Transcription
m Avalon Healthcare SolutionsCONTACT USABSTRACTAvalonHealthcareSolutions(Avalon), founded in 2013, is aclinical and information technologycompany helping physicians,consumers, and payers maximizethe cost-effective use of diagnosticlaboratory tests. Leveraging wellestablished laboratory science,Avalon has developed and deployeda comprehensive Laboratory BenefitManagement (LBM) solution tomanage laboratory testing qualityBarry S. Davis, Chief Growth Officer201-218-3425barry.davis@avalonhcs.comand spend on behalf of payers.Avalon’s solutions help payerstransform their lab benefit fromthe old fee for service model to aValue Based Care model, deliveringimproved quality and significantlaboratory cost reduction. Further,Avalon serves as a valuable resourcefor payers, providers, and patientsas they navigate an increasinglycomplex and clinically challengingtesting landscape.1Sara Sabin, VP, Business elo Devita, VP, Business Dev.215-872-2202Angelo.Devita@avalonhcs.comFred Barry, VP, Business Dev.714-615-1889Fred.Barry@avalonhcs.comJoy Harris, Director, Business Dev.813-751-3814joydana.harris@avalonhcs.comVisit AvalonHCS.com
Avalon’s Program ResultsThrough a robust solutionwhich entails both GeneticTestingManagementandRoutine Testing Management,Avalon has demonstrated theability to successfully decreasethe utilization of unnecessarylaboratoryproceduresanddrive the continual reduction ofinappropriate testing and codingover time. Members also benefitfrom the improved alignment tothe laboratory science standardsas they receive high-quality careand avoid costs associated withunnecessary testing. Currentlyserving health plans representingover 21 million members, Avalon’sLaboratory Benefit Management(LBM) solution commonly delivers10-18% savings across all outpatientlaboratory services.In 2019, Avalonhelped commercialplans save between 1.75 - 2.35Per Member PerMonth (PMPM) inunnecessary labtesting spendCURRENT INDUSTRY CHALLENGESA growing problem exists in thefield of laboratory medicine whichcontinues to cause unnecessarywaste and medical spend. At theforefront of this issue is the increaseand unnecessary utilization oflaboratory testing, as well as thehigh variance in cost of testing.urine, or tissue to help diagnosea condition. Across Avalon’sbook of health insurance payerbusiness, laboratory expensesrepresent 6-10% of total healthcarecosts and are often increasingat a rate greater than growth inoverall medical expense. Manyresearchers have found that theINCREASING LABdemand for laboratory testing isUTILIZATIONincreasing disproportionally when1Laboratory tests can be defined compared to medical activity .as medical devices which utilize Studies show that approximatelybiological samples such as blood, 29% of all outpatient encounters2are associated with laboratorytests; further, among specialistencounters such as encounterswith oncologists or cardiologists,the percentage associated withlaboratory tests is even higherat 88%2,3. To control this testingexcess, physicians must be able toappropriately order tests, resultsmust be provided in a timelymanner, and findings must beinterpreted correctly.
