containing 3% dextransodium sulfate (DSS; MP Biomedicals, Irvine, CA, USA)1008021:4641for 5 days followed by regular water drinking for 14 days.This cycle was repeated twice and mice were killed on the80th day (Fig. 1A).Histopathological analysisFormalin-preserved colon sections were processed andembedded in paraffin by standard techniques. Longitudinal sections of 5 mm thick were stained with hematoxylinand eosin (H&E) and examined by a pathologist blindedto the experimental groups. Colitis scores were assignedbased on the extent and severity of inflammation,ulceration, and hyperplasia of the mucosa, as describedby Zaki et al. (2011). For immunohistochemistry, formalin-fixed paraffin-embedded tissues were cut into 4 mmsections and slides were stained with antibodies againstthe CRH (Sigma), UCN1 (Abcam, Cambridge, MA, USA),CRHR1 (Novus Biologicals, Cambridge, MA, USA), macrophage marker F4/80 (Abcam), B cell marker CD20(Abcam), and T cell marker CD3 (Abcam).******CControlCACControlCAC**6040CRHR150 kDa20Actin43 0 CRH400 400 Ucn1CRHR1400 Figure 1Expression of CRHR1 and its ligands increased in the mice with colitisrelated cancer induced by AOM and DSS. (A) Schematic overview of theCAC regimen. Crhr1C/C littermates were injected with AOM followed bythree cycles of 3% DSS in drinking water. Colons were analyzed on day 80.(B) Real-time PCR analysis for mRNA of urocortin (Ucn1), corticotrophinreleasing hormone (CRH), and CRH receptor 1 (CRHR1) in colon from CACmice and Crhr1C/C littermate (nZ8 mice per group). (C) Western blottinghttp://erc.endocrinology-journals.orgDOI: 10.1530/ERC-14-0239q 2014 Society for EndocrinologyPrinted in Great Britainanalysis for CRHR1 protein in colons from CAC and control mice (nZ8 miceper group). (D) Expressions of CRHR1 were determined by immunohistochemistry from the colon samples of CAC patients. (E) Expressions andlocalizations of UCN1, CRH, and CRHR1 were determined by immunohistochemistry from CAC and control mice. Data represented meansGS.E.M.;**P!0.01, ***P!0.001 vs Crhr1C/C.Published by Bioscientifica Ltd.Downloaded from Bioscientifica.com at 02/14/2022 08:11:13PMvia free access
Endocrine-Related CancerResearchY Liu et al.Role of CRHR1 in colitis-relatedcancer21:4642Quantitative real-time PCRPBMC isolationTotal RNA from the mouse colon was isolated using TRIzol(Invitrogen) according to the manufacturer’s protocol,and an equal amount of RNA (2 mg) was transcribed intocDNA using an RT reagent kit (iTaq, Hercules, CA, USA).Subsequently, quantitative real-time PCR was carried outwith SYBR Green oligonucleotides (iTaq) using a 7300Fast Real-Time PCR instrument (Applied Biosystems).The level of expression was calculated based on the PCRcycle number (CT) at which the exponential growth influorescence from the probe passed a certain thresholdvalue (CT). Relative gene expression was determined bydifferences in the CT values of the target genes afternormalization to the RNA input level, using the CT valueof ACTIN. Relative quantification was represented bystandard 2KDCT calculations. DCTZ(CT-target geneKCT-ACTIN).Each reaction was carried out in triplicate. Primersequences are given in Table 1.Mice were anesthetized in a diethyl ether atmosphere andblood was collected by cardiac paracentesis in a tubecontaining EDTA-2K buffer. Anti-coagulated