Transcription
INFUSION NURSES SOCIETYPolicies andProceduresforInfusion Therapy:AmbulatoryInfusion Centers1st edition
Policies andProceduresforInfusion Therapy:Ambulatory InfusionCentersINFUSION NURSES SOCIETYSETTIN G TH E STAN DA RD FO R I NFUS I ON CARE
Copyright 2019 by the Infusion Nurses Society, Inc. All rights reserved. No part of thisbook may be reproduced without written permission from the Infusion Nurses Society.
CONTENTSPREFACE. 6Infusion Therapy in the Ambulatory Infusion Setting. 71. GENERAL ORGANIZATIONAL POLICIESInfusion Team. 12Competence and Competency Validation.14Product Evaluation, Integrity, and Defect Reporting. 17Informed Consent. 19First Dose Administration. 23Latex Sensitivity or Allergy. 25Adverse and Serious Adverse Events. 272. INFECTION PREVENTION AND SAFETY COMPLIANCEHand Hygiene. 31Sharps Management. 34Medical Waste Disposal. 36Durable Medical Equipment Disinfection. 37Standard Precautions. 39Transmission-Based Precautions. 423. VASCULAR ACCESS DEVICE PLACEMENTVascular Access Device (VAD) Planning. 46Local Anesthesia. 52Short Peripheral Catheter (SPC) Placement. 56Ultrasound-Guided Short Peripheral Catheter (SPC) Placement. 63Ultrasound-Guided Midline Catheter Insertion. 68Ultrasound-Guided Peripherally Inserted Central Catheter (PICC)Insertion Using Modified Seldinger Technique (MST). 77
4. SITE CARE AND MAINTENANCEAdministration Set Change. 88Maintaining Vascular Access Device (VAD) Patency:Flushing and Locking. 91Vascular Access Devices (VADs):Ongoing Assessment, Site Care, and Dressing Change. 96Vascular Access Device (VAD) Removal. 1025. INFUSION-RELATED COMPLICATIONS:IDENTIFICATION & INTERVENTIONAir Embolism. 108Allergic Reaction and Anaphylactic/Anaphylactoid Reactions. 111Catheter Damage.114Central Vascular Access Device (CVAD) Malposition.118Central Vascular Access Device (CVAD) Occlusion.122Central Vascular Access Device (CVAD)-Associated VenousThrombosis. 129Circulatory Overload. 133Infiltration/Extravasation. 135Nerve Injuries. 145Phlebitis. 148Vascular Access Device (VAD)-Associated Infection. 1526. OTHER INFUSION-RELATED PROCEDURESPreparing Parenteral Medications. 157Implanted Vascular Access Port: Accessing and Deaccessing. 160Phlebotomy: Blood Sampling from a Vascular Access Device (VAD). 166
7. OTHER INFUSION ACCESSIntraspinal Access Device: Care and Management. 175Subcutaneous Access Device: Placement and Infusion Administration. 183Intraosseous Access Device: Placement, Care, and Management. 1888. INFUSION THERAPIESIV (Intravenous) Administration: Continuous Infusion, IV Push,Intermittent Infusion. 194Transfusion Therapy. 205Parenteral Nutrition. 212Antineoplastic Therapy. 216Biologic Therapy. 223Patient-Controlled Analgesia (PCA). 227Moderate Sedation/Analgesia. 231Therapeutic Phlebotomy. 234IllustrationsVein Anatomy.239Policies and Procedures for Infusion Therapy: Ambulatory Infusion Centers isintended to reflect current knowledge and practices of the clinical specialtyof infusion therapy. Because clinical practice continuously evolves based onongoing research, clinicians should make an independent assessment of theappropriateness and applicability of a policy or procedures in any specificinstance. Applicable federal and state laws and regulations should also beconsidered, as well as the standard of care in a particular jurisdiction, as thesemay take precedence. INS is not responsible for injury to persons or property,or other harm, arising from exercising guidelines outlined in this publication.Suggested citation for this publication:Infusion Nurses Society. Policies and Procedures for Infusion Therapy: AmbulatoryInfusion Centers. Norwood, MA: Infusion Nurses Society; 2019.
