Transcription
Adjuvant Chemotherapy in BreastCancerElgene Lim, Shom Goel, and Eric P. Winer4 Introduction5The biological rationale for adjuvant systemictherapy is to eradicate micrometastases andtherefore improve patient outcomes. Adjuvantcombination chemotherapy regimens result in asignificant reduction in risk of 5-year recurrenceand 15-year mortality rates, with a greater benefitin women 50 years of age [1]. In the clinicalsetting, the decision to use adjuvant chemotherapy is guided by the clinician’s estimation of thepatient’s prognosis (both her risk of cancer recurrence and overall life expectancy) and assessment of the chemosensitivity of the tumor. Notsurprisingly, the use and choice of adjuvant chemotherapy regimen in clinical practice are highlyvariable. Prognostic determinants of breast cancer recurrence may be broadly divided into thecategories of tumor stage (including both tumorsize and nodal status) and tumor biology (suchas tumor grade, estrogen receptor (ER), progesterone receptor (PR) status, and HER2/neuexpression).It is important to note that the relapse riskfor small tumors is relatively small, and it isimportant to consider the limited benefits in thispatient subgroup in the context of the 829E. Lim, MBBS, FRACP, PhD (*)S. Goel, MBBS, FRACP E.P. Winer, MDDivision of Women’s Cancers, Dana-Farber CancerInstitute, 450 Brookline Ave, Boston, MA 02115, USAe-mail: elgene lim@dfci.harvard.edu12233risks of toxicities with systemic chemotherapy.Substantial progress has been made in our current understanding of the genes involved in breastcancer, with gene profiling techniques c onfirmingthe biological heterogeneity of breast cancer ata molecular level. Researchers have identifiedat least two intrinsic luminal subtypes (luminalA and luminal B) with distinct gene expression,a basal-like subtype, comprised of primarilytriple- negative breast cancer (TNBC, defined asER negative, PR negative, and HER2/neu negative), and a HER2/neu-positive subtype [2, 3].Broadly speaking, strongly hormone receptor(HR)-positive tumors are considered less chemosensitive than HR-negative breast cancers [4],with the degree of HR positivity thought to correlate with endocrine therapy responsiveness. Assuch, the optimal use of adjuvant chemotherapyin HR-positive breast cancer has become quitecomplex [5]. The identification of the specificsubgroup of patients with HR-positive tumorsthat will benefit the most from adjuvant chemotherapy remains a major challenge to cliniciansat present.Prospective data on the utility on biomarkersto predict chemosensitivity are limited, with themost promising biomarkers likely to be multigene prognostic signatures that are able to capture the multiple biological pathways thatdetermine chemotherapy response. The earlierNational Institute of Health (NIH) clinical guidelines on adjuvant therapy have recommendedchemotherapy for those patients with tumors 1 cm and in the presence of involved nodes [6].A.I. Riker (ed.), Breast Disease: Comprehensive Management,DOI 10.1007/978-1-4939-1145-5 23, Springer Science Business Media New York 5354555657585960616263
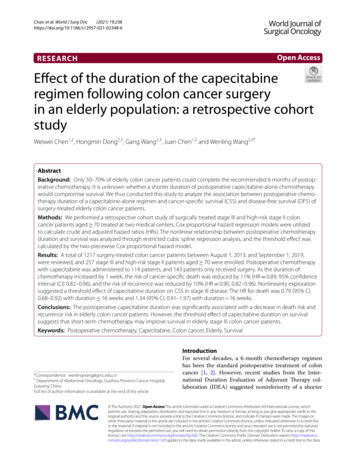
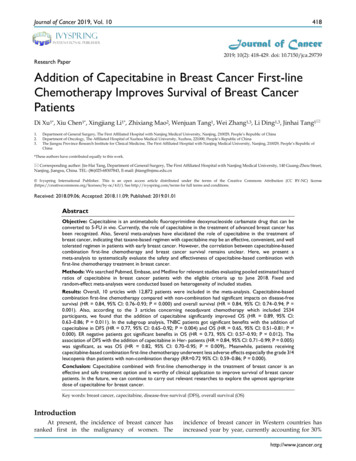
E. Lim et owever, recent advances in our understandingof breast cancer have resulted in several revisionsto these guidelines, taking into account the tumorbiology of breast cancer.This chapter will focus on the use of adjuvant chemotherapy primarily in the HER2/neu- negative subtype of breast cancer. HER2directed therapy will be covered in detail ina separate chapter. The regimens that will bediscussed are used in both the ER-positive andtriple-negative breast cancer (TNBC, defined asER-negative, PR-negative, and HER2/neu-negative) subtypes and in both preoperative (neoadjuvant) and adjuvant settings. Specifically, the useof biomarkers and multigene tests to identify thesubset of patients with HR-positive breast cancer will be discussed in detail. Finally, we willalso discuss special considerations for the use ofadjuvant chemotherapy in the setting of inflammatory breast cancer, elderly, young, and