Transcription
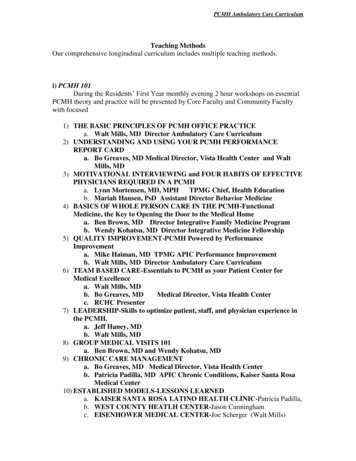
Colorado Community Health NetworkSpring ConferencePCMH : A WINDOW TO 2014Presented by:Bonni Brownlee, MHA CPHQ CPEHRNCQA PCMH Certified Content ExpertSenior Clinical Consultant
Audience Poll: Where are you now? Value of PCMH unclear Leadership not onboard Key positions fortransformation arevacant Fear of change Currently reviewingstandards Assembling PCMH teamMAYBE ACTIVE PCMH Team meetsregularly Actively collectingsupportingdocuments Already hit “submit”button Awaiting score PCMH Teamcontinues to meet Areas recognizedas problematicduring applicationphase are broughtforward to the QIPlan Reviewing 2014PCMH StandardsSUSTAINING
Why Attain Formal PCMH Recognition? Drives improvement in patient care and operating frameworkAlignment with Meaningful UseExternal validation of PCMH transformation andcommitment to high quality carePrideMarket advantagePotential for increased reimbursement and otherincentives
2014 NCQA PCMH Standards1. Patient-Centered Access2. Team-Based Care3. Population Health Management4. Care Management & Support5. Care Coordination and Care Transitions6. Performance Measurement and QualityImprovement
2014 NCQA PCMH STANDARDS1 Patient-Centered Access (10)4Care Mgmt and Support (20)A Pt-Centered Appointment AccessAIdentify Patients for Care ManagementB 24/7 Access to Clinical AdviceBCare Planning and Self-Care SupportC Electronic AccessCMedication ManagementDUse Electronic Prescribing2 Team-Based Care (12)ESupport Self-Care & Shared Decision MakingA Continuity5Care Coordination and Care Transitions (18)B Medical Home ResponsibilitiesATest Tracking and Follow-upC Culturally-Ling Appropriate ServicesBReferral Tracking and Follow-upD The Practice TeamCCoordinate Care Transitions6Perf Measurement & Qual Improvement (20)3 Population Health Management (20)AMeasure Clinical Quality PerformanceA Patient InformationBMeasure Resource UseB Clinical DataCMeasure Patient/Family ExperienceC Comprehensive Health AssessmentDImplement Continuous Quality ImprovementD Use Data for Population ManagementEDemonstrate Continuous Quality ImprovementEFReport PerformanceGUse Certified EHR TechnologyImplement Evid-Based Decision Support
PCMH 1: Patient-Centered Access1A: Patient-Centered Appointment Access1. Same-Day appointment availability2. Appointments outside of regular business hours 3. Availability of alternative visit types 4. Availability of appointments: Time to Third Next Available Appointment 5. Monitoring of No Show Rates 6. Acting on opportunities to improve access
PCMH 1. Patient-Centered Access1C. Electronic Access (use of patient portal) 1. 2. 3. 4.5.6.More than 50% of patients have online access to healthinformationMore than 5% of patients view, are able to download,or transmit their health informationClinical summaries provided within 1 day for more than50% of office visitsSecure message sent to more than 5% of patientsPatients have 2-way communication with the practicePatients can request appointments, prescription refills,referrals and test results
PCMH 2: Team-Based Care2B. Medical Home Responsibilities1.2.3.4. 5. 6. 7. 8.Practice responsible for coordinating careInstructions for obtaining care and advice when office is closedPatients to provide a complete medical history and info aboutcare obtained outside the practiceAccess to evidence-based care, patient education and selfmanagement supportScope of services available, including how behavioral healthneeds are addressedEqual access to all patients regardless of source of paymentGives uninsured patients information about obtaining coverageInstructions on transferring records to the practice
