Transcription
Review ArticleiMedPub Journalshttp://www.imedpub.comJournal of Healthcare CommunicationsISSN 2472-16542016Vol. 1 No. 4: 36DOI: 10.4172/2472-1654.100036A Comprehensive Review of an ElectronicHealth Record System Soon to AssumeMarket Ascendancy: EPIC AbstractIntroduction: Federal and state mandates have compelled healthcare systems toadopt “meaningful use” electronic health record (EHR) systems. Off-the-shelf, onthe-spot, one-source EHR systems such as EPIC have become popular choices.Indeed, EPIC recently captured a substantial proportion of the Houston TexasMedical Center (TMC), CVS Pharmacy mini-clinics, and extended into academicinstitutions. Current reported estimates are contentious but vary between 2047% of the EHR market share. Therefore, it is only sensible to conduct a reviewof EPIC.Aim: The intent of this article is to report a systematic and comprehensive reviewof the scientific literature regarding EPIC’s advantages and disadvantages in termsof “meaningful use”.Method: Findings reported herein derive from a grounded, iterative review ofopen-source, peer-reviewed scientific literature on EPIC.Findings: EPIC excels providing accurate/connected information virtually inreal time with which to adjust medical practice. However, hidden costs areassociated with EPIC, including expensive vendor support and add-on programs,“technological somnambulism,” increased data entry “after-hours tax,” andtraining. Nevertheless, EPIC can enhance patient safety, monitoring, tracking,continuity of care, and patient involvement. It also has promise as a medicaleducation tool. However, end-user satisfaction has never exceeded 70% (C-). EPIChas failed in terms of e-document management, especially for human researchsubject protection. Finally, results are reported from a preliminary examination ofEPIC transition Help Desk online responses.Ralph J Johnson IIIDivision of Pastoral Care, CHI St. Luke'sHealth/Baylor St. Luke's Medical Ctr, andUT-MD Anderson Cancer Centre, Houston,Texas, United StatesCorresponding author:Ralph J Johnson III , Catholic Chaplain’s Corps, Division ofPastoral Care CHI St. Luke's Health/BaylorSt. Luke's Medical Ctr, 6720 Bertner Ave,Houston, TX 77030, USA.Tel: 832-372-3511Citation: Johnson III RJ. A ComprehensiveReview of an Electronic Health RecordSystem Soon to Assume MarketAscendancy: EPIC . J Healthc Commun.2016, 1:4.Conclusion: EPIC provides a high-quality, tech-savvy front-end-to-back-end EHRsystem for collecting and managing accurate “raw” inter-connected medicalrecord data for timely reporting. However, it carries substantial hidden costs.Also, EPIC is lacking in the management of e-documentation. Avenues for futureresearch are considered regarding EPIC.Keywords: Electronic health records; EHR systems; EPIC; Health informationtechnology; Meaningful use; Texas medical centerReceived: August 03, 2016; Accepted: September 12, 2016; Published: September23, 2016IntroductionHealth information technology (HIT) has become fundamentalto healthcare improvement and will be a primary strategy forenriching its quality, enhancing patient management, extending/expanding research, and evolving capabilities in healthcaredelivery [1-4]. Research has identified more effective HIT as thekey to closing quality and safety gaps in the healthcare system[3,5]. Thus, the U.S. federal government has enacted legislation topromote health providers’ and medical practitioners’ “meaningfuluse” of electronic health record (EHR) systems, with the federalgovernment providing funding incentives for compliance with the Under License of Creative Commons Attribution 3.0 License This article is available in: ve.php1
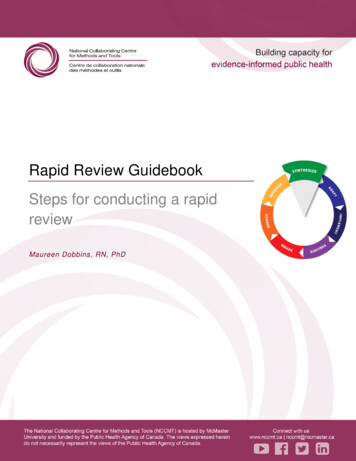
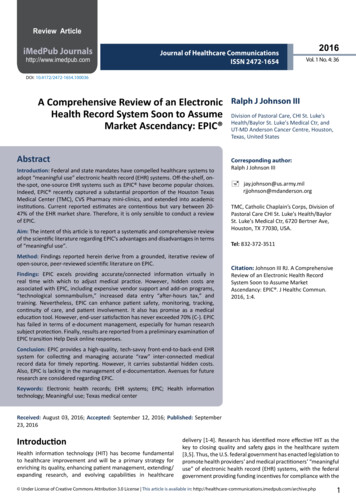
ARCHIVOSDE MEDICINAJournal of “meaningful criteria” [2,6-8]. The federal and state governmentshave also enacted legislation and regulatory mandates andpenalties for not embracing EHRs that are certified “meaningfuldata producers” [9]. This is because the traditional or legacy EHRwas developed strictly as a document storage, management, andretrieval system for provision of clinical care. It was not designedfor front-end-to-back-end seamless data extraction, subsequentanalyses, or virtually real-time reporting [2,10-13]. Also, legacyEHRs permitted unstandardized and disjointed entries, therebyproducing variation in content. Furthermore, this resulted inclinical data housed in multiple disconnected systems, furtherrestraining efficient and meaningful EHR analyses [14].On-the-spot, commercial EHR systems are increasingly beingadopted because of their certified off-the-shelf and instantaneouspotential to produce the “meaningful data” required to qualifyfor financial incentives or avoid penalties for non-compliance[1,3]. Also, it is only common sense for large-scale patient caredelivery and academic research systems to acquire the latesttechnological advances as the industry in general shifts to pursuethe power that meaningful data-producing