pregnant patients and will conclude with a discussionon the management of chemotherapy-associatedtoxicities.87 Standard Chemotherapy Regimens88The choice of an adjuvant chemotherapy regimenshould take into account the tumor burden andbreast cancer subtype, as the absolute reductionin the risk of recurrence and mortality from adjuvant chemotherapy is dependent upon the baseline risk. There are a number of commonlyutilized adjuvant chemotherapy regimens in clinical practice today (Table 23.1), with most typically given over 4–8 cycles in total. As many ofthese regimens have not been compared head tohead in clinical trials, there is currently no singleuniformly accepted standard adjuvant chemotherapy regimen.Commonly used regimens for breast cancerare summarized in Table 23.1 and can broadly bedivided into:1. Non-anthracycline-containing regimens (i.e.,CMF and TC)2. Anthracycline-containing regimens (i.e., AC,FAC, 3. Anthracycline- and taxane-containing regimenswhich incorporate both anthracyclines and taxanes (i.e., AC T, FEC taxane and TAC)The Early Breast Cancer Trialists’Collaborative Group (EBCTCG) has published alarge meta-analysis of different polychemotherapy regimens used in over 100,000 women from123 randomized trials [1]. The most effectiveadjuvant chemotherapy regimens included bothanthracycline and taxanes, but these were alsoassociated with the highest frequency of toxicity.Overall, the addition of adjuvant chemotherapyreduced breast cancer mortality by about onethird, and the proportional risk reductions in thetrials analyzed were only minimally affected byage, tumor burden (tumor size and nodal status),tumor grade, ER status, or tamoxifen use.A summary of the key findings are as follows [1]: Standard AC (4 cycles) and standard CMF(6 cycles) are equivalent. Anthracycline-based regimens such as FAC orFEC, which have a higher cumulative anthracycline dosage than standard AC (4 cycles),are superior to standard oral CMF (6 cycles). The addition of 4 cycles of a taxane to a fixedanthracycline-based control regimen reducedbreast cancer mortality. However, there wasno significant difference in outcomes when theextra 4 taxane cycles were counterbalancedwith extra cycles of a non-taxane chemotherapy.More recently, results from the large phase IIIrandomized National Surgical Adjuvant Breastand Bowel (NSABP) B-38 trial were reported,comparing the three adjuvant chemotherapy regimens, dose-dense AC T, dose-dense AC Tplus gemcitabine, and TAC, in a large cohort ofapproximately 5,000 patients (65 % with nodalinvolvement and 80 % with ER-positive disease)[20]. The 5-year DFS and overall survival (OS)rates were similar in all three groups; however,the incidence of grade 3 or 4 toxicity was thelowest with the AC T regimen.Another area of variability is the frequencyof administering chemotherapy. Dose-densechemotherapy typically refers to the administration of chemotherapy over a shorter interval.The best example of this is with AC, which 40141142143144145146147148149150151152153154
23 Adjuvant Chemotherapy in Breast Cancer[AU1]t1.1t1.2t1.3Table 23.1Cycle durationNocycles Notesq4 weeks6q3 weeks4q3 weeks4q3 weeks6q4 weeks6q4 weeks6[15]q3 weeks6Filgrastim support[16]should be consideredq2 weeks4 4t1.40t1.41DoseRegimenNon-anthracycline containingCyclophosphamideOral CMF(100 mg/m2, PO) d1 to 14Methotrexate (40 mg/m2) d1, 85-Fluorouracil(500 mg/m2) d1, 8TCDocetaxel (T; 75 mg/m2)Cyclophosphamide(600 mg/m2)Anthracycline containingACDoxorubicin (A; 60 mg/m2)aCyclophosphamide(600 mg/m2)FAC5-Fluorouracil (500 mg/m2)AC (50/500 mg/m2)bCAFCyclophosphamide(600 mg/m2)Doxorubicin (A; 30 mg/m2)bd1, 85-Fluorouracil (500 mg/m2)FEC605-Fluorouracil (500 mg/m2)(Canadian)Epirubicin (60 mg/m2)cCyclophosphamide (75 mg/m2,PO) d1 to14FEC1005-Fluorouracil (500 mg/m2)Epirubicin (100 mg/m2)cCyclophosphamide(500 mg/m2)Anthracycline and taxane containingAC TDose-dense ACa,d Paclitaxel(T; 175 mg/m2)AC Paclitaxel(T; 80 mg/m2)FEC100 DocetaxelFEC100 D(T; 75 mg/m2)FEC100 (T; 100 mg/m2)FEC100 PTACDocetaxel (T; 75 mg/m2)AC (50/500 mg/m2)a, dt1.42t1.43All chemotherapy is given