Unnecessary LabUtilizationlaboratory utilization has amplifiedover time, the need for identifyingand managing inappropriateWhenusedappropriately,laboratory procedures has becomelaboratory procedures inform careincreasingly evident. Integral topathways and guide treatmentthe management of inappropriatedecisions. However, a recenttesting is the further understandingmeta-analysis showed that overof provider behavior and the factors20% of all laboratory utilization isthat impact the utilization ofnot medically necessary4; otherslaboratory testing.estimate this number to be as highas 33%5. Overtreatment or low-value From a member perspective,care in the medical field, including several studies have identifiedlow-value screening, testing, or andevaluatedinappropriateprocedures, has led to excess spend laboratory testing as a sourcebetween 17.2 and 27.9 billion in of increased financial burden8,9,the United States annually6.delayed diagnoses and subsequent20% - 33%OF LAB UTILIZATIONIS NOT MEDICALLYNECESSARYInappropriate laboratory testingmay include overordering testsnot necessary for adequate patientcare, and failing to order theappropriate diagnostic test (whichmay account for approximately 50%of avoidable laboratory orders)7.The unnecessary utilization of testsnot only leads to overutilization,but also lead to an increasedrisk of incorrect diagnosis andtreatment, unnecessary followup visits, an increase in resourceutilization, increased length inhospital stays, and unnecessarypatient stress7. As inappropriatetreatment10, hindered qualityof care, and decreased patientsatisfaction11. At the same time,the extremely high laboratorytest volume, complexity of thescience, and increasing number ofcommercially available tests hasprecluded most health plans fromfully managing the laboratorysegment of spend. Over the last20 years, the number of laboratorytests available to clinicians hasincreased significantly; currently,more than 75,000 genetic tests areon the market, with approximately10 new tests introduced daily12.THERE ARE75,000 GENETIC TESTSON THE MARKET3Laboratory testing may bedivided into genetic tests, suchas single gene testing and paneltesting, and routine tests, suchas complete blood count, lipidpanels, or urinalysis. Both types oftesting have led to unnecessary labutilization.APPROXIMATELY13% - 30%OF GENETIC TESTS AREORDERED IN ERRORGenetic Testing: Approximately13%-30% of genetic tests are orderedin error13,14. Further, these tests areexpensive, complex, the science ischanging rapidly, and number oftests are exploding.Routine Testing: This represents 90% of lab spend with a highvolume of unnecessary tests,inappropriate billing, and pricediscrepancies.HIGH COST VARIANCEFurther, high variances in costfor the same test also impact thelaboratory testing community.The American Medical Association(AMA) has created CurrentProcedural Terminology (CPT )codes and Proprietary LaboratoryAnalyses (PLA) codes to standardizemedical procedures performed in
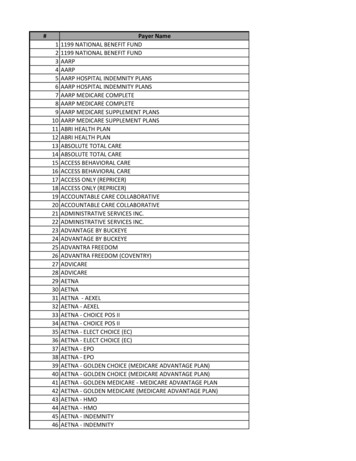
inpatient and outpatient settings.Other coding types include theHealthcare Common ProceduralCoding System (HCPCS) developedby the Centers for Medicareand Medicaid (CMS), and theInternational Classification ofDisease (ICD) coding systemdeveloped by the CMS and theNational Center for HealthStatistics (NCHS). These procedurecodes are used by providers toorder laboratory tests, as well asfor billing and tracking purposes.Figure 1 below shows the pricingarbitrage of two CPT codes (83036and 82306), exposing how thesame test experiences a widevariance of cost across place ofservice (POS). Several types of POSexist including physician offices(11), outpatient services includinghospital laboratories (19 and 22),and independent laboratories(81). Regarding CPT codes 83036and 82306, up to 31% of outpatientlaboratory spend could be avoidedthrough POS optimization, asshown in the figure below.Average Allowed per Unit by Procedure Code and Place of ServiceGlycosylated hemoglobin test(83036)Vitamin D 25 Hydroxy(82306)Procedure CodeFigure 1: Pricing arbitrage of CPT codes 83036 and 82306 categorized by place of service.4