EHRs possess [1,6].For many small and medium-sized hospitals and healthcaresystems, this translated into one vendor, EPIC , which in thepast had widespread adoption among small and medium-sizedmarkets [1,15] and where EPIC “cut its teeth.” EPIC products arenot only certified to produce meaningful use data but they alsoleverage an incredibly powerful electronic connectivity, therebypermitting more rapid and thorough data transfers, expansions,and extensions from and to other EPIC-based systems, as well asmore efficient and rigorous data analyses [1].EPIC previously had held a constant yet commanding EHR marketshare with approximately a 20% share of the EHR market [16-19].EPIC is one of the “Big 8” meaningful use EHRs—that offer somesimilar features as EPIC . The percentage of academic institutionsusing EPIC is unknown but is estimated to be substantial andgrowing [20]. Nevertheless EPIC is now poised to extend itsmarket reach to large-scale and global hospital/healthcaresystems, medical research institutions, and elsewhere. Forexample, five out of six research hospitals and medical facilitiesin the world’s largest medical center, the Texas Medical Centerin Houston, are adopting EPIC as their EHR system in 2016 [20].With this and other recent coups, though recent unconfirmedestimates are contentious, it appears EPIC may capture morethan 25% of the EHR market share, potentially shifting controlof future markets and even other systems its way. Due to itsrapid market penetration, EPIC now exercises vast potentialcontrol of healthcare itself through decision support rules, ordersets, visualizations, quality measurement, and coordinationand control of workflow. This is not nefarious but the reality ofsubstantial software shaping workflow, data, standards, anddefinitions.Therefore, it is worth taking a long and hard look at EPICregarding its benefits and drawbacks in terms of meaningfuluse through a systematic review of the literature, includingstandardized data collection, technological somnambulism, timecommitments and productivity, real-time data warehousing and(patient-centered) efficient production of outcome measures,22016Vol. 1 No. 4: 36enhanced patient safety, patient tracking and follow-up, enduser satisfaction, reminders, patient involvement, potential usein medical education, training, issues for research, and practicalexperience regarding recent implementation in the Texas MedicalCenter. (Note: There are other systems similar to EPIC and betteror worse; however, this article is not a comparative analysis.Rather, given its recent market ascendency this article’s focus ison what is known about EPIC in the literature and the positive ornegative aspects described are probably not unique only to EPIC).MethodThe findings in this article derive from a systematic, iterativeliterature review on EPIC that is depicted in Figure 1.Figure 1 depicts the evidence-based and best practices literaturereview research process that informed the work reportedherein through which open-source peer-reviewed articles wereidentified then reviewed and conceptual themes generated.Essentially, Figure 1 describes the steps in this process. Stepone involved deriving relevant keywords with which to searchfor articles. Step two was targeting appropriate peer-reviewedmedical/health and open-source subject matter databases. Stepthree was applying the search terms to online medical databases.Steps four and five were the identification and retrieval ofrelevant articles and removal of duplicates. Step six was retrievaland review of abstracts or executive summaries. Step seven wasgathering the articles and step eight was reviewing their contentfor relevance. Step nine was identification and enumeration ofthemes and the retrieval of related information for review untilall themes were exhausted with the outcome, and step ten wasthe review. Given that the process is “theoretically grounded”[21], though the steps are generally sequential and linear, theycan be repeated individually or the researcher can cycle back andforth between steps or back through the process. However, theeventual and ultimate aim was the identification, summation,and exhaustion of all themes. The one limitation in this methodis that not all possible themes in the universe may have beenidentified. However, this does not suggest that those identifiedherein are any less important or meaningful.FindingsStandardized data collectionEPIC’s potential for improving healthcare lies in its abilityto connect information and retrieve standardized data forcomparative analysis and because it requires pre-determineddata outcome measurements [2,3,11,14,15,22,23]. Grigoryanet al. [24] found EPIC’s Clarity module was essential in terms ofidentifying low compliance with current medical best practicesand misuse of medications that could prove deadly. Specifically,EPIC was able to generate accurate (and timely) reports basedon requirements for entry of standardized data codes (e.g., EPIC“hard stops”), in this case diagnosis codes [2,3,23]. These codescan be immediately queried for programmatic evaluation andmodification research. However, Koppel and Lehman’s work [15]cautiously insinuates that a disadvantage of monopoly or marketdominance and a monoculture is that it maintains antiquatedThis article is available in: ve.php