blood waslayered onto mononuclear separating medium (Haoyang,Tianjin, China) and peripheral blood mononuclear cells(PBMC) were purified by gradient centrifugation (400 g,30 min) according to the manufacturer’s recommendations.Cell amount analysisBriefly, blood was sampled from retroorbital sinus in a tubecontaining EDTA-2K buffer, and stained for macrophagocyte cell markers CD11bC and CD11cK (e-Bioscience,San Diego, CA, USA) and then analyzed with flowcytometry (BD Biosciences, Franklin Lakes, NJ, USA).Table 1Immunoblotting analysisEqual amounts of protein from colon were subjected toSDS–PAGE analysis and immunoblotting using antiCRHR1 antibody (1:1000, overnight in 4 8C; NovusBiologicals), anti-p-NFkB antibody (1:1000, overnight in4 8C; Cell Signaling Technology, Danvers, MA, USA), antiNFkB antibody (1:1000, overnight in 4 8C; Cell SignalingTechnology), anti-p-STAT3 antibody (1:1000, overnight in4 8C; SAB), anti-STAT3 antibody (1:1000, overnight in4 8C; Cell Signaling Technology), anti-BCL2 antibody(1:1000, overnight in 4 8C; Cell Signaling Technology),anti-BAX antibody (1:1000, overnight in 4 8C; Abcam),anti-b-ACTIN antibody (1:5000, overnight in 4 8C, SAB),and anti-histone antibody (1:10 000, overnight in 4 8C;Abmart, Shanghai, China). Western blotting analysis wascarried out as described previously (Xu et al. 2009).Summary of qRT-PCR of primer sequencesNameSequencesGenBank accession numberCRHR1Sense: GGAACCTCATCTCGGCTTTCAAntisense: GTTACGTGGAAGTAGTTGTAGGCSense: TCTTGCTGTTAGCGGAGCGAntisense: TCGAATATGATGCGGTTCTGCSense: CCTCAGCCGGTTCTGATCCAntisense: GCGGAAAAAGTTAGCCGCAGSense: TGACCTGGGCTGTCCTGATGAntisense: GGTGCTCATGTCCTCATCCTGSense: CTGCAAGAGACTTCCATCCAGTTAntisense: GAAGTAGGGAAGGCCGTGGSense: GCTCTTACTGACTGGCATGAGAntisense: CGCAGCTCTAGGAGCATGTGSense: AGGCTGCCCCGACTACGTAntisense: GACTTTCTCCTGGTATGAGATAGCAAASense: GGGTGTCCCTTCACTTCTTTCAAntisense: TGGGAGGCACTTGCATTGASense: AAGCGTCATTGAATCACACCTGAntisense: TGACCTCAAACTTGGCAATACTCSense: ATGCTCCCCGGGCTGTATAntisense: CATAGGAGTCCTTCTGACCCATTCNM 007762.4UrocortinCRHIL1bIL6IL10TNFaCOX2IFNgACTINNM 021290.2NM 205769.2NM 008361.3NM 031168.1NM 010548.2NM 001278601.1NM 011198.3NM 008337.3NM 007393.3CRH, corticotropin-releasing hormone; CRHR, CRH receptor; TNFa, tumor necrosis factor alpha; IL, interleukin; IFNg, interferon gamma; COX2,cycloxygenase 2.http://erc.endocrinology-journals.orgDOI: 10.1530/ERC-14-0239q 2014 Society for EndocrinologyPrinted in Great BritainPublished by Bioscientifica Ltd.Downloaded from Bioscientifica.com at 02/14/2022 08:11:13PMvia free access
ResearchY Liu et al.In situ intestinal proliferation assayThe number of proliferating cells in intestinal epitheliumwas determined using the immunoperoxidase stainingprotocol with the thymidine analog 5-bromo-2-deoxyuridine (BrdU, Sigma). In brief, a working solution of BrdUin PBS at 1 mg/ml was prepared and injected mice i.p. with1 ml (1 mg) of BrdU solution. Twenty-four hours later,colon tissues were collected, fixed in 10% neutral bufferedformalin, and embedded in paraffin. Immunohistochemistry was carried out using the BrdU In situ DetectionKit (BD Pharmingen, San Jose, CA, USA) as describedearlier (Zaki et al. 2010).Role of CRHR1 in colitis-relatedcancer21:4643also displayed enhancement of CRHR1 expression inthe carcinomatous tissues compared with normal