. Policies and Procedures for Infusion Therapy: Ambulatory Infusion CentersPrefaceWhile a patient’s plan of care for infusion therapy often begins in the hospital,that care may transition to other practice settings. Ambulatory infusion centersoffer an environment where patients who don’t need to be hospitalized cansafely, efficiently, and cost-effectively receive their therapies. In our effortto ensure safe, quality infusion patient care, the Infusion Nurses Society(INS) develops resources to guide clinicians in their practice. We recognizethe invasive nature and risks associated with infusion care—not only to ourpatients, but to clinicians as well. Therefore, it’s imperative the resources aresupported by the most current research and best available evidence. Betterpatient outcomes result when there is consistency in practice among healthcare professionals. Incorporating practices from the Policies and Procedures forInfusion Therapy: Ambulatory Infusion Centers provides the framework to do justthat.As the basis for professional practice, clinicians are accountable within theboundaries of their scope of practice. With variations among health careorganizations, knowledge of the policies, procedures, and practice guidelinesof one’s organization is essential, as well as any directives from federal, state,or regulatory bodies. While the policies and procedures are written in generalterms, there may be device-specific features or specifications that need to befollowed for proper function, so clinicians need to adhere to the manufacturers’directions for use.The format for the Policies and Procedures for Infusion Therapy: AmbulatoryInfusion Centers includes the policy, which defines a course and purpose ofan action, and the procedure, which lists the steps needed to comply withthe policy. Sections on key points, assessment, and patient education havealso been added. While there are areas of care, such as infusion-relatedcomplications and infusion therapies that don’t fit the typical policy andprocedure format, inclusion was important as these areas directly impact thedelivery of infusion care.A bibliography accompanies each policy and procedure as a resource for thoseseeking more information. Since the 2016 Infusion Therapy Standards of Practicewas the primary reference for development of the policies and procedures, theindividual standards are not cited in the bibliography in order to minimizerepetition.As clinicians seek to provide safe infusion care and improved patient outcomes,the Policies and Procedures for Infusion Therapy: Ambulatory Infusion Centers isan indispensable resource in the quest to achieve consistency in practice—aprinciple INS fully endorses.Mary Alexander, MA, RN, CRNI , CAE, FAANINS Chief Executive Officer6
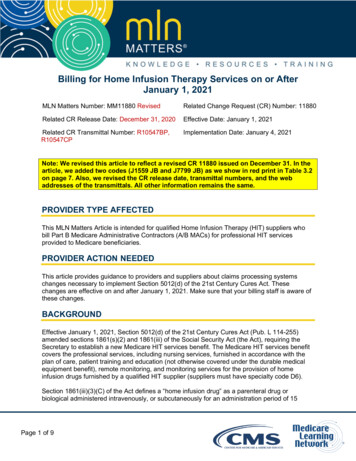
Infusion Therapy in the Ambulatory Infusion SettingThe high cost of health care and decreasing reimbursement have madeearly discharge from an acute care facility to an ambulatory infusion settingfor infusion administration a necessity. In some cases, hospitalization foruncomplicated conditions can be avoided by delivery of needed infusiontherapy at an ambulatory practice site.An infusion center may be located in a variety of health care environments,including a provider’s office, a hospital clinic, an urgent care center, emergencydepartment, or a free-standing infusion clinic. Infusion centers have healthcare professionals on-site and ready availability of medications, supplies, andequipment needed to respond to vascular access complications or emergencies.The nurse, physician, pharmacist, social worker, dietitian, and administrativestaff work together to provide an effective and efficient communication systemfor designing treatment programs and promoting positive patient outcomes.Infusion centers allow for coordination of resources and efficient deliveryof services. With staffing, equipment, and provider involvement similar tothose in a hospital, the infusion center is a practical way to initiate extendedoutpatient care. Because of this similarity, some patients may perceive thetransition from the hospital to the infusion center as less traumatic andperhaps better supervised than transitioning directly to home care and selfadministration. Specialized infusion services in the infusion center include,but are not limited to, vascular access device (VAD) care; antimicrobial,antifungal, and antiviral infusions; continuous or intermittent chemotherapyadministration; various intramuscular and subcutaneous injections, infusionsof intravenous immunoglobulin and other biologics, hydration solutions, andanalgesics; transfusion therapy; and parenteral nutrition administration.Patient Care ConsiderationsThe criteria for patient selection and monitoring of patients who receiveinfusion therapies in the ambulatory setting has been established by variousprofessional groups. The patient is the central member of the care team andmust participate in his or her own care. The patient’s mental and physicalabilities, self-confidence, anxiety, and fears should be assessed during dischargeplanning from the hospital. Limitations on ambulation, prolonged sitting,and access to transportation may weigh heavily against an ambulatory settingfor treatment. Yet, home care may not be appropriate either for patients wholive alone and are not able to adequately self-monitor their infusion care. Animportant role for the patient is reporting significant changes in vital signsand symptoms of adverse effects, including rash, nausea, vomiting, diarrhea,phlebitis, erythema, or purulence at the insertion site of the access device.Educating patients to be reliable team members involves encouraging them tocommunicate often with the nurse, physician, and pharmacist.7
