Transcription
In the name of GodPanelof:Antimicrobialsensitivity tests , control andpreventionPerformance ofStandards forAntimicrobialSusceptibilityTesting (AST)CLSI2016Presented by; M. Hakemi-ValaAssociate Prof of SBMU
Introduction Heavily information from the microbiologylaboratory causes challenge for clinicians.Over time, a microorganism’s susceptibility toan antimicrobial agent may decrease,resulting in a lack of clinical efficacy hods and QC parameters may be refinedto ensure more accurate and betterperformance of antibiotic susceptibility testmethods (CLSI).
Cont’d Infectionsneed to be treated quickly tokeep them from spreading, especially incritical cases such as blood infections. But bacteria are constantly mutating andachievingresistancetoantibiotics,making it harder for medical personnel torespond in time with the right drugs.
Cont’d Empiricaltherapy, is used when: No enough time to AST. This means probable antibiotics resistanceis assessed on the basis of the populationthe patient belongs to – for instance acountry's general public. The next tactic is: to treat the patient withbroad spectrum antibiotics. But these are less effective than targetedantibiotics and their use can contribute toantibiotic resistance.
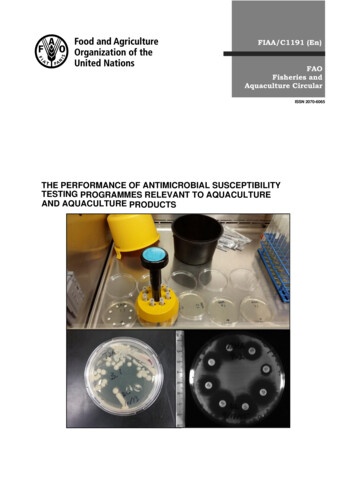
STANDARDIZATION For laboratory tests to accurately determineorganism based resistances, the potentialinfluence of environmental factors onantibiotic activity should be minimized. So,need to:Optimizes bacterial growth conditions Optimizesconditionsformaintainingantimicrobial integrity and activity Maintains reproducibility and consistency inthe resistance profile of an organism
Cont’d Earlyand accurate recognition of resistantbacteria significantly aids the selection ofantimicrobial therapy and optimal patientmanagement. Thus: Invitro AST provides valuable data thatare used in conjunction with otherdiagnostic information to guide patienttherapeutic options.
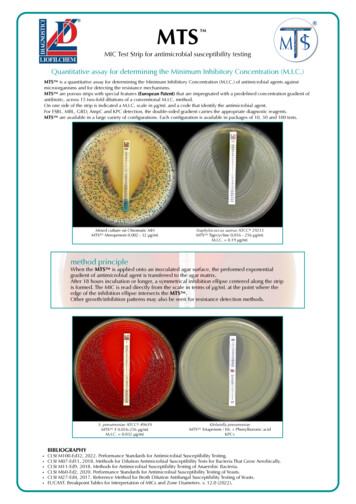
Direct measures of antimicrobialactivity are accomplished using: Conventionalsusceptibilitytestingmethods such as: dilution (broth, agar ),and disk diffusion. Commercialsusceptibility testing systems(E-TEST, Automated methods). Specialscreens and indicator tests.(CATreagent kit)
Standard methods forantimicrobial sensitivity testing AST methods; are in vitro procedures used todetect antimicrobial resistance in individualbacterial blishedforeachpathogen-antibioticcombination indicating at what level of Abagainst the isolate should be considered to use S,I or R.The interpretative criteria for these are based onextensive studies that correlate laboratoryresistance data with serum achievable levels foreach antimicrobial agent and a history ofsuccessfulandunsuccessfultherapeuticoutcomes.
Cont’d Standard conditions for these assays havebeen established based on extensivebatteries of laboratory testing.Guidelines and recommendations for theseare continuously updated by certainorganizations worldwide, such as CLSI,EUCAST, OIE (is reference organizationfor standards relating to animal health andzoonosis),BSAC(BritishSocietyForAntimicrobial Chemotherapy), SFM (CaliforniaReferenced Standards Code), SRGA (theSwedish Reference Group for Antibiotics ) andAustralia ).
Lab approaches and strategies Some points toconsider when deciding whether or not toconduct an AST: Clinical relevance of the isolatePurity of the isolateLogical panel of antimicrobial agents to be tested (i.e.,do not include antibiotics to which the isolate is knownto have intrinsic resistance)Availability of test methodology, resources, and trainedpersonnelStandardization of testingValid interpretation of resultsCost efficiencyEffective means to communicate results andinterpretation to end-users.