andpericarcinomatous tissues (Fig. 1D). We further analyzedthe localizations of CRHR1 using immunohistochemistry.Similarly, CRHR1 and its ligands were less expressed inthe mucosal inflammatory cells of normal mice, whiletheir expression were all upregulated in the CAC mice.Interestingly, CRHR1 was mainly located in inflammatorycells of pericarcinomatous area, while CRHR1 were mostlyexpressed in the pejorative epithelial cells in the tumorarea (Fig. 1E). These results indicated that increasedCRHR1 might have an important biological functionduring the development of CAC.Endocrine-Related CancerTUNEL stainingThe TUNEL procedure was performed using the in situ CellDeath Detection Kit (Roche Applied Science). Proteinase K(20 mg/ml, Sigma) was applied to the tissue sections for15 min at room temperature. Endogenous peroxidasewas blocked by incubation of the sections with 2% H2O2for 5 min. The sections were incubated with the TdTenzyme for 2 h at 37 8C. Antidigoxin-peroxidase solutionwas applied for 30 min, followed by exposure to diaminobenzidine (DAB) substrate for 3–5 min and counterstaining with hematoxylin.Statistical analysisData were represented as meanGS.E.M. The differencein survival was shown by Kaplan–Meier plot. The log-ranktest was used to compare significant survival difference.Statistical significance was determined by Student’st-test. A P value !0.05 was considered statisticallysignificant.ResultsExpression of CRHR1 in the colon of mice and CRC patientsTo explore the role of CRHR1 in CAC development,Crhr1C/C mice were injected with a single dose of theDNA-methylating agent AOM followed by three rounds oforal administration of DSS to trigger chronic CAC (Fig. 1A)and the mice were fed with tap water as the controls. Thequantitative real-time PCR showed that the expression ofCRHR1 and its ligands (UCN1 and CRH) were obviouslyincreased in the colon of CAC mice compared withcontrols (Fig. 1B) and similar results were observed at theprotein level of CRHR1 by western blotting (Fig. 1C).As in the model of CAC mice, slices from CRC patientshttp://erc.endocrinology-journals.orgDOI: 10.1530/ERC-14-0239q 2014 Society for EndocrinologyPrinted in Great BritainCRHR1 deficiency contributed to the alleviation ofcolitis-associated tumorigenesisTo dissect the exact effect of CRHR1 on CAC, Crhr1K/Kmice were generated and we induced colon tumorigenesiswith AOM and DSS as mentioned above. Changes in bodyweight were monitored daily throughout the studyduration and colonic tumor burden was determined80 days after AOM and DSS treatment. Mortality andweight loss were significantly reduced in Crhr1K/K micecompared with Crhr1C/C during the early stage of tumorinduction (day 10 after AOM injection) (Fig. 2A and B).Consistently, Crhr1K/K mice were markedly protectedfrom AOM and DSS-induced tumorigenesis (Fig. 2C, D, E,and F).Decreased tumor burdens were associated withlower incidence of dysplasia and less inflammatorycytokines expressionHistological examination revealed that 70% of Crhr1C/Cmice developed high-grade dysplasia, of which 30% wereclassified as adenocarcinoma with invasive growth. Bycontrast, only 40% of Crhr1K/K mice displayed high-gradedysplasia and no adenocarcinomas were observed in anyof Crhr1K/K (Fig. 3A and B). Histological scores from thequantifications of ulceration, inflammation, and