intravenously unless otherwise stated. Cumulative doses a240 mg/m2, b 240 mg/m2,c 300 mg/m2, dGiven with filgrastim support155be administered at the same doses in a standardthree- weekly interval or a dose-dense fashionevery 2 weeks [9, 11]. With treatment administered every 2 weeks, growth factor supportwith filgrastim is required. With dose-dense ACregimens, paclitaxel may be given following ACeither every 2 weeks for 4 cycles or weekly for12 weeks (at 175 mg/m2 and 80 mg/m2, 62q3 weeks weekly 12 4 12Reference[7–9]Nonstandard IVCMF(600/60/600 mg/m2),d1, 8, q4 weeks isoccasionally given[10]Dose-dense AC isgiven q2 weeks withdfilgrastim support[9, 11][12, 13]C may be given POat 100 mg/m2 on d1to 14 of each cycle[14][17][18]q3 weeks3 3[16]q3 weeks weekly 8q3 weeks4 86[19][12]tively), and it is unclear at this point if eitherapproach is associated with improved outcomes.A recent meta-analysis of dose-dense chemotherapy for early breast cancer, which included10 randomized trials involving over 10,000patients, reported a better DFS and OS withdose-dense regimens, particularly in womenwith HR-negative breast cancer [21].163164165166167168169170
E. Lim et 03204205206207208209210211212213214 hemotherapy in Different BreastCCancer SubtypesThe EBCTCG overview reported a benefitin terms of 5-year recurrence-free survival withadjuvant sequential chemoendocrine therapyEndocrine therapy forms the basis of adjuvant over endocrine therapy alone with hazard ratiostherapy in patients with HR-positive breast can- of 0.64 and 0.85 in patients with ER-positivecer, and the addition of chemotherapy benefits a tumors aged 50 and 50 years, respectivelysubset of these patients. In patients with HER2/ [27]. The larger impact of chemotherapy inneu-positive tumors, HER2-directed therapy younger patients may be partially explained byalone has not been tested in large adjuvant trials, the endocrine effect of chemotherapy on ovarand the addition of chemotherapy to HER2- ian function [6]. Similar long-term DFS benefitsdirected therapy is considered to be the current with the addition of chemotherapy to adjuvantstandard of care in the United States. Finally, for endocrine therapy were also noted in the phaseTNBC, there are no targeted therapies recom- III randomized NSABP B-20 and Southwestmended for use outside of a clinical trial in the Oncology Group (SWOG) 8814 trials [26, 28].adjuvant setting, again with combination chemo- The identification of predictors of chemosensitivtherapy recognized as the standard of care.ity in HR-positive tumors has been identified asa key challenge.There is evidence suggesting an inverse rela Chemotherapy in Hormonetionship between HR expression and chemotherReceptor- Positive Breast Cancerapy benefit in luminal breast cancers. In a studyof postmenopausal women with ER-positive andWhile adjuvant endocrine therapy is the standard node-positive cancers from the Internationalof care in patients with tumors that express HRs, Breast Cancer Study Group (IBCSG) Trials VIIthe indication for adjuvant chemotherapy in and 12-93, the addition of adjuvant chemotherpatients with HR-positive disease is undergoing apy to endocrine therapy improved the DFS (hazreevaluation. Adjuvant chemotherapy is typically ard ratio 0.81, p 0.02, median follow-up ofgiven in sequence with, and prior to, endocrine 13 years) [29]. Nonparametric subpopulationtherapy, as there have been conflicting outcomes treatment effect pattern plot (STEPP) analyseswith concurrent therapy [22–24]. On average, demonstrated that this benefit was limited to thepatients with HR-positive breast cancers derive patients whose tumors had low to intermediateless benefit from chemotherapy compared to levels of estrogen expression. The level of ERHR-negative tumors [25]. However, there still appears to predict the response to both endocrineappears to be a subset of patients with HR-positive and chemotherapies in opposite directions, buttumors that are chemosensitive. The basis for the these factors may not entirely overlap. It is likelyaddition of chemotherapy to adjuvant endocrine that there are other