Aspects of quality control Onecritical aspect is following standardizedprocedures that can generate reproducibleresults, i.e. quality control. QC includes: Standardized bacterial inoculum size culture(St0.5McFarland;1.5x108 CFU/mL) Conditions(growth medium, pH,cationconcentration Blood and serum supplements and thymidinecontent) Incubation conditions (atmosphere, temperature,duration) Concentration of antimicrobials for testing. Site of Infection(eg; NTF and UT not other sites)
Test Methods in Detecting AntimicrobialResistance Dilution method; broth (Agar/Broth) and(Macrodilution /Microdilution]Disk-diffusion method (Kirby-Bauer method)E-test strip methodAutomatedResistant Mechanism-specific tests: (e.g: βlactamase detection test and chromogeniccephalosporin test)Genotypic methods: such as PCR and DNAhybridization methods
MIC MIC, values determined as described in M07-A10 maybe reported directly to clinicians for patient carepurposes.The MIC obtained using a dilution test may tell aphysician the concentration of antimicrobial agentrequired at the site of infection to inhibit the infectingorganism. However, the MIC does not represent anabsolute value.It is essential that an interpretive category result (S, I, or R)also be provided routinely to facilitate understanding ofthe MIC report by clinicians.In place of interpretive criteria (“breakpoints” or “clinicalbreakpoints”) an epidemiological cutoff value (ECV)may be listed for specific organism/ antimicrobial agentcombinations.
Cont’d1- Dilution methodsMIC determinationAgardilutionMicro brothDilution(0.05-0.1ml)Macrobrothdilution(1ml)
Notes The Ab concentration range may be basedon; the level of drug required to reliablydetect a particular resistance mechanism.In this case, the test concentration for a drugmay vary depending on the organism and itsassociated resistances.For example, to detect clinically significantresistance to cefotaxime in S. pneumoniae,the dilution scheme uses a maximumconcentration of 2 µg/mL; however, to detectcefotaxime resistance in E. coli, the requiredmaximum concentration is 16 µg/mL orhigher.
Inoculation in microdilution ifthe volume of broth in the well is 0.1 mLand the inoculum volume is 0.01 mL, thenthe 0.5 McFarland suspension (1 108CFU/mL) should be diluted 1:20 to yield 5 106 CFU/mL. When 0.01 mL of this suspension is inoculatedinto the broth, the final test concentration ofbacteria is approximately 5 105 CFU/mL (or5 104 CFU/well in the microdilutionmethod).
Inoculation in macrodilution Dilutingthe 0.5 McFarland suspension 1:150,resulting in a tube containing approximately1 106 CFU/mL. The subsequent 1:2 dilution in step 3 bringsthe final inoculum to 5 105 CFU/mL
A. Bacterial growth profiles in a broth microdilutiontray. The wells containing the lowest concentration of anantibiotic that completely inhibits visible growth (arrow)are recorded in micrograms per milliliter (µg/mL) as(MIC).
2- Disk diffusion method Becauseof convenience, efficiency and cost, thedisk diffusion method is probably the most widelyused method for determining antimicrobialresistance method. Included of: Mueller-Hinton agar(MHA) Bacterial lawn of inoculation: approximately 1 to 2 x108 CFUs/ ml Zone diameter of inhibition Results: S,I,R Note: MIC measurement cannot be determinedfrom this qualitative test.
A, Disk diffusion method: antibiotic disks are placed on the agarsurface just after inoculation of the surface with the test organism. B,Zones of growth inhibition around various disks are apparent after 16to 18 hours of incubation.
Reading and Interpretation ofResults The plate is examined to confirm that a confluent lawn of growthhas been obtained.If growth between inhibitory zones around each disk is poor andnonconfluent, the test should not be interpreted and should berepeated.The lack of confluent growth may be due to insufficient inoculum.Alternatively, a particular isolate may have undergone mutation,and growth factors supplied by the standard medium are no longersufficient to support robust growth.In the latter case, medium supplemented with blood and/orincubation in CO2 may enhance growth.Plates should also be examined for purity.
Instructions for Use of Tables Tables1A and 1B in CLSI —Suggestedgroupings of antimicrobial agents thatshould be considered for routine testingand reporting by clinical microbiologylaboratories. For each organism group, an additionaltable (Tables 2A through 2I) contains:
Selecting Antimicrobial Agentsfor Testing and Reporting Selectionof the most appropriateantimicrobial agents to test and to reportis based on the: Adecision best made by eachlaboratory in consultation with theinfectious diseases practitioners and thepharmacy. The recommendations for each organismgroup include agents of proven efficacy.
