Transcription
CLINICAL TRIALS: HOW TECHNOLOGYIS DRIVING DIGITISATIONMEDICAL TECHNOLOGY
CLINICAL TRIALS: HOW TECHNOLOGY IS DRIVING DIGITISATIONWHITE PAPERINTRODUCTIONThe era of clinical trials as we’ve known them, is coming to an end.The rising costs of running a trial, coupled with the commercial risks offailure, are unsustainable. This disruptive state is driving the adoptionof new technologies, and catalysing the digital transformation of clinicaltrials.Clinical studies constitute the most critical stage of a drug’sdevelopment, and a key activity in the calendar of any clinical trialsponsor. They are costly, with unpredictable timelines, and theiroutcomes influence the short and long-term future of pharmacompanies. To give a sense of scale, there are approximately7,000 Phase III interventional clinical trials1 currently active.Bearing in mind that a Phase III trial could cost tens of millionsof dollars, the impact that they can have on any sponsor’sbalance sheet is considerable. Clinical trials attract the interestof regulators, investors, and even patient advocacy groups.They involve multiple stakeholders, across multiple countriesand their published results often make it to the mainstreampress. As a result, the pressure on pharmaceutical companiesto succeed is not only financial but also reputational. Here, weidentify the key challenges that clinical trial sponsors face andsuggest the use of digital technologies to address them. Wealso present the fundamental technological solutions that willcatalyse the transformation of clinical trials.1 https://clinicaltrials.gov/ct2/results?recrs b&recrs a&recrs f&recrs d&age v &gndr &type &rslt &phase 2&Search Apply01
WHITE PAPERCLINICAL TRIALS: HOW TECHNOLOGY IS DRIVING DIGITISATIONWHY CHANGESUSTAINABILITYEscalated clinical trial costs drive the cost of developingtreatments, which in turn impacts the price of productsand burdens healthcare reimbursement systems. In 2013alone, the cost of the 6,199 biopharmaceutical sponsoredclinical trials in the U.S. was calculated to be in the regionof 10 billion2. The same trend applies to the complexity ofrunning clinical studies, particularly given that the number ofregistered studies has quadrupled since 20093. As a result,there is pressure on companies to reduce development costs,and justify the price of their product according to achievedendpoints and outcomes. With so much at stake, clinicaltrial sponsors need to mitigate the risks, identify areas ofimprovement and control the spiralling costs. If sponsors donot act, it is likely that payers will.AGILITYClinical trials are not dynamic in nature. Slight changes totheir protocols require time to implement. Investigators oftentitrate treatments according to the drug’s efficacy performanceand the occurrence or persistence of side effects. SuchAGILITYSUSTAINABILITYCLINICAL TRIALSOPERATIONSRECRUITMENT2302WHYCHANGE?QUALITY OFPATIENT-REPORTEDOUTCOMESINFORMED ENCE
CLINICAL TRIALS: HOW TECHNOLOGY IS DRIVING DIGITISATIONchanges rely heavily on timely access to information, so thatinvestigators can make informed decisions. However, thisusually requires a face to face meeting with a patient, whichis resource demanding and takes time to organise. Similarly,it is not easy to deal with changes in a standardised wayacross multiple centres. There is scope for technology toclose the gap and allow for more efficient and scalable dataaccess.QUALITY OF PATIENT-REPORTED OUTCOMESThere is a need for more efficient management of patientreported outcomes (PRO). Patients are required to completePRO surveys at least twice throughout the duration of a clinicaltrial and this is expected to take place at predetermined timepoints. Failure to do so impacts the quality of the data andcould put patients under unnecessary safety risk. A recentstudy by Kyte et al.4 revealed several inconsistencies inhow this process is managed across different clinical trialcentres. PROs are often not completed, or completed atincorrect times. Moreover, clinical trial staff do not respondto incomplete and overdue PROs in a standardised fashion,which introduces bias to the data captured. The authors ofthe study also revealed that it is possible for clinical trial staffto not respond to PRO alerts in a timely and standardisedmanner – e.g. when evidence exists that a patient is underpsychological distress. Improving standardisation levelswhen it comes to the completion, processing and analysis ofPROs would positively impact clinical trials.PATIENT ADHERENCENon-adherence is a key challenge for clinical trial sponsorsas it increases costs, and impacts both outcomes andendpoints. Lack of monitoring systems for adherence couldlead to misinterpretation of data on the effectiveness andsafety of a treatment. There have been numerous studies thathave analysed data from clinical trials and have concludedthat adherence reporting is often inconsistent, causing dataanalyses to be biased5,6. Lack of adherence, when accountedfor properly at the data analysis stage, reduces the statisticalpower of the study sample, which automatically impacts thevalidity of the study. It has been reported that non-adherenceto investigational medical products can be as high as 40%after just 150 days from the beginning