Transcription
Monitoring Medicaid ManagedCarePresented By:Navigant Healthcare - Cheryl Duva and Tamyra Porter andThe Commonwealth of Pennsylvania – Barbara Molnar
AgendaNavigant Health Care OverviewThe Importance of Monitoring – Making the CaseThe Changing Landscape of MedicaidIntegration and Coordination
Monitoring Medicaid Managed CareNAVIGANT HEALTHCARENAVIGANT HEALTHCARE OVERVIEW
Who is Navigant Healthcare?30 years Global Consulting Firm2,500 professionals located in over 45 U.S. / Global Based OfficesKey Health Care Practice Areas:Health Care: 500 consulting professionals and industry thought leaders Payer Provider Performance Improvement Life SciencesOur ClientsFederal and State Government AgenciesHealth PlansHealth Systems and PhysiciansPharmacy Benefit Managers (PBMs)
Monitoring Medicaid Managed CareMAKING THE CASEWHY IS MONITORING IMPORTANT
The ultimate goal of monitoring plan and programperformance is to improve health outcomes in themost cost-effective manner while promotingcompliance with contract requirements
Why is Monitoring Important?Managed care is expanding State Medicaid agencies transitioning from FFS to Managed Care More than just a transfer of responsibility Effective contractor monitoring will be particularly critical for states moving populations withspecial needs to managed careRigorous federal reporting requirements Meeting these requirements becomes more challenging with expanding populations, particularlywith expansion to shared savings modelsFiscal Responsibility States are increasingly under the microscope to ensure the best use of taxpayers dollars to gainthe optimum return on the investmentAccountability Value based purchasing .driving performance improvement.
Managed Care Operating in the States, LAFLHIComprehensive MedicaidManaged Care enrollment 66%MCO only (16 states and DC)PCCM only (12 states)MCO and PCCM (19 states)No MMC (3 states)Source: Kaiser Commission of Medicaid and the Uninsured. A Profile of Medicaid Managed Care Programs in 2010:A SummaryFrom a 50 State Survey. September 2011.Page 8
Federal Monitoring RegulationsOverviewFederal rules require quality management for Medicaidmanaged care plansState monitorsquality of careMCOs monitor servicedelivery and performanceimprovement usingHEDIS and CAHPS CMS monitors via aQuality StrategyProgramPerformanceFederal Medicaid Managed Care Regulations (42 CFR 438.200 et seq.)
Impact of the Accountable Care Act onState Medicaid ProgramsNewpopulationsand sedpressuresforefficiencyH.R. 1‐‐111th Congress: American Recovery and Reinvestment Act of 2009. (2009)Kaiser Commission of Medicaid and the Uninsured. A Profile of Medicaid Managed Care Programs in 2010:ASummary From a 50 State Survey. September 2011.
National Themes: Available DollarsState budgets are stressed from the recessionAffordable Care Act provisions introduce new programs andrequirements, including eligibility expansionSource: Center for Budget and Policy Priorities. States Continue to FeelRecession’s Impact. Revised June 2011.Source: Center for Budget and Policy Priorities. States Continue to FeelRecession’s Impact. Revised June 2011.
National Themes: CostsTotal Medicaid Spending and Enrollment Percent Change, FY 1998 – FY 2012Source: Smith, Gifford and Ellis. Moving Ahead Amid Fiscal Challenges: A Look at MedicaidSpending, Coverage and Policy Trends Results from a 50-State Medicaid Budget Survey for StateFiscal Years 2011 and 2012. Kaiser Commission on Medicaid and the Uninsured, October 2011Page 12Source: Smith, Gifford and Ellis. Moving Ahead Amid Fiscal Challenges: A Look at MedicaidSpending, Coverage and Policy Trends Results from a 50-State Medicaid Budget Survey for State
National Themes: Payer & Provider ImplicationsPage 13
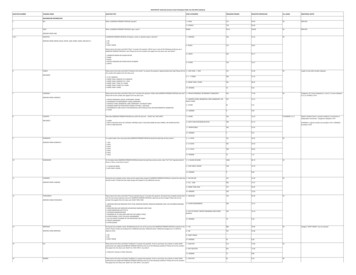
Savings OpportunitiesKey Drivers to Cost Savings (in billions of dollars)1. Administrative System Inefficiency and Errors 100 – 1502. Provider Inefficiency and Errors 75 – 1003. Lack of Care Coordination 25 – 504. Unwarranted Use 250 – 3255. Preventable Conditions and Avoidable Costs 25 – 506. Fraud and Abuse 125 - 175Page 14
Monitoring Medicaid Managed CareTHE CHANGING LANDSCAPE OFMEDICAID: PREPARE FOR IMPACTOPPORTUNITIES AND NEXT STEPS
The Changing Landscape: Prepare for ImpactI. 2014 Medicaid ExpansionEffective January 1, 2014ACA mandates coverage for all children andnonelderly adults with family incomes up to 133%FPL (estimated at 8 to 22 million)States may pursue alternative managed caredesigns to handle the influx of new enrollees.States may enroll additional members in current contractsStates may need to contract with additional health plans toaccommodate increase populationStates may transition current, fee–for-service programs to riskbased managed careH.R. 1‐‐111th Congress: American Recovery and Reinvestment Act of 2009. (2009)
The Changing Landscape: Prepare for Impact- EHR Incentiveprogram- HealthInsuranceExchanges- l InitiativesOther Federal opportunities that are changingthe landscape and helping states prepare- Real-time data- Levers forqualityimprovementand monitoring- Federal dollars