biological factors that interacttherapy is usually guided by the clinician’s esti- with the ER-signaling pathway to determine chemation of prognosis and assessment of the endo- mosensitivity. The assumption that chemosensicrine- and chemosensitivity of the tumor. Patients tivity is inversely related to endocrine sensitivityfor whom systemic chemotherapy should be in ER-positive breast cancer is therefore notstrongly considered include patients with grade 2 clearly defined. Tumors that are endocrine sensior 3 disease, those with high-risk features based tive may also be chemosensitive; conversely,upon the gene signature (such as Oncotype DX endocrine resistant tumors with poor prognosticand MammaPrint), and patients with a higher dis- factors may not always be chemosensitive.ease burden. That said, not every patient withOne biomarker that has been examined in chenode-positive disease has to be treated with che- mosensitive ER-positive tumors is Ki67, a markermotherapy, and multigene signatures are particu- of cellular proliferation. In an analysis of 1,521larly useful in guiding the clinicians in regards to premenopausal and postmenopausal patientsthe decision to recommend chemotherapy [26].with ER-positive tumors from the IBCSG 247248249250251252253254255256257258259260261262
23 Adjuvant Chemotherapy in Breast and IX trials, respectively, a high Ki67 index wasfound to be associated with poorer DFS, but didnot predict an OS benefit with the addition ofchemotherapy to endocrine therapy [30]. Theadjuvant chemotherapy used in these trials wasCMF and did not include anthracyclines and taxanes. In contrast, a high Ki67 index was predictive of both outcome and benefit to adjuvanttaxane chemotherapy in ER-positive breast cancers in subset analyses of the PACS 01 and BreastCancer International Research Group (BCIRG)001 trials [31, 32]. An important caveat of thesefindings is that these were unplanned subset analyses. At this point, Ki67 should not be used as abasis of recommendation for adjuvant chemotherapy outside of a clinical trial setting, at leastin part because the test is not always reliable.A major advancement in the identification ofbiomarkers of chemosensitivity in HR-positivebreast cancers has been the development of multigene prognostic signatures. These are typicallyderived from high-throughput analyses of tumorspecimens for gene expression patterns andsubsequently validated in patient cohorts fromclinical trials. These assays have the potentialto identify subsets of patients that would benefit from the addition of adjuvant chemotherapyto endocrine therapy. The 21-gene assay, calledthe Oncotype DX (Genomic Health, RedwoodCity, CA, USA), provides a recurrence score(RS) that predicts for risk of 10-year distantrecurrence. The RS is derived from a complexalgorithm calculated on the gene expressionsof a preselected list of 16 genes of biologicalinterest, including genes involved in estrogensignaling, cell proliferation, and HER2/neu signaling and 5 reference genes for normalizationpurposes [28]. The utility of the RS as a predictor of distant recurrence risk at 10 years wasinitially assessed in the NSABP B-14 trial, inwhich patients with ER-positive, node-negativebreast cancer were randomized to receive eithertamoxifen or placebo. The RS was shown tomore accurately predict for distant recurrencethan conventional clinicopathologic characteristics in the tamoxifen- treated patients [33].The utility of the RS to accurately predict10-year distance recurrences was demonstratedin a retrospective analysis of the NSABP B-20trial, in which patients with ER-positive, node- negative breast cancer were randomized to eithertamoxifen or tamoxifen plus chemotherapy.Patients with a low or intermediate RS (defined as 18, and 18 and 31, respectively) were foundnot to benefit from chemotherapy, while thosewith a high RS (defined as 31) derived a significant benefit from chemotherapy [28]. The absolute difference in the 10-year distant recurrencerates with the addition of chemotherapy in theseRS groups was an increase of 1.1 % and 1.8 %and a reduction of 28.6 %, respectively. Similarresults were obtained in a retrospective analysisof the SWOG 8814 trial, in which postmenopausal patients with ER-positive, node- positivebreast cancer were randomized to receive eithertamoxifen or tamoxifen plus anthracycline- basedchemotherapy [26]. One of the primary strengthsof this assay is that RNA may be extracted fromarchived formalin-fixed, paraffin- embedded tissue, which is the primary mode of preserving tissue in most pathology departments.Another multigene signature with prognosticutility is the FDA-approved 70-gene MammaPrintsignature (Agendia, Amsterdam, Netherlands).Unlike the Oncotype RS assay where genes arepreselected, MammaPrint was developed usingan unsupervised hierarchical clustering approachwhereby the high-risk gene signature predicted apoor clinical outcome in tumors of all subtypes[34]. A retrospective analysis of pooled patientcohorts with ER-positive, node-negative breastcancer demonstrated that the 70-gene score hadprognostic value and predicted improved survivaloutcomes with the addition of chemotherapy toendocrine therapy only in the subgroup of70-gene high-risk patients [35].While both the Oncotype and MammaPrintassays were tested retrospectively, the OncotypeRS was evaluated retrospectively in a prospectively assembled clinical trial. For this reason,there is far greater confidence, at this time,that the Oncotype assay can reliably predictwhich patients will benefit from chemotherapy,and even more importantly, which ones willnot. In addition, unlike the Oncotype assay,MammaPrint is performed on 55356357358
E. Lim et 91392393394395396397398399400401402403404405406t issue that may limit its feasibility for routineuse. Both of these multigene signatures are currently undergoing prospective validation in largeongoing studies (Oncotype RS, TAILORx andRxPONDER trials; MammaPrint, MINDACTtrial), which include over 100,000 patients collectively to definitively address their predictivevalue for chemosensitivity in ER-positive breastcancer [36, 37].In considering the benefits of adjuvant chemotherapy in patients with HR-positive tumors, it isimportant to consider common relapse patterns.Patients with HR-positive tumors are at a continued risk of relapse for many years after initialbreast cancer diagnosis [38]. More than half of allrecurrences among women treated with adjuvanttamoxifen therapy occur between 6 and 15 yearsafter diagnosis, and the greatest benefit with theaddition of chemotherapy in DFS was seen primarily within the first 5 years from diagnosis [27].The limited benefit from chemotherapy in preventing late relapses is also reflected in the DFSpatterns of patients with poor prognosis multigene signatures with both the Oncotype RS andMammaPrint assays [28, 39]. Late recurrencesand deaths remain a formidable clinical challengein HR-positive breast cancer, and chemotherapyis unlikely to be the answer to this problem.The summary recommendations for adjuvantchemotherapy in hormone receptor-positivebreast cancer are as follows: Adjuvant chemotherapy should be stronglyconsidered in the setting of node-positive disease, high-grade tumors, and high-risk genemultigene signatures. In regard to the utility of the Oncotype DXRecurrence Score:–– The use of Oncotype for node-positive disease is discouraged in poorer prognosisdisease, for example, 4 positive nodes, orin the setting of high- grade disease, as chemotherapy should routinely be given inthese settings.–– The use of chemotherapy is stronglyencouraged in patients with Oncotype RS 31.–– In node-positive patients, particularlythose with one to three positive nodes,c onsideration can be given to omittingchemotherapy if the Oncotype RS is low( 18) and there are no other unfavorablefeatures.