Inapt Methods toResolve the ProblemSeveral methods have se methods include priorauthorization, individual providercontracting, and clinical laboratoryeditor software. Unfortunately,each method has also introducednew impediments to the laboratorytesting field.Inefficient PriorAuthorizationProcessesPrior authorization (PA) is a processrequested by a health insurancecompany that requires a physicianto obtain approval from the healthplan before the cost of specifictests, medications, or medicalprocedures will be paid. Theserequests are approved or deniedbased on medical necessity. Thisprocess was developed for manyreasons including to stop patientsfrom being prescribed medicationthat they do not need, to check forpotential drug interactions, and todetermine if a more cost-effectivegeneric alternative is available.However, many complain aboutcurrent PA practices stating that thistechnique often causes patients toexperience delays and restrictionsin necessary care15. A surveycompleted by the AMA showed that90% of physicians surveyed claimedthat the PA process delayed patientaccess to necessary care; further,26% of physicians had waited threeor more business days, on average,for PA decisions to return fromhealth plans in the previous weekalone15.90%OF PHYSICIANSCLAIMED THE PAPROCESS DELAYEDPATIENT ACCESS TONECESSARY CAREANNUAL PA COSTSFOR THE HEALTHCARESYSTEM ARE BETWEEN 21 BILLION- 31 BILLIONtremendously from an automatedPA system for screening andverification. PA is a very expensiveprocess, typically costing 35 100 per occurrence; this is muchmore expensive than electronicprocessing of claims which can costas low as 0.6615. Total PA costs forthe healthcare system are between 21 billion to 31 billion annually16.Individual ProviderContractingThe key metric for most health plancontracting activities is cost/test.Many current health plan systems Historically, the achievement of alack the foundation for data reduction in lab services expenseexchange, resulting in time involved a narrow network andconsuming manual methods. an exclusive relationship withIt has been suggested that one of the large national labs.healthcare providers would benefit This contracting philosophy can5
result in increased expenses dueto out of network lab leakage,ordering provider dissatisfactionassociated with limited choice inlab services, especially with respectto specialized labs (e.g. genetictesting), and a general lack ofaccess to lab services for the plan’smembers. These issues have drivenmembers to seek lab services at thehigher cost laboratories associatedwith integrated health systemswhere there is a perception ofhigher quality. In addition, there isa lack of education of the renderinglabs with respect to the plan’smedical policies. This results in theover-utilization of common testsand therefore high-cost, backendprocesses to recoup these expenses.Finally, the rapid emergence of newtesting technologies combinedwith limited resources to reviewand assess these new tests resultsin either the addition of testingwith limited clinical utility, ora blanket moratorium in theadding of important advances intechnology. The consequence ishigher cost due to unnecessarytesting or in member appeals to theplan for coverage for needed testingservices.accuracy, increase medical andadministrative savings, and reduceappeals. Some claims editorsfocus primarily on front-end editsto prescreen claims for potentialbilling and coding errors17.Examples of common claim editorsinclude ClaimsXten , Cotiviti, andOptum. A common theme with thecurrently available claims editorsis that they exhibit difficulty in theadministration of policy adherence.Similarly, health plans tend to focuson payment and coding but noton the medical policy itself. ThisMinimal Editingmay lead to gaps in enforcementVarious software-based claim that current claims editors cannoteditors have been developed which mend.create automated rules to improveAvalon’sComprehensive SolutionTo combat current limitations inthe healthcare field, Avalon hasredefined the way health plans,physicians,andlaboratoriescoordinate laboratory care formillions of patients by developingand deploying a comprehensiveLaboratory Benefit Management(LBM) solutionto managelaboratory spend on behalf ofpayers.Thecomprehensivesolution, detailed below, wasdeveloped to deliver the best-inclass laboratory services to patientswhile also delivering annualoutpatient laboratory savings.Avalon’s solution helps payers movefrom the old Fee for Service modelbased on volume, to a Value BasedCare Laboratory. This increasesaccess to the right tests, improvesclinical outcomes, and reducesoutpatient laboratory costs.6Clinical Advisory Boardand Medical PolicyAvalon’s independent ClinicalAdvisory Board (CAB) stands at theforefront of laboratory technologyassessment. The CAB, as depictedon the following page in Figure2, is comprised of five prominentindividuals in the medicalcommunity located across thecountry.