PCMH 3: Population Health Management3D: Use of Data for Population Management1. 2.3.4. 5.2 preventive care services2 immunizations3 chronic/acute care servicesPatients not recently seen by practiceMedication monitoring or alert
PCMH 3: Population Health Management3E. Implement Evidence-Based Decision Support1. Mental health or substance abuse disorder2. Chronic medical condition3. Acute condition4. Condition related to unhealthy behaviors5. Well child or adult care6. Overuse/appropriateness issues
PCMH 4: Care Management and Support4A. Identify patients for care management1. Behavioral health conditions2. High cost/high utilization3. Poorly controlled or complex conditions 4. Social determinants of health 5. Referrals by outside organizations 6. Monitoring the percentage of total patientpopulation identified for care managementand support
PCMH 6: Performance Measurement andQuality Improvement6A: Measure Clinical Quality Performance 1.2.3.4.2 immunization measures2 other preventive measures3 chronic or acute care clinical measuresData stratified for vulnerable populations to assessdisparities in care6B: Measure Resource Use and Care Coordination 1.2.2 measures related to care coordination2 measures affecting health care costs
PCMH 6: Performance Measurement andQuality Improvement6E: Demonstrate Continuous Quality Improvement1. 2. 3. 4.Measuring effectiveness of actionsAchieving improved performance on at least twoclinical quality measuresAchieving improved performance on 1 utilizationor care coordination measureAchieving improved performance on at least onepatient experience measure
Comparison of Must Pass Elements201120141AAccess During Office Hours1APatient-Centered Access2DUse Data for Population Mgmt2DThe Practice Team3CCare Management3DUse Data for Population Mgmt4ASupport Self Care Process4BCare Planning and Self CareSupport5BReferral Tracking and Follow-Up5BReferral Tracking and Follow-up6CImplement Continuous QualityImprovement6DImplement Continuous QualityImprovement
PLANNING FOR THE SURVEY Getting Started Understanding the NCQA PCMH ApplicationProcess Transitioning / Renewal Applications
Getting Started Build your project teamSet a goal/date for completionCommunicate with staffConduct a scored self-assessmentDevelop action plan with short term goals and timelinesBuild the Document LibraryUse a tracking sheet to monitor progress
Access and Utilize NCQA’s ResourcesTools, Resources, Materialswww.ncqa.org/recognition PCMH Standards and Guidelines (most current version)Self-Assessment tool (for baseline scoring)NCQA Training available on-lineNCQA On-line Application & Web-based ISS Survey Tool
If you are NCQA Recognized under the2008 standards Upgrade to the 2011 standards Purchase your ISS tool and application tool NOW Deadline for submission under 2011 standards is March 31, 2015. NCQA’s Advice: Avoid the rush– submit by December 31, 2014 Some grant programs require recognition by November 2014. Review the 2011 standards. If you have held the gains achieved through the preparation of the2008 application, you should be able to start preparing your 2011application.
Transitioning from 2011 to 2014 StandardsMarch 31, 2015Last day tosubmit a 2011Survey ToolMarch 20142014 StandardsReleasedJune 30, 2014Last day topurchase2011 SurveyTool
For Renewal Practices Streamlined approach for practices recognizedunder 2008 standards with Level 2 and 3 statusCan attest to 16 of the 39 elements!Score each factor/element, and write an attestationstatement:“XYZ Clinic previously achieved Level 3 recognition as a PCMH and atteststhat the responses to the factors for this element reflect the currentoperations of the practice site and the documentation to support theseresponses can be provided upon request.”