Cont’d Drugslisted together in a single box areagents for which interpretive results (S, I, orR) and clinical efficacy are similar. Within each box, an “or” betweenagents indicates those agents for whichcross-resistance and cross-susceptibilityare nearly complete. EX; cefotaxime S ceftriaxon S
Test/Report Groups Agents in Group A: are appropriate for inclusion in a routine,primary testing panel, as well as for routine.Agents in Group B: are may warrant primary testing, but theymay be reported only selectively, such as when the organism isresistant to agents of the same antimicrobial class, as in GroupA.Selected specimen source (eg, a 3th-generation cephalosporinfor enteric bacilli from CSF or SXT for UT isolates);A polymicrobial infection,Infections involving multiple sites,Cases of patient allergy or intolerance,Failure to respond to an antimicrobial agent in Group A;For purposes of infection control.
Cont’d Group C; includes alternative or supplementalantimicrobial agents that may necessitatetesting in those institutions that harborendemic or epidemic strains resistant toseveral of the primary drugs (especially in thesame class, eg, β-lactams);Treatment of patients allergic to primary drugsTreatmentof unusual organisms (eg;chloramphenicol for extra-intestinal isolates ofSalmonella spp).
Cont’dU (“urine”), includes certain antimicrobialagents (eg, NTF and certain quinolones) that areused only or primarily for treating urinary tractinfections (UTIs). These agents should not be routinely reportedagainst pathogens recovered from other sites. Group
Cont’d GroupO (“other”) includes agents with clinicalindication for the organism group but are generallynot candidates for routine testing and reporting . ial agents that are investigational for theorganism group and have not yet been approved bythe FDA.
Reporting Results It is essential that an interpretive categoryresult (S, I, or R) also be provided routinelyto facilitate understanding of the MICreport and zone diameter by clinicians.Zone diameter measurements without aninterpretive category should not bereported.
Susceptible (S) Dose S;dependentImplies that isolatesare inhibited by the usuallysusceptible(DDS)achievable concentrations of antimicrobial agent. DDS;NOTE: The SDD interpretation is a newcategory for antibacterial susceptibility testing,although it has been previously applied forinterpretation of antifungal susceptibility test results. Implies that susceptibility of an isolate is dependenton the dosing regimen that is used in the patient.The concept of SDD has been included within theintermediate category definition for antimicrobialagents.
Intermediate Theconcept of SDD has been includedwithintheintermediatecategorydefinition for antimicrobial agents. This category also includes a buffer zone,which should prevent small, uncontrolled,technical factors from causing majordiscrepancies in interpretations, especiallyfor drugs with narrow pharmacotoxicitymargins.
Resistant (R) The“resistant” category implies thatisolates are not inhibited by the usuallyachievable concentrations of the agentwith normal dosage schedules and/orthat demonstrate MICs or zone diametersthat fall in the range.
Nonsusceptible (NS) NS,is used for isolates for which only asusceptible interpretive criterion has beendesignated because of the absence orrare occurrence of resistant strains. Does not necessarily mean that theisolate has a resistance mechanism. For these strains , organism identificationand AST results should be confirmed.
Cont’d
Some changes in CLSI tables Deleted from Tables 1A, 1B, and/or 1C ,quinupristindalfopristin,spectinomycin, telithromycin, and olozane-tazobactamtoTest/Report Group B.Clarified information for use of cefazolin as asurrogate test for uncomplicated urinary tractinfections (UTIs) in Group U.
Cont’d Pseudomonas aeruginosa:Moved piperacillin-tazobactam to Test/Report Group A.Added ceftolozane-tazobactam to Test/Report Group B.Staphylococcus spp.:Added oritavancin, tedizolid, and telavancin toTest/Report Group B.Enterococcus spp.:Added oritavancin, tedizolid, and telavancin toTest/Report Group B .Acinetobacter spp.:Moved tetracycline to Test/Report Group U .Burkholderia cepacia complex:Moved levofloxacin and meropenem to Test/ReportGroup A.Moved chloramphenicol to Test/Report Group C.
Cont’d Table4B : Added QC ranges for: Haemophilus influenzae ATCC 49247 Delafloxacin Lefamulin Levonadifloxacin
References Bailyand Scott 2014 CLSI 2016 esistance Sciencenordic.com
batteries of laboratory testing. Guidelines and recommendations for these are continuously updated by certain organizations worldwide, such as CLSI, EUCAST, OIE (is reference organization for standards relating to animal health and zoonosis), BSAC (British Society For Antimicrobial Chemotherapy), SFM (California Referenced Standards Code), SRGA .