Avalon provides scientific labpolicies to be reviewed by the CABexperts on a quarterly basis. Theapproved and finalized policiesare offered to payers for adoption.These policies may be adopted intotal or adopted with variance(s),depending on the client’s needs orpreferences.Avalon’s medical policy catalogencompasses approximately 140evidence-based lab policies, eachreviewed and revised at leastannually or when the sciencechanges. These medical policyreviews also include an evaluationof procedure codes to ensure theappropriate testing and medicalnecessity of testing are utilized.Further, new policies are alsointroduced depending on clientor scientific community needs.Policies are managed throughour Routine Testing Managementor Genetic Testing Managementsolutions.Geoffrey S. Baird,MD, Ph.D.Timothy R. Hamill,MDVICTORIA PRATT,Ph.D.Brian P. Rubin, MD,Ph.DBrian R. Smith, MDChairProfessor emeritusand Ex-Vice Chair,Laboratory Medicine,University of SanFranciscoPracticing Medicaland Clinical MolecularGeneticist, BoardCertifiedPracticing Pathologistwith subspecialtyexpertise in bone andsoft tissue tumorsProfessor & Director ofthe PharmacogenomicsLaboratory at IndianaUniversity School ofMedicineProfessor and ViceChair of Pathology;Dir., Soft TissuePathology; Dir., Bone &Soft TIssue PathologyFellowship Program,Cleveland ClinicProfessor and Chair ofLaboratory Medicine,Prof of BiomedicalEngineering, Medicine(Hematology) andof Pediatrics at YaleSchool of MedicinePracticing Pathologist,Board CertifiedDirector of ClinicalChemistry atHarborview MedicalCenter, SeattlePrior Director, UCSFClinical LaboratoriesLaboratory MedicalDirector at NorthwestHospital, SeattlePast President,Association ofMolecular PathologyFigure 2: The independent CAB featuring affiliated and practicing laboratory clinicians representing leading medical centerlaboratories across the United States.Avalon provides scientific labpolicies to be reviewed by the CABexperts on a quarterly basis. Theapproved and finalized policiesare offered to payers for adoption.These policies may be adopted intotal or adopted with variance(s), evidence-based lab policies, eachdepending on the client’s needs or reviewed and revised at leastpreferences.annually or when the sciencechanges. These medical policyAvalon’s medical policy catalog reviews also include an evaluationencompasses approximately 140 of procedure codes to ensure the7
appropriate testing and medicalnecessity of testing are utilized.Further, new policies are alsointroduced depending on clientor scientific community needs.Policies are managed throughour Routine Testing Managementor Genetic Testing Managementsolutions.Routine TestingManagement onis powered by the proprietarycloud-based clinical lab editingapplicationknownastheAutomated Policy EnforcementApplication (APEA). Approximately70 of Avalon’s medical policiesare partially or fully managed byAPEA. In real-time, APEA providesdecision advice codes to deny,reduce, or approve claim linesalong with references to specificpolicy detail supporting theIntakeFor health plans who are notProvides real-timeyet equipped to implement theclinical lab editingAPEA system, a solution has beendeveloped to adequately supportRuns on cloud-basedclaims. This solution, known asAmazon Web ServicesAPEA-Pre, was established byProvides advice toAvalon as a temporary measure todeny, reduce, orprovide savings before the healthapprove claims in 1 secondplan completes its integrationwith APEA. This tool allows AvalonHandles 2 million independent laboratory providerautomated evidenceclaims to be reviewed in APEA-based lab editsby pre-editing claims prior todecision. APEA may be integrated submission to the health plan. Thiswith the payer’s adjudication APEA alternative has proven to besystem to automate the review of successful with clients.fixed criteria from lab claims to Genetic Testingensure compliance with the payer’s Management (GTM)policies.Avalon’s proven APEA solution is Avalon has a robust programhighly configurable and can support that oversees Genetic Testingexemptions by various filters such Management (GTM), as depicted inas line of business, place of service, Figure 3 below. The four principleand provider. APEA savings have steps of the GTM process consistproven to be incremental and of intake, clinical evaluation,notification, and appeal ealSupportKey Features1. Test Identification: Analyte-specific evaluation of molecular panel and unlisted codes2. Panel Evaluation: Promotes appropriate use of lab-specific molecular panels (elimination ofunsuitable code stacking and/or excessive panels)3. Decision Detail: Accessible and easy to understandFigure 3: Avalon’s GTM process. The four broad phases of the GTM process include intake, clinical evaluation, notification,and appeal support.8