. Policies and Procedures for Infusion Therapy: Ambulatory Infusion CentersPractice guidelines from the Infectious Diseases Society of America listfactors to be considered when evaluating patients for outpatient parenteralantimicrobial that include the following: There is a documented need for outpatient antimicrobial therapy. The patient’s health care resource needs are available at the proposedoutpatient site. Patient and/or caregiver is willing to participate in care. Mechanisms are in place for rapid and reliable communications forpatient monitoring. Patient and/or caregiver understand the risks, benefits, and economicconsiderations.VAD selection should be appropriate for the prescribed therapy. Peripheralcatheters may be appropriate for short-term infusion therapies. Theperipherally inserted central catheter is frequently the VAD of choice; longterm catheters such as tunneled catheters or implanted ports present anotheroption, especially when frequent blood draws are necessary in very activepatients or in children. The patient should be included and educated in thedecision process of VAD selection.Role of the Infusion NurseAs a method of public protection to ensure safety, the infusion nurse should beclinically competent in the safe delivery of infusion therapy and VAD insertionand/or management within his or her scope of practice in the ambulatorysetting. Pharmacological and technical advances demand that the nurseworking in an ambulatory infusion setting be specialized and knowledgeablein order to offset the risk involved and maximize value for the patient and thehealth care organization. The infusion nurse must demonstrate accountability,reliability, initiative, and effective communication and technical skills.Clinical competencies describe practice and educational requirementsand provide validation for professional infusion nursing practice. Clinicalcompetencies include many tasks that infusion nurses perform daily, such asinitiating, monitoring, and terminating infusion therapy; educating the patientor caregiver; and collecting and analyzing data. The ambulatory infusionorganization must define in their policy and procedure, the competencies thatare the responsibility of the infusion nurse and the organization. Competencyassessment and validation should be performed and documented initially andon an ongoing basis. Achieving and maintaining board certification, notedby the certified registered nurse infusion (CRNI ) designation, is one methodfor documenting continuing competence and should be encouraged andsupported.8
SummaryInfusion therapy is administered across all health care settings. When patientsare stable in the acute care setting yet still require ongoing infusion therapy,the most appropriate alternative setting should be selected. Increasingly,infusion therapies are safely initiated in a non-acute care setting withoutprior hospitalization. The patient’s specific infusion therapy needs along withfunctional and cognitive status, availability of caregiver or family support,home environment, and patient and provider preference are important factorsinfluencing the optimal infusion setting. Regardless of the setting, the role ofthe infusion nurse is essential in ensuring the best possible outcome for thepatient.BibliographyAmerican Nurses Association. ANA’s Principles for Nurse Staffing. 2nd ed. Silver Springs,MD: ANA; 2012.Corrigan A. Infusion nursing as a specialty. In: Alexander M, Corrigan A, Gorski L,Hankins J, Perucca R, eds. Infusion Nursing: An Evidence-Based Approach. 3rd ed. StLouis, MO: Saunders/Elsevier; 2010:1-9.Gorski L, Hadaway L, Hagle ME, McGoldrick M, Orr M, Doellman D. Infusiontherapy standards of practice. J Infus Nurs. 2016;39(suppl 1):S1-S159.Gorski L, Miller C, Mortlock N. Infusion therapy across the continuum. In: AlexanderM, Corrigan A, Gorski L, Hankins J, Perucca R, eds. Infusion Nursing: An EvidenceBased Approach. 3rd ed. St Louis, MO: Saunders/Elsevier; 2010:109-126.Norris AH, Shrestha NK, Allison GM, et al; Infectious Diseases Society ofAmerica. 2018 Infectious Diseases Society of America clinical practice guidelinefor the management of outpatient parenteral antimicrobial therapy. Clin Infect Dis.2019;68(1):e1–e35. doi:10.1093/cid/ciy745.9
. Policies and Procedures for Infusion Therapy: Ambulatory Infusion Centers10
1. GENERAL ORGANIZATIONAL POLICIESInfusion Team.12Competence and Competency Validation.14Product Evaluation, Integrity, and Defect Reporting. 19Informed Consent.21First Dose Administration. 23Latex Sensitivity or Allergy. 25Adverse and Serious Adverse Events.2711
. Policies and Procedures for Infusion Therapy: Ambulatory Infusion CentersInfusion TeamPolicyThe team is structured through its scope of service to meet patient andorganizational needs for safe, effective, and high-quality infusion therapy.Vascular access device (VAD) insertion and/or VAD management andsurveillance are performed by clinicians and/or teams with validatedcompetency.The infusion team is evaluated for effectiveness through collection, monitoring,and reporting of quality outcome and process data.Key PointsThe scope of services and hours of operation for the infusion team are clearlyidentified.When the infusion team works with many patient populations, responsibilitiesfor each aspect of infusion therapy are clearly delineated based on the requiredknowledge, skill(s), availability, and outcomes from clinicians and the team, aswell as the complexity, risks, and volume of the patients’ infusion therapies.Although there is overlap between groups of professionals within infusiontherapy, no single profession may claim ownership of any skill, activity, or task.Use the infusion team for infusion therapy product evaluation, education,and quality improvement initiatives, and to collaborate in the evaluation andimplementation of standardized evidence-based infusion therapy practices.Preferably the infusion team is led by a certified infusion nurse specialist(eg, CRNI ) with a staffing mix that may include registered nurses, licensedpractical/vocational nurses, and/or unlicensed assistive personnel.A designated infusion team increases first-attempt insertion success rateswith short peripheral catheters and decreases facility-acquired bloodstreaminfections, other complications, and accidenta
the infusion nurse is essential in ensuring the best possible outcome for the patient. Bibliography American Nurses Association. ANA’s Principles for Nurse Staffing. 2nd ed. Silver Springs, MD: ANA; 2012. Corrigan A. Infusion nursi