hyperplasia of the mucosa were significantly decreased inCrhr1K/K mice (Fig. 3C and D). Besides, both mRNA andprotein expression of proinflammatory cytokines, such asIL1b, IL6, and TNFa, were markedly lower, whereas theanti-inflammatory factor, IL10 was significantly higher inCrhr1K/K than that in Crhr1C/C mice (Fig. 3E). We nextanalyzed the expressions of multiple cytokines andtumorigenic factors cycloxygenase 2 (COX2) and interferon gamma (IFNg) in colon tissue as these factors oftenPublished by Bioscientifica Ltd.Downloaded from Bioscientifica.com at 02/14/2022 08:11:13PMvia free access
Y Liu et al.ResearchBCrhr1 / Crhr1 –/–6040200CCrhr1 / Crhr1 –/–1.21.51.11.00.9**0.8Crhr1 / Crhr1 –/–1.00.5*0.001020304050607080Days (d)Days (d)DEF20Percentage of tumor size(diameter)Number of tumors in per colon1001510504020r1 –/– 2 mm2–5 mm 5 mmrhCrhr1 –/–60CCrhr1 / r1 / Crhr1 –/–rh / 800CCrhr1Crhr1 / Crhr1 –/–**25Endocrine-Related 7880Percent survival8021:4Tumor incidence (%)100Body weight change (%)ARole of CRHR1 in colitis-relatedcancerFigure 2Decreased CAC tumorigenesis in Crhr1-deficient (Crhr1K/K) mice.(A) Survival rate of Crhr1C/C mice (27.27%) and Crhr1K/K mice (47.62%)were shown by the Kaplan–Meier plot. The log-rank test indicated therewere significant survival differences between Crhr1K/K (nZ21 mice pergroup) and WT (Crhr1C/C) (nZ33 mice per group) PZ0.001. (B) Bodyweight loss was shown. Day 15 (Crhr1C/C: 79.77%G0.389%; Crhr1K/K:96.13%G0.775%) and day 18 (Crhr1C/C: 78.6%G1.22%; nZ11; Crhr1K/K:103.96%G0.60%; nZ17). *P!0.05 vs Crhr1C/C. (C) The incidence of tumorwas analyzed (Crhr1K/K: nZ17 mice per group; Crhr1C/C: nZ11 mice pergroup). (D) Mice were killed to determine tumor development in the colonon day 80. (E) Numbers of tumors in the whole colon were counted (nZ6mice per group) Crhr1C/C: 16.4G0.35; Crhr1K/K: 6.3G0.36). (F) Diameter ofthe tumors was measured at the end of the study (nZ6 mice per group).Data represented meanGS.E.M.; *P!0.05, **P!0.01 vs Crhr1C/C.drive tumorigenesis. Similarly, mRNA levels of Cox2 andIfng were markedly reduced in Crhr1K/K mice than thosein Crhr1C/C mice (Fig. 3F). These results suggested thatCRHR1 activation increased the risk of tumorigenesis withenhanced inflammation and hyperplasia, and a higherincidence of dysplasia.analysis revealed more severely damaged colonic mucosawith extensive loss of crypt structures and epithelial celldenudation, larger areas of ulceration, and more extensiveinfiltration of inflammatory cells in Crhr1C/C group(Fig. 4C), which was also reflected in the pathologicalassessment of colitis severity scores (Fig. 4D and E). Takentogether, these results suggested that CRHR1 played acritical role during the early stage of colitis-associatedtumorigenesis, because from day 25 onwards, occurrenceof tumor formation was observed as described above.CRHR1 was critical in tumor induction during theearly stage of CACAs described earlier, the weight loss and survival ratedifferences between Crhr1C/C and Crhr1K/K mice weredetected at the early stage of tumorigenesis. These resultspromoted us to hypothesize that CRHR1 influencing ontumorigenesis occur early from the onset of tumorigenesis. To characterize this possibility in detail, we collectedthe colons from mice killed at day 10, 15, and 25 afterAOM injection. Interestingly, colons