In the initial intake phase, a requestis received for Prior Authorization(PA) review. During the clinicalevaluation, the nurse or physicianreviews testing that the orderingphysician has requested, alongwith the clinical information andrecords provided, to see if theprescribed test or panel is medicallyappropriate. Proactive outreachmay also occur if clarity is neededin order for the reviewing physicianor nurse to evaluate a request. Thereviewing nurse or physician, forquality assurance, also reviews therequest submitted by the renderingprovider to ensure that it matchesthe test or panel ordered by theinitial provider and that the codingfollows AMA guidelines.For an approval notification,both the ordering and renderingprovider receives a notification.If a claim is denied, the member,the ordering provider, and therendering provider all receivedetailed notifications. A clear,readable description of why anadverse determination was givenis included within the notification.This notification will contain thereason(s) why the ordered test is notconsidered medically necessary. Ifthe denial is solely due to a codingdiscrepancy, then as part of theeducation process, the rationaleincludes how the member may beable to receive approval for testingif the correct procedure codes aresupplied on resubmission. AppealSupport includes educationalendeavors to help abate abrasionthat health plan clients may receiveas well as internal provider andnetwork lab education. This oftenincludes peer-to-peer consultation.Avalon has also integrated geneticcounseling into the current GTMprocess to reduce inappropriategenetic test utilization, decrease thenumber of adverse determinationsdue to lack of genetic counseling,and ensure that patients arereceiving the most appropriatetest. Avalon focuses on theutilization of physicians and nursesfor peer to peer education andintegrates genetic counseling whenappropriate. Genetic counseling ispromoted by Avalon prior to testingwhen warranted.9Further, a portion of the GTMsystem can be automated throughan Avalon-based proprietary selfservice Prior Authorization System(PAS). PAS was implementedin April 2019 as an on-demand,24/7 tool for providers to submitor check the status of existingpreservice review requests (PSR).Approximately 86% of PSR requestsare submitted through PAS andabout 100 CPT, HCPCS, and PLAcodes have the capability of beingautomatically approved whensubmitted through PAS via itsbuilt-in clinical rules engine. If PASis unable to automatically approvethe PSR request, the request isreviewed by Avalon’s clinical staff.Orderingandrenderingproviders are notified of all PSRdeterminations, approvals, anddenials via an electronic notificationand have immediate access totheir determination letters viaPAS. Avalon’s focus on providereducation and high-touch modelhelps the provider and memberget the right test approved, leadingto greater physician and membersatisfaction.
Independent LaboratoryNetworkAvalon partners with over 60independent laboratories creating abroad network that supports clienthealth plans in all medical areas.Leveraging 50 years of leadershipexperience in the laboratoryindustry, Avalon can increase thescope of network managementwhile acting as an adjunct to thehealth plan’s current resources.Avalon’s ability to capitalize on themerging of 60 individual vendorrelationships and fee schedulesand incorporate these into asingle standard reimbursementmechanism brings greater accessand satisfaction for members andproviders. Avalon’s broad networkphilosophy provides expandedadvanced diagnostic resourcesthrough national laboratories aswell as in the specialty focus labspace. We have the ability to managethe myriad of new and emerginglaboratory technologies whilealso aligning the utility of medicalpolicy, coding, and appropriatereimbursement. This allows plansto better focus on their business,mission, and member engagement.Avalon has demonstrated theability to successfully decreasethe utilization of unnecessarylaboratoryproceduresanddrive the continual reduction ofinappropriate testing over