–– Recommendations for patients withintermediate- risk multigene signatures(i.e., Oncotype RS 18-31) are an area ofcontroversy and active research, and prospective trials in this population are currently underway [36, 37].407408409410411412413414415416 hemotherapy in HER2-PositiveCBreast Cancer417The advent of HER2-directed therapy has revolutionized the management of HER2/neu-positive,early-stage breast cancer. Based on the resultsof five randomized clinical trials, 12 months ofadjuvant trastuzumab is now an integral part ofsystemic therapy for these patients [40–42]. Inall studies, trastuzumab was added to a chemotherapy backbone, and there is currently no datato support the use of adjuvant trastuzumab monotherapy. Evidence-based chemotherapy backbones in this context include AC T (NSABPB-31, NCCTG N9831), AC docetaxel (BCIRG006) and docetaxel carboplatin (BCIRG 006).Given the increased cardiotoxicity risk uponadministering trastuzumab concurrently withan anthracycline in the metastatic setting [43],trastuzumab is omitted during the period ofanthracycline chemotherapy.There remains controversy about the treatmentof small HER2/neu-positive cancers. There arelimited data on outcomes for patients with small,stage I HER2/neu-positive breast cancers becausethe seminal adjuvant trastuzumab trials excludedpatients with these tumors. Current guidelinesfrom St. Gallen and the European Society forMedical Oncology (ESMO) do not recommend adjuvant trastuzumab and chemotherapyfor node-negative HER2/neu-positive tumorsthat are 1 cm [44]. In contrast, the NationalComprehensive Cancer Network (NCCN) treatment guidelines have factored in the indirectevidence obtained from retrospective and subsetanalyses of trials and recommend 447448449450451
23 Adjuvant Chemotherapy in Breast Cancer Preoperative Chemotherapy(Neoadjuvant)489Most early systemic chemotherapy trials foroperable breast cancer were conducted in theadjuvant setting, with the use of preoperative(neoadjuvant) chemotherapy limited primarily toinflammatory and locally advanced breast cancer.The original rationale for neoadjuvant chemotherapy (NAC) was to render locally advancedtumors operable by shrinking the diameter ofthese tumors, thereby reducing the extent of surgery required in operable breast cancer. Studiescomparing the adjuvant and NAC approacheshave found the survival to be equivalent whenusing identical systemic agents (Table 23.2).These trials also demonstrated that patients whoachieved a pathological complete response (pCR)following NAC had improved clinical outcomescompared to patients who did not.The NAC and adjuvant chemotherapy regimens used clinically are identical. The NACapproach is now increasingly used in smaller,operable TNBC and HER2/neu-positive tumors,although less commonly with HR-positive tumorsas they are inherently less chemosensitive [4, 50].There has also been a trend by many clinicians toevaluate novel therapies in the preoperative setting. A NAC allows for the study of the biological impact of systemic therapy on pre- andposttreatment tissue and therefore represents afertile setting for tissue-intensive correlativeresearch. The goal of biomarker discovery inNAC clinical trials is to identify surrogate endpoints of clinical outcomes, such as predictivebiomarkers of therapeutic response or resistance.The US Food and Drug Administration (FDA) is491488be given to the use of trastuzumab- based therapyin T1bN0 tumors, in particular, in the hormonereceptor-negative subset [45].However, there is a wide variation in clinicalpractice in this subgroup. Recently, interest hasdeveloped in using less intensive, and thereforepotentially less toxic, partner chemotherapieswith adjuvant trastuzumab for low-risk HER2- positive tumors. In a phase II study in womenwith HER2/neu-positive metastatic breast cancer,weekly paclitaxel and trastuzumab resulted in a67–81 % response rate, and a 6 % incidence ofgrade 3 or 4 neutropenia [46]. The Dana-FarberCancer Institute led a multicenter, phase II, nonrandomized study of weekly paclitaxel plustrastuzumab for 12 weeks, followed by maintenance trastuzumab for a further 9 months inpatients with node-negative, HER2/neu-positivetumors that are 3 cm (information available atClinicalTrials.gov; identifier NCT00542451).This trial has completed accrual of 410 patients,of whom approximately 50 % had tumors 1 cm.If the 3-year DFS is 95 %, the regimen will bedeemed worthy of further investigation. It