from Crhr1K/K micewere significantly longer than those from Crhr1C/C miceafter day 15 (Fig. 4A and B). In addition, .orgDOI: 10.1530/ERC-14-0239q 2014 Society for EndocrinologyPrinted in Great BritainInflammatory cell activity was decreased in Crhr1K/K micePrevious studies suggested that CRHR1 was a keyinflammation regulator (Xu et al. 2009, Zocco et al.2010). To further confirm the effect of CRHR1 oninflammation in terms of CAC, inflammatory cytokineproduction was analyzed during day 0 to day 25. Notsurprisingly, the mRNA expression for Il1b, Il6, and Tnfawas decreased, while Il10 was increased in Crhr1K/K micePublished by Bioscientifica Ltd.Downloaded from Bioscientifica.com at 02/14/2022 08:11:13PMvia free access
Y Liu et al.ResearchRole of CRHR1 in colitis-relatedcancerCrhr1 / AdenocarcinomaCrhr1–/–High gradeLow gradeRelative mRNAEA1.5100 Low gradeHigh gradeAdenocarcinoma1.0Crhr1 / Crhr1–/–Crhr1–/–IL1β31 kDaActin43 kDa***TNFαCrhr1 / 1.0Crhr1–/–TNFα23 kDaActin43 kDa0.5***0.00.5Relative mRNA1.50.0Crhr1 / CHistology scoreCrhr1–/–Crhr1 / Crhr1–/–4*Crhr1 / 1.00.5***Crhr1–/–IL626 kDaActin43 ative mRNA*2flaIL60.030**Crhr1 / Crhr1–/–40IL1017 kDa20Actin43 kDa0DF121.586***420Crhr1 / Crhr1–/–1.00.50.01.5IFNγ***Relative mRNA10Relative mRNATotal histology scoreEndocrine-Related CancerPercentage of micewith dysplasia1.5Relative mRNABCrhr1 / 0.51.5200 645IL1β1.00.021:4COX2Crhr1 / Crhr1–/–1.00.5***0.0Figure 3Alleviated CAC severity in Crhr1K/K mice attributed to reduced inflammationresponse. (A) Representative images of H&E staining of colon sectionsshowing dysplasia. (B) Overall grading of dysplasia in each genotype. (C) H&Estained sections were scored for inflammation, ulceration, hyperplasia, andinflamed area, and determined in a double-blind manner. (D) Total histologyhttp://erc.endocrinology-journals.orgDOI: 10.1530/ERC-14-0239q 2014 Society for EndocrinologyPrinted in Great Britainscores from Crhr1C/C mice (scoresZ10G0.20) and Crhr1K/K mice(scoresZ4.2G0.33). (E) Expression of IL1b, IL6, IL10, and TNFa in colon wereanalyzed. (F) RNA for expression analysis of IFNg and COX2 by real-time PCR.Data represented meanGS.E.M.; nZ5–7 mice per group; *P!0.05, **P!0.01,***P!0.001 vs Crhr1C/C littermates.Published by Bioscientifica Ltd.Downloaded from Bioscientifica.com at 02/14/2022 08:11:13PMvia free access
Y Liu et al.ResearchADay 0Day 10Role of CRHR1 in colitis-relatedcancerDay 15Day 25CDay 0Day 1021:4Day 15646Day 25Crhr1 / 200 Crhr1 –/–200 Histology E***1ype–r1 –/rhCCrhr1 / r1 –/–CCrhr1 /Crhr18Crhr1 / Crhr1 –/–3Infla**Crhr1 / –/–Totalhistology scoreColon length (cm)10Endocrine-Related Cancer4nBrh – r1 –/r1 /rhCCrhrhCCrhr1 / r1 –/–D***Crhr1 / Crhr1 –/–Figure 4CRHR1 induced tumor at the early stage of tumorigenesis. (A, B, and C)Mice were killed at day 0, 10, 15, and 25 after AOM injection. (A and B)Changes in colon length was monitored. (C) Mucosal histology wasexamined by H&E staining. (D and E) Colitis severity scores were determinedat day 25 in a double-blind manner. Data represented meanGS.E.M.; nZ9 pergroup; *P!0.05, **P! 0.01, ***P! 0.001 vs Crhr1C/C littermates.after day 10 (Fig. 5A). We therefore hypothesized that theloss of CRHR1 may protect from colitis-associated tumorigenesis by attenuating immune cell activation andinflammatory responses in response to DSS