time.This has led to a positive impact forproviders and members by avoidingunnecessary testing with the addedbenefit of reduced costs.As shown in Figure 4, in 2019 Avalonhelped commercial populationbased plans save between 1.75and 2.35 Per Member Per Month(PMPM) in unnecessary outpatientlaboratory testing spend throughRTM and GTM.This 2.35 PMPM savings can befurther categorized by GTM andRTM. Figure 5 shows that in 2019, 0.55 of the 2.35 PMPM savings can2019 Saved CostsAvalon’s Success in ReducingUnnecessary Lab Utilization2019 Avalon Client Saved CostsPMPM4.00 2.352.000.00Actual Saved CostsFigure 4: In 2019, Avalon helped commercial plans save between 1.75 and 2.35PMPM in unnecessary laboratory testing spend. RTM saved costs occurred becauseclaims did not meet coverage criteria and laboratory policy specifications, and GTMsaved costs occurred because the requests were not considered medically necessary.2019 Saved PMPM Costs by Enforcement 0.55, 23% 1.80, 77%GTMRTMFigure 5: The PMPM savings that Avalon helped plans achieve in 2019, split betweenGTM and RTM. Of the total 2.35 PMPM savings in 2019, 0.55 was due to GTMenforcement and 1.80 was due to RTM enforcement.10
be attributed to GTM enforcement, Incorrect coding of laboratory testsand 1.80 can be attributed to RTM for a grander payout was identifiedenforcement.as a common occurrence by Avalon.For example, many laboratoriesGenetic Testingwere found to be coding lab testsManagement (GTM)erroneously, particularly tests thatAvalon has achieved great success should have been listed as part ofwith their Genetic Testing a panel test. Instead, they wereManagement (GTM) program as it coded under CPT 81479 (unlistedeffectively prevents unnecessary molecular pathology procedure)and low-quality, high-cost tests for higher payment. Avalon’s GTMprospectively. The GTM program review has successfully preventedalso helps to ensure that labs are this incorrect coding practice frominputting codes correctly and moving forward. Figure 6 belowlists the top five CPT code denialsappropriately.through Avalon’s GTM program.These denials accounted for alarge portion of 2019 GTM relatedsavings.Additional data in Figure7 below show how Avalon’s GTMmanaged population successfullylowered costs compared to healthplan populations that were notmanaged by Avalon. Utilizationand associated costs were 45%higher in populations withoutAvalon GTM programs as comparedto populations with Avalon GTMprograms in 2019.Top Denied Procedure CodesFigure 6: The top denied procedure codes through GTM. Unlisted molecular pathology code 81479 accounts for a majority of thedenied units.Allowed PMPMGTM Utilization (Dollars) 0.6345% 0.43GTM Unmanaged PopulationGTM Managed PopulationGTM Allowed PMPM11Figure 7:GTM utilizationin dollarsbetween AvalonGTM managedand Avalonunmanagedpopulations.
Routine TestingManagement (RTM)Services. Advice to deny, reduce,or approve claims is provided toclients in less than one second.Avalon’s APEA solution decreasesthe volume of inappropriate testsand increases compliance withpolicies. Members also benefitfrom the improved alignment tounnecessary testing. An exampleof APEA’s success is revealed belowin Figure 8. The compound annualgrowth of units ordered PMPM inpopulations without APEA (green)is increasing at 4.9%, while thecompound annual growth of unitsordered PMPM in populations withAvalon has also achieved greatsuccess with their Routine TestingManagement (RTM) programpowered by the AutomatedPolicy Enforcement Application(APEA). This program effectivelythe laboratory science standards APEA (blue) is decreasing at -2.7%.provides real-time clinical labas they receive high-quality care The utilization of APEA has alsoediting through the utilizationand avoid costs associated with led to a decrease in billed unitsof cloud-based Amazon WebAPEA Units PMPM by APEA StatusUnits PMPM4.9%-2.7%Quarterwithout APEA Paid Unitswith APEA Paid UnitsFigure 8: RTM, powered by APEA, bends the healthcare trend by showing a negative drift in compound annual growth for populationswith APEA.Billed Units PMPMChange in Billed Unit Utilization by Place of ServiceFigure 9: Billed units across place of service are decreasing after APEA implementation.12