16 Elements for Attestations2011 NCQA PCMH Standards1A. Access During Office Hours4B. Referrals to Community Resources1B. After-hours Access5A. Test Tracking and Follow-up1D. Continuity5B. Referral Tracking and Follow-up1E. Medical Home Responsibilities6A. Measure Performance1F. Culturally & LinguisticallyAppropriate Services6B. Measure Patient Experience2A. Patient Information6D. Demonstrate Continuous QualityImprovement2B. Clinical Data6E. Report Performance3E. E-Prescribing6F. Report Data Externally
Conduct a Scored Self-AssessmentSummary Statistics - Total Score (scores will automatically calculate)StandardPCMH 1:Enhance Access andContinuityPCMH 2:Identify and Manage PatientPopulationsPCMH 3:Plan and Manage CarePCMH 4:Provide Self-Care Supportand Community ResourcesPCMH 5:Track and Coordinate CarePCMH 6:Measure and ImprovePerformanceElement (total points possible)Points**A: Access During Office Hours (4)0B: After-Hours Access (4)0C: Electronic Access (2)0D: Continuity (2)0E: Medical Home Responsibilities (2)0F: Culturally and Linguistically Appropriate Services (2)0G: The Practice Team (4)0A: Patient Information (3)0B: Clinical Data (4)0C: Comprehensive Health Assessment (4)0**D: Use Data for Population Management (5)0A: Implement Evidence-Based Guidelines (4)0B: Identify High-Risk Patients (3)0**C: Care Management (4)0D: Medication Management (3)0E: Use Electronic Prescribing (3)0**A: Support Self-Care Process (6)0B: Provide Referrals to Community Resources (3)0A: Test Tracking and Follow-Up (6)0**B: Referral Tracking and Follow-Up (6)0C: Coordinate With Facilities and Manage Care Transitions (6)0A: Measure Performance (4)0B: Measure Patient/Family Experience (4)0**C: Implement Continuous Quality Improvement (4)0D: Demonstrate Continuous Quality Improvement (3)0E: Report Performance (3)0F: Report Data Externally (2)0G: Use Certified EHR Technology (2)NATotal Score# MPE Passed at 50%Level of Recognition00NoneSummary Statistics - Must Pass Elements ScorePointsneeded PassedMust PassPointStandardtoat 50%?Elementsspass at (Yes/No)50%PCMH 1: Enhance**A: Access During02NOAccess andOffice HoursContinuityPCMH 2: Identify**D: Use Data forand PCMH 3: Plan and**C: Care Management02NOManage CarePCMH 4: ProvideSelf-Care Support **A: Support Self-Care03NOand Community ProcessResourcesPCMH 5: Track**B: Referral Tracking03NOand Coordinateand Follow-UpCarePCMH 6: Measure **C: ImplementContinuous Quality02NOand ImproveImprovementPerformance
Set a Goal for Submissionand a Realistic Project Timeline
Types of Supporting Documentation Documented Process Reports Formal organizational documentation that describes what you do, such aswritten policy, procedure, protocol, workflowMust be dated and in place for 3 monthsAggregated and site-specific data showing evidence of actionTrended data, graphical presentationsData must be less than 1 year old; label all parts of graphics carefullyRecords or Files DE-IDENTIFY!Actual patient records, files or registry/log entriesScreenshots from EHR, website or other Materials Information given to patients, staff or clinicians, such as self-management oreducational resources, guidelines, letters, emails, meeting minutes
Before Submission, revisit the SelfAssessment Tool What can you reasonably accomplish by yourdeadline ?Can you get maximum points for all elements andfactors ?Do we meet all the Critical Factors and Must Passelements ? If not, why not ?Understand where you can sacrifice points.
NCQA PCMH 1: ENHANCE ACCESS AND CONTINUITYElement (total points possible)**A: Access During OfficeHours (4)Points3STRENGTHSWEAKNESSESCAN WE MAXIMIZE THE POINTS?Triage protocolCall logs to demonstrate response time toNo. Must produce the triageSame Day Appts for eachclinical advice callsproviderprotocol, call logs, and use of phoneDocumentation of clinical advice in theAppointment scheduling policynotes to be solid at 3 points.patient's medical record (use of phone notes)No Patient PortalB: After-Hours Access (4)2Extended clinic hoursAnswering service availabilityCall logs to demonstrate response time toclinical advice calls after hours, and alsoYes, if call logs demonstrate responsethorough documentation of advice given aftertimes and full documentation.hours.Bonni to complete the logs with a chart review.C: Electronic Access (2)0NoneNo Patient PortalD: Continuity (2)2Empanelment PolicyCentricity data field for PCPContinuity of Care ReportsEmpanelment protocols not fully in place, but Yes.will not impede application.E: Medical HomeResponsibilities (2)0NoneF: Culturally andLinguistically AppropriateServices (2)2G: The Practice Team (4)3No Patient Brochure which explains the rolesand responsibilities of a PCMHNo. We do not have an active PatientPortalNo. There is no time to prepare andprint a Patient Brochure.Assessment of Racial and Ethnicbreakdown of patientpopulationAssessment of , and languageNoneYesneeds of patient populationInterpretation servicesPrint materials in otherlanguagesTeam diagramTeams are a bit weak, but starting to gel; willHuddles documentationnot impact the application. Trainings are weakWeds clinical team meetingsin that they have not been provided to all team No. There is not time to train staffStanding Ordersmembers, but can be further developed; will and implement self managementTrainings on communication;not impact the application. Involvement in QI support for all clinical support staff.population mangement; careweak, but can be represented throughcoordinationBEACON and pap projects.Teams involved in QI
TIPS AND TRAPS from a Reviewer’s perspective
1A: Access during Office HoursFactor 3: Providing timely clinical advice by secure electronicmessages during office hours1B: After Hours AccessFactor 4: Providing timely clinical advice during secureelectronic messages when the office is not open “Interactive electronic system” means that someonewill monitor incoming messages and respond in realtime. A turnaround time for response to messages of 24or 72 hours does not meet the definition of“interactive”.