isexpected that the preliminary results will beavailable in late 2013.The adjuvant therapy of HER2/neu-positivebreast cancer will be discussed in detail in a separate chapter. The summary recommendationsfor systemic adjuvant chemotherapy inHER2/neu-positive breast cancer are as follows: Systemic adjuvant chemotherapy should begiven in combination with trastuzumab, especially in tumors 0.5 cm. Trastuzumab is omitted during the period ofanthracycline chemotherapy but can be givenconcurrently with taxanes.t2.1Table 23.2 Seminal trials comparing neoadjuvant chemotherapy to adjuvant chemotherapy for early-stage breast 83484485486487490Neoadjuvant vs. adjuvant therapyt2.2t2.3t2.4t2.5t2.6t2.7t2.8TrialNSBAP B-18EORTC 10902ECTOpCR rateChemotherapy(%)AC 4133.7FEC60 4AP 4 CMF 3 20pCR vs. non-pCRhazard ratioOS: 0.32†OS: 0.91RFS: 0.43†BCS rates68 % vs. 60 %*35 % vs. 22 %65 % vs. 34 %*DFS HR0.931.121.21OS HR0.991.091.10Reference[47][48][49]BCS breast cancer survival, DFS disease-free survival, OS overall survival, pCR pathological complete responsep 3524
E. Lim et 0541542543544545546547548549550551552considering the possibility of using pCR in theNAC setting as a surrogate end point for clinicalbenefit and as an indication for accelerated drugapproval [51].Practically, NAC should be managed onlyin a multidisciplinary team setting, with initialassessments made by the breast surgeon andmedical and radiation oncologists. Evaluationof treatment response to NAC could potentiallyallow the treating team to tailor individual treatment based upon tumor response, particularly ifthere is the suggestion of disease progression.There have been two trials in which patients wererandomized mid-treatment to non-cross-resistantchemotherapy regimens according to their mid- treatment response [52, 53]. In both trials, deviating from the initial course of therapy in clinicalnonresponders did not increase either the clinicalor pathological response rates or improve survival. For operable breast cancer, in the event ofdisease progression mid-NAC, we would recommend an immediate reevaluation by the breastsurgeon in order to assess the feasibility of surgical resection with mastectomy. Decisions aboutadditional chemotherapy can be deferred until theadjuvant setting. For patients with non- resectabledisease, radiation or alternative i nvestigationalapproaches should be considered [54].553 Special Clinical Scenarios554I nflammatory and Locally AdvancedBreast flammatory breast cancer (IBC) represents aunique biological entity characterized by distinctclinical and histopathological features, aggressivebehavior, and an exceptionally poor prognosis(median survival with current therapy 4 years)[55]. The current standard of care for management of stage 3B IBC is a multimodality approachconsisting of NAC followed by surgery and radiotherapy. Achieving a pCR to NAC is the singlemost important prognostic factor in IBC [56, 57].Given the relative rarity of IBC, there havebeen no specific randomized trials examining theoptimal NAC regimen, and moreover patientswith IBC have historically been excluded fromNAC systemic therapy studies due to their poorprognosis. Single-arm studies and retrospectivecase series show that anthracycline-based regimens are effective (clinical response rates around70 %) [56] and that their efficacy is enhanced bythe subsequent addition of a taxane as evidencedby increased clinical and pCR rates [58, 59]. Assuch, regimens included in the “Anthracycline andTaxane” section of Table 23.1 are recommended.Although outside the scope of this chapter, itis noteworthy that approximately 40 % of IBCare HER2/neu positive, and evidence from randomized phase 3 clinical trials strongly supportsthe routine addition of trastuzumab to NAC inthis setting [60].5
uniformly accepted standard adjuvant chemo-therapy regimen. Commonly used regimens for breast cancer are summarized in Table 23.1 and can broadly be divided into: 1. Non-anthracycline-containing regimens (i.e., CMF and TC) 2. Anthracycline-containing regimens (i.e., AC, FAC, FEC) 3. Anthracycline- and taxane-containing regimens