across POS. Decreased units canbe attributed to provider educationand more appropriate billingpractices. As noted in Figure 1,the same test may experience awide variance of cost across POS.Figure 9 shows that the orderingof labs in physician offices (11)and independent laboratories (81)has decreased significantly afterAPEA implementation; further,outpatient hospital laboratory(19/22) ordering is modestlydecreasing as well.experiencing increased utilization.Many health plans have adopteda medical policy supportingscreening for Vitamin D deficiencyin individuals considered high riskfor vitamin D deficiency, whilelimiting coverage for screeningin healthy populations. Avalon’sAPEA system was set up to enforcethese complex criteria on behalfof payer clients. The results wereimpressive and are depicted belowin Figure 10. In this case study,Vitamin D testing was 2.4 timesmore likely to be compliant withMany additional examples of the established science. Prior toAPEA’s impact on correct coding APEA implementation, over 40%can be found throughout Avalon’s of all vitamin D tests billed tolarge portfolio of medical policies. the health plan were not alignedFor example, vitamin D testing with the established science.is commonly overutilized and is Following APEA implementation,Vitamin D Policy Compliance: Before and After Case StudyClaims Compliantwith PolicyClaims Not Compliant withPolicy - Paid by Heath Plan6 Months Before APEA Go-LiveNon-compliant Claimsdenied by APEA6 Months After APEA Go-LiveFigure 10: RTM, powered by APEA, bends the healthcare trend by showing a negative driftin compound annual growth for populations with APEA.13the health plan stopped payingfor the inappropriate tests andexperienced a significant costssavings. At the same time, thenumberofnon-compliantclaims decreased in the monthsfollowing APEA implementation aslaboratory providers modified theirtest menus to support on-goingpolicy compliance. Many payershave a vitamin D policy, and otherpolicies, but their systems are notable to enforce them. APEA ensuresthe payers policies are administeredand enforced correctly.CONCLUSIONAvalon has successfully providedthe best-in-class laboratory servicesto patients while also deliveringannual outpatient laboratorysavings. Avalon’s independentClinical Advisory Board (CAB)ensures that all medical policies arecurrent and relevant. Further, boththe Routine Testing Management(RTM) and Genetic TestingManagement (GTM) programs haveimproved outcomes, increasedprovider and member satisfaction,and provided substantial savings toclients. These programs have alsopositively impacted correct codingpractices and have led to a decreasein billed units across place of servicewhich can be attributed to providereducation and more appropriatebilling practices.
evidence-basedscientific references1. Freedman DB. Towards Better Test Utilization - Strategies to Improve Physician Ordering and Their Impact on Patient Outcomes.Ejifcc. 2015;26(1):15-30.2. Zhi M, Ding EL, Theisen-Toupal J, Whelan J, Arnaout R. The landscape of inappropriate laboratory testing: a 15-year meta-analysis.PLoS One. 2013;8(11):e78962.3. Rohr UP, Binder C, Dieterle T, et al. The Value of In Vitro Diagnostic Testing in Medical Practice: A Status Report. PLoS One.2016;11(3):e0149856.4. Ngo A, Gandhi P, Miller WG. Frequency that laboratory tests influence medical decisions. The Journal of Applied LaboratoryMedicine. 2017;1(4):410-414.5. Mize R, Hunt S, Redman W. The Issue of Test Utilization within the Clinical Laboratory. Journal of Business and Behavior Sciences.2019;31(2):70.6. Shrank WH, Rogstad TL, Parekh N. Waste in the US Health Care System: Estimated Costs and Potential for Savings. Jama. 2019.7. Cadamuro J, Ibarz M, Cornes M, et al. Managing inappropriate utilization of laboratory resources. Diagnosis (Berl). 2019;6(1):5-13.8. van Walraven C, Naylor CD. Do we know what inappropriate laboratory utilization is? A systematic review of laboratory clinicalaudits. Jama. 1998;280(6):550-558.9. Hauser RG, Shirts BH. Do we now know what inappropriate laboratory utilization is? An expanded systematic review of laboratoryclinical audits. Am J Clin Pathol. 2014;141(6):774-783.10. Epner PL, Gans JE, Graber ML. When diagnostic testing leads to harm: a new outcomes-based approach for laboratory medicine.BMJ Qu
a comprehensive Laboratory Benefit Management (LBM) solution to manage laboratory testing quality and spend on behalf of payers. Avalon's solutions help payers transform their lab benefit from the old fee for service model to a Value Based Care model, delivering improved quality and significant laboratory cost reduction. Further,