1E: Medical Home ResponsibilitiesThe practice has a process and materials that it providespatients/families on the role of the medical homeFactors 1-4: coordinating care, obtaining care and advice duringoffice hours and when the office is closed, patients must provide acomplete medical history and information about care obtained outsidethe practice, care team provides evidence-based care and selfmanagement support You must submit a documented process for how youprovide printed materials to patients about themedical home as well as the brochure/materialsthat are given to patients.
1G – Team Structure and Roles Job Descriptions should reflect a team approach tocare delivery. Example: “Each team member plays an integralrole in providing patient-centered healthcare. Ourmodel uses the parallel workflow design whereworkload is distributed throughout the team, thusimproving efficiency resulting in better workflowand improved patient an staff satisfaction.”
Care Team Diagram
2C: Comprehensive Health AssessmentFactors 1-9: age/gender appropriate immunizations and screenings; familysocial and cultural characteristics, communication needs, medical history,advance care planning, behaviors affecting health, mental health/substanceabuse, developmental screening (peds), depression screening tool Submit a documented process and a completedhealth assessment Must use screenshots from the SAME patient for allfactors Rationale: Using screenshots from different patientsdoes not demonstrate a PROCESS
2D: Use Data for Population MgmtFactor 4- Specific Medications Intent: Ability to pull lists of patients on specificmedications for purposes of clinical care and/orpatient safety. Submit list of patients on the medication of yourchoice, and also an example of an outreach letterabout the medication. Can’t just say “We’ve never had a recall situation.” Be proactive and prepare a letter to be used incase of a recall or notice of newly known adverseside effects
3: Plan and Manage CareElement A: Implement Evidence-Based GuidelinesFactors 1-3: First important condition; second important condition; third condition related tounhealthy behaviors or mental health or substance abuse. Important conditions do not have to be the most frequently seen, but they are diagnoses, not treatment protocols or screeningMust provide BOTH source of guidelines and evidence ofimplementationDo not use one guideline to cover two conditions (such as DM and HTN)EHR templates for chronic disease care are acceptable as evidenceof implementing EBGScreenshots must be of real patientsAll screenshots illustrating implementation of EBG should come fromthe same patient
6E – Report PerformanceFactor 1- within the practice, results by individual clinicianFactor 2- Within the practice, results across the practice These factors REQUIRE reporting examples from themeasures provided in both: 6A (clinical measures) and 6B (patient satisfaction survey data)
Is your EMR Vendor Pre-Validated? Athena HealthCerner : Power ChartConnexin : Office Programs/RecognitionGE nway : PrimePrevalidationProgram.aspxHealthFusion : MediTouchWebsite accessed May 7 2014i2iSystems : i2iTracksM3 InformationMDLand : iClinicMDDatacor : MDInsightPatientPointPhytel : Insight, Outreach, CoordinatePhysician Hub: Electronic Medical OfficeVitera Healthcare Solutions: Vitera Intergy
Questions and Thank You!!!
2008 standards Upgrade to the 2011 standards Purchase your ISS tool and application tool NOW Deadline for submission under 2011 standards is March 31, 2015. NCQA's Advice: Avoid the rush- submit by December 31, 2014 Some grant programs require recognition by November 2014. Review the 2011 standards.