EHR Incentive Program: Administration and Complianceand ComplianceState Medicaid agencies are making significant investments in their Medicaid EHRIncentive Programs and providers stand to earn billions in incentive programs ifthey can successfully apply, attest, and comply with program requirements.The SituationBillions available to providers to promote the adoption and meaningful use of EHRs: Professionals: 60k;Hospitals: MillionsAll states, the District, and the territories are pursuing Medicaid EHR Incentive Programs and have enhanced 90 %Federal funding match available40 states have already gone live and made incentive payments requiring administrative oversight through 2021The ChallengeStates have requested help designing, developing and administering their EHR Incentive programsProviders can receive incentive payments from both State (Medicaid) and Feds (Medicare) and are at riskof financial forfeiture for non-compliance with program requirementsStates must conduct audits within four months of provider payments ---includes all eligibility andmeaningful use criteriaStates will require data analytics to administer their incentive programs and interpret provider dataStates must identify all overpayments and return funds within a year to the Federal government Statesmust identify all overpayments and return funds within a year to the Federal governmentPage18
Cost Containment: Payment Integrity ComplianceHealth Care Fraud, Waste and Abuse (FWA) is believed to be a 70Bindustry and growing. Rx FWA offerings are in nascent stage.The SituationCMS imposes strict Fraud, Waste and Abuse program requirements on Medicare contractors andMedicaid State agenciesPayers are seeking new cost containment / performance improvement strategiesLack of PBM oversightThe ChallengeRetrospective not enough .prospective solutions are sought after as “cost avoidance” is moremeaningfulMarket Lacks comprehensive (integrated medical/pharmacy) one-stop-shop solutionsPayers typically have SIU units that focus predominantly on Fraud and not overpayments/abusePBMs focus primarily on pharmacy fraud and overlook member and provider constituencies
Health Insurance ExchangesStates are scrambling toward preparedness to comply with ACA HealthInsurance Exchange Requirements and Market Impact (EconomicFeasibility/Sustainability, Provider Access, Health Plan Participation)The SituationExchanges continue to be one of the most pressing health care reform implementation issues forhealth plans, states and national policy makersStates will continue to examine the impact of health insurance market reforms, implementation ofpremium payments, submission of benefit and rate information to the Exchange, and the implicationsfor the consumer experience as they search for insurance optionsThe ChallengeSignificant systems integration likely required for State Agenciese.g., State Agency coordination / integration re: eligibility and enrollment for betterconsumer experienceKey Impact: New Processes, e.g., Qualified Health Plan (QHP) Selection:LicensingCertificationRe-certification / de-certification
Monitoring Evolution: From Complianceto Performance ImprovementBasic Monitoring – Program Inception Focuses primarily on policies and procedures, operations, andhealth plans' past performance and experience. Includes the readiness review and focuses on collecting baselinedata for future monitoring Can the health plan support the program?Compliance Monitoring - “Growing Pains” Focuses on contract compliance and compliance with otherprogram requirements Frequency of compliance monitoring is based on priorities andpast complianceQuality and Performance Monitoring - Seasoned/TenuredProgram Helps the reviewer understand how the health planoperates Focuses on high priority clinical areas and measures towhat extent the health plan is successful in improving healthoutcomesPage 21
Monitoring Must-HavesGoals: Health plans andstate agencies share thesame goalStructure: Develop andmaintain an appropriateorganizational structureTools: Develop and usetools that support themonitoring goalsProcesses: Developmonitoring processes,policies and proceduresPeople: Train healthplan and state staff towork together toward thecommon goalPage 22
Integration and CoordinationClinical models and paymentsTechnology as a driver of qualityInfrastructure to drive integration and performance improvement
Integration and Coordination: OverviewStates are realigning staff, data and technologyto deliver “care for the whole person”– The right data, presented in the right manner helpsclinicians and policy makers make the rightdecisions.– Using the data effectively to monitor and evaluatedrives the quality and cost containment process
Integration and CoordinationClinical Models and PaymentACOsPatient CenteredMedical Homes Promote integrated, organizedprocesses for delivering coordinatedservices that meet the highest qualityand efficiency standards Designed at the macro/systems level Similar goals of an ACO Utilize payment redesign, qualityreporting requirements, datarequirements and accreditation todrive performance and qualityimprovement at the micro/providerlevel
Integration and CoordinationTechnology as a driver of qualityEHRs: Real time collection of data used for qualitymonitoring and improvementsHealth information exchange at the regional and statelevelsOther Drivers: ICD-10; cost sharing for duals anddata availabilityChallenges persist: submitting and collecting valid data,making comparisons over time across providers
Integration and CoordinationInfrastructure that drives integration and performance improvementInfrastructure- Training- Experience- ToolsThe key is not to just havereports with numbers onthem, but rather to buildcomprehensive plans forgathering, analyzing,disseminating, and usinginformation to s
Conclusion States must effectively monitor and plan“today” to help them best prepare for“tomorrow” Demand for accountability will increase Competition for dollars will increase
EHR Incentive Program: Administration and Compliance and Compliance 18 All states, the District, and the territories are pursuing Medicaid EHR Incentive Programs and have enhanced 90 % must identify all overpayments and return funds within a year to the Federal government The Situation