ARCHIVOSDE MEDICINAJournal of Vol. 1 No. 4: 36Likewise, Katzan et al. [2] noted that EPIC provides “ theadditional software layers for easy access to (standardized) clinicalinformation and serves as an accessible, evaluable platform forcollecting and analyzing clinical outcomes .” This team noted thatEPIC can be conformed to shepherd data entry and pre-identifyerrors and error patterns at the moment clinicians enter data.Thus, data points can be identified and evaluated virtually in realtime, almost immediately enhancing accuracy and quality of dataas well as informing medical service adjustments [2,22,23,2729]. Also, it should be noted that EPIC improves healthcare byproviding high-quality, integrated standardized documentationfor ordering medications, therapies, and procedures. Dataanalytics though important are a secondary outcome of thisprecision and not the primary reason for its implementation.Step 1Key Words/TermsStep 2On-line MedicalDatabaseIdentificationStep 3Apply KeyWords/TermsStep 4One challenge Bornstein [13,14] reported was that whenKaiser-Permanente (KP) transitioned from a ‘legacy documentmanagement system’ to EPIC, KP found EPIC ill-suited for backloading data and information in the standard format, whichresulted in multiple and expensive remediation efforts. Backloading continued to be a chronic and long-term problem resultingin maintenance and the attendant expense of supporting severaldifferent systems that EPIC was supposed to eliminate in the firstplace. Conversely, Borstein [14] observed that EPIC was easily ableto capitalize on its standardized real-time workplace data entry ofmedical-condition-service-for-fee codes to identify patterns andpractices. It permitted non-intrusive, accurate, and virtually realtime identification for analyses that could continuously operateunnoticed in the background [2,22-24,30].Medical DatabaseIdentificationStep 5Article AbstractRetrieval & DiscardDuplicatesStep 6Article AbstractReviewStep 7Retrieve ArticlesStep 8Review ArticlesStep 9Identification &Enumeration ofThemes/Info forInclusion2016Literature ReviewFigure 1 “Grounded” literature review process.programming and retard responsiveness, de-confliction,flexibility, enhancement, and the ability to evolve. Also, this stateof affairs locks purchasers into EPIC such that any disruption ofthat unitary system will result in disturbances in nascent dataflows, data format standards, and user interface templates [15].Carberry et al. [3] revealed that incorporating patient-centeredstandardized measurement tools at the medical conditionlevel required an iterative collaboration and inter-disciplinecommitment among clinicians, analysts, and data architects,which the EPIC system fostered [25]. They cautioned that thisprocess can be resource and time intensive and risked wastefulduplication of efforts, but the end-product was well worth thetrouble. Lindholm et al. [26] found a statistically significant (p 007)difference in that EPIC produced 78% greater identification ofpotential candidates for tobacco cessation. This was because EPICallows for modification/inclusion of evidence-based prompts andhard stops for identifying and mandating standardized data entry. Under License of Creative Commons Attribution 3.0 LicenseDeBoer et al. [11] were able to leverage EPIC’s standardizeddata-ready feature to track medical procedures and substantiallyreduce unplanned outcomes. Also, Sweet et al. [31] used EPIC’sstandardized data infrastructure to facilitate genetic counsellingfor multiple complex diseases and pharmacogenetics as well asclinically based decision support. Bain [13] validated the fact thatEPIC’s front-end-back-end standardized data entry and queryand data report generator eliminated the expensive, repetitiveloading of data into multiple different systems. The old processwas a by-product of traditional e-document managementsystems. The latter process involved by-hand data transfer andwas prone to error and duplication of effort by simple virtue ofadditional and unnecessary steps [2].Technological somnambulismAlong with hard-stop-enabled standardized data entry come itsdownside, namely, risk for reflexive and non-reflective technologydriven hypnosis and even sleepwalking [32-36]. Carberry et al.[3] highlight an issue surrounding EPIC that is inherent in allEHRs with “meaningful use” capabilities. Specifically, frontend data collection is shepherded, entailing over-reliance onpre-determined existing (“canned’) forms and templates forinformation collection—as opposed to producing meaningfuldata. This can be further complicated by polished and slick-veneerelectronic systems. Carberry et al. [3] found that meaningfulmeasurement had to be identified by an outcome measurementteam that worked with dedicated vendor-trained analysts. Thisteam’s mission was to build sophisticated customized forms andtemplates relevant to particular organizations and their missions3