treatment. Totestify this possibility, immunohistochemical analysis wasused to characterize the immune cell associated with theinduction of hyperinflammatory responses in the colon.During inflammation response, more lymphocytes andmacrophages infiltrated into the colon mucosa of Crhr1C/Cmice (Fig. 5B). To determine the inflammatory cell typeregulated by CRHR1, immunostained mucosa of largeintestine with the markers of macrophage, B cells, T cells,and anti-CRHR1 was examined. The results showed thatCRHR1 was mostly detected in macrophages but not in Bcells and T cells (Fig. 5C). Flow cytometry analysis showedthat lower levels of macrophages in the whole peripheralblood of Crhr1K/K mice than in those of Crhr1C/C micefrom day 10 (Fig. 5D). To further characterize whetherCRHR1 deficiency could affect the secretion of inflammatory cytokines, mononuclear cells (macrophage precursors)collected from the whole peripheral blood of Crhr1C/Cand Crhr1K/K mice were equally seeded into plate andstimulated with LPS for 6 h, and the inflammatory factorsin the supernatant were monitored using ELISA. The ELISAanalysis showed significantly less IL6 and TNFa releasedfrom mononuclear cells in Crhr1K/K mice, but nodifference in the levels of IL1b and IL10 between Crhr1K/Kand Crhr1C/C mice (Fig. 5E).Thus, these results suggested that less susceptibletumorigenesis of Crhr1K/K was partly owing to weakerinflammatory response in inflammatory cells, especiallythe OI: 10.1530/ERC-14-0239q 2014 Society for EndocrinologyPrinted in Great BritainCRHR1 regulated colonic cells survival andproliferation through NFkB and STAT3 signalsThe expression of tumorigenic and proinflammatorygenes is modulated by signal transduction pathwaysmediated by NFkB and STAT proteins. To understandwhether these pathways and molecules were deregulatedin the presence of CRHR1, we examined the activation ofNFkB and STAT signaling pathways by western blotting.Indeed, after AOM/DSS treatment, significantly higheractivation levels of NFkB (p65 phosphorylation) andphosphorylated STAT3 were observed in the colon tissueof Crhr1C/C mice at day 25 after AOM injection (Fig. 6A).Published by Bioscientifica Ltd.Downloaded from Bioscientifica.com at 02/14/2022 08:11:13PMvia free access
Y Liu et al.ResearchCRHR12520ayDDay1510ayayDDRelative mRNA***10***52520400 Day15ayDCD20Day25100DF4/80MacsCrhr1 / 400 Crhr1 –/–Cell number ( 105)80Endocrine-Related Cancer400 NFα1.5Crhr1 / Crhr1 –/–1.5ay******0.010Relative mRNA***Relative mRNA**10Relative mRNA1.00.5CIL6IL1β1.5DARole of CRHR1 in colitis-relatedcancerCrhr1 / Crhr1 –/–60*4020**Day 15Day 250Day 10400 Figure 5The presence of CRHR1 led to increased inflammatory cell activation incolon tissue. (A) Real-time PCR was carried out to detect the expression ofIL1b, IL6, IL10, and TNFa in the colons collected from day 0, 10, 15, and 25after AOM injection. (B) Colon tissue collected at day 25 was immunostained for the macrophage marker F4/80, B cell marker CD20, and T cellmarker CD3. (C) Mucosa of large intestines (collected at day 25) was stainedwith markers of macrophage, B cells, T cells, and ant
Crhr1 C/ mice during treatment with AOM and DSS. Tumorigenesis was significantly reduced inCrhr1K/K mice, . (Shacter & Weitzman 2002, Karin et al. 2006, Lin & Karin 2007). . Another key player in apoptosis is the