ARCHIVOSDE MEDICINAJournal of and designed to capture information throughout the medicalcare cycle [25].In this regard, EPIC’s drawback is that it does not permit enteringmore specific or different information [2], except through theincorporation of add-ons that detract from its overall efficiency. Insupport of this contention, Makam et al. [1,37] found that with theintroduction of EPIC, little extemporaneous dictation exceeded thestandardized templates or pre-populated phrases. Interestingly,this team also observed a curved-linear and statisticallysignificant relationship between use of standardized data entryand years after graduation from medical school. Specifically,they found a linear correlation between use of standardized dataentry that maxed at 14 years post-medical school graduation andthen decreased exponentially. They suggested that this findingmight also point to a relationship between familiarity with thetechnology and the advent of the more recent tech-savvy (i.e.,Nintendo) generation that grew up with the technology and takeit for granted almost unquestioningly.Time commitments and productivitySeveral issues are incumbent with all “meaningful use” EHRsthat turn clinicians into data entry clerks. One is the additionaltime commitment of entering data loaded onto the already timeintensive commitments of clinical practice [1,13,14,37]. EPICseems to be no different. Hammoud et al. [32,36] reported thatmedical students spent a substantial amount of time enteringdata into EPIC—more so than physicians—and this was apossible distraction from their medical studies. Bornstein [1,14]noted that added documentation in EPIC also added burden onphysicians. However, the resulting seamless data analysis waswell worth the effort from the physicians’ perspective. Makamet al. [1] also noted a substantial “after hours’ time tax” to enterinformation and there may not be time-savings over paper chartsin terms of clinical visits. They found that on average 43% ofclinicians reported an additional 1-3 h spent on EPIC data entryor about 45 minutes for every hour of medical practice. Yet ina case-controlled study conducted by Barnett, Mehorta, Jena,and Newhouse [38] found, despite clinical staff additional timecommitments to entry into EHRs, especially EPIC , there was notadverse effect on patient care.Carberry et al. [3] observed the aspect of EPIC that makes it trulydesirable for outcomes measurement, program evaluation, andresearch, specifically, its hard stops. However, this also is a severedetraction or Achilles’ heel in that they disrupt smooth work flowand also result in end-use dissatisfaction [14,33]. Nevertheless,Cheriff et al. [13,37] reported that medical providers’ productivitywork volume, charges, and work relative to volume units actuallyincreased with EPIC. The caveat was that it took several monthsof EPIC experience to realize increased productivity. The authors’ultimate conclusion was that worker apprehension about EPICadoption due to lost productivity was grossly unfounded andcounterproductive.Real-time data warehousing and (patient-centered)efficient production of outcome measuresEPIC excels when it comes to generating reasonably accurate(and extremely timely) outcome measures, which is the essence42016Vol. 1 No. 4: 36of “meaningful use” [1,3,11,13,22-24,30,38-42]. Goldberg etal. [1,11,13,14,39,41,43] found that EPIC was responsible fora dramatic decrease in multi-center decision support systemsand time-to-decision. Heidemann et al. [30,37-40] showed thatphysician use of data output substantially and geometricallyimproved accurate identification of drug-induced liver disease.However, this was not possible without an add-on program thathelped analyze the raw data that the back-end of EPIC produced[30,41].Bellon et al. [8,14,22] found that EPIC’s patient-centered MyChart data reports feature provided sufficiently accurate data tomake evaluation comparisons on prescription practices on whichto base policy decisions. My Chart also provides patients withsummary medical information on their case in real time. Unni etal. [34] reported that EPIC’s FRAX analysis tool underestimatedosteoporosis risk factors and that it underestimated an average10 years probability of any major risk factors. This was the resultof EPIC only supporting passive data collection in terms of riskfactors [3]. This study called into disrepute EPIC’s independentability to collect relevant outcome data. Nevertheless, Steidl andZimmerman
EPIC previously had held a constant yet commanding EHR market share with approximately a 20% share of the EHR market [16-19]. EPIC is one of the “Big 8” meaningful use EHRs—that offer some similar features as EPIC . The percentage of academic institutions using EPIC is unk