of the clinical trial.Interestingly, there is an exponential relationship betweenthe level of non-adherence and the number of patients that456789WHITE PAPERneed to be recruited to conserve the statistical power ofthe sample in a study. For a non-adherence level of 40%, a200% increase in sample size7 is required, which makes theneed to address this issue more than evident.CLINICAL TRIAL OPERATIONSRECRUITMENTRandomised, controlled clinical trial patient samples are notrepresentative of the patient types that HCPs treat underreal world conditions, and in many cases would not pass anexternal validity or generalisability test. There is a need torecruit patients across more geographies and demographicsand for patients that better represent the clinical scenariosunder which a treatment will be used. By default, theintroduction of more screening criteria will make therecruitment process more resource demanding, costly andlengthy. There are many limitations that clinical trial sponsorsneed to overcome in order to make the recruitment processmore efficient. One such barrier is making the propositionof joining a clinical trial more attractive to patients. Forexample, patients can often be sceptical about the fate of thedata generated during clinical trials 8 and the effectivenessof data security mechanisms employed. Moreover, patientsdo not appreciate the fact that data they generate cannotbe accessed by healthcare professionals of their choice, orbecome part of their standard health record. There is scopeto make participating in clinical trials more attractive.INFORMED CONSENTPatient informed consent is the cornerstone of clinical trialsand failure to diligently satisfy consent requirements can havea catastrophic impact on the validity of the study. The currentprocess comprises extensive paperwork, can be confusingand burdensome, tests the commitment of patients and doesnot represent a robust system. Considering that satisfyingconsent requirements is not a single event in the clinical trialcalendar but a more open-ended process (e.g. a patient canwithdraw consent at any point), it causes frustration, leadingto oversights and improper practice. It has been reportedthat a significant percentage of clinical trials assessed bythe FDA exhibit consent collection issues9. Clinical trials willbenefit from streamlining the process of consent, makingit less labour intensive and more effective to manage. Theprocess would benefit from a more transparent system thatallows for constant monitoring by all Personal communication with clinical trials 6603
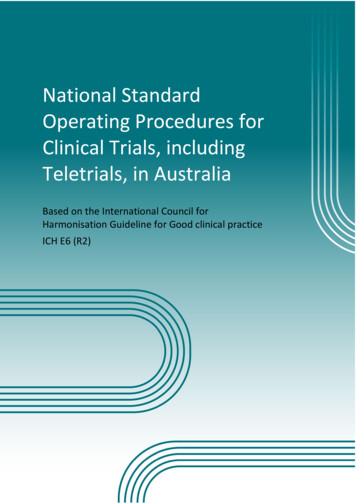
WHITE PAPERCLINICAL TRIALS: HOW TECHNOLOGY IS DRIVING DIGITISATIONHOW CLOSE ARE WE TO CHANGING CLINICAL TRIALS?Clinical trials are a necessity for pharmaceutical companies,as they need to comply with the demand for safe and effectivetreatments at justifiable prices. With so much at stake, the timehas come to improve the efficiencies of clinical trials, and there isevidence that this change is underway.Firstly, over the last 10 years, the Clinical Trials TransformationInitiative (CCTI) – a public-private collaboration – has systematicallypromoted the need to increase the efficiency and quality of clinicaltrials. The CTTI’s recommendations on endpoints, and how digitalservices and tools can create a new gold standard clinical trialdesign, have been critical in transforming clinical trials.Secondly, the global e-clinical solution software market, isexpected to grow to 10.6 billion by 2024, growing at a CAGR of13.4% from 2016 to 202410. The growth of software for clinicaltrials will be fuelled by the need to manage an increasing numberof clinical trials. The larger number of clinical trials will exacerbatethe challenges faced by sponsors today, including the complexrecruitment requirements across multiple centres and countries.The growth of software is also associated with the sponsors’increased appetite for outsourcing studies, while containing theotherwise bursting costs.It should then be no surprise that the amount of VentureCapital funding invested in this area has increased over theyears, while companies specialising in clinical trial softwaresolutions have achieved significant fund-raising successes.One such example is Bio-Optronics, a developer of softwarefor clinical trials, that claims to allow regulatory complianceflexibility and efficiency. Recently, it attracted 30 millionin funding from Mainsail partners11. Equally successful inraising funds has been goBalto12, which since its inception10 years ago has raised more than 35 million. These twoexamples represent just the tip of the iceberg.Another sign of change is the investment that pharmaceuticalcompanies are making in novel technologies. Many of thetop-tier companies are actively seeking solutions that willre-shape the way they conduct clinical trials and give themcompetitive advantage over their competition. Companiessuch as Novartis, Otsuka and Janssen often feature inindustry news related to the adoption of innovations thatcould disrupt the way clinical trials are conducted13. Theirpartnerships with Science 37 – a technology enabled clinicalresearch company that offers decentralised clinical trials – isone example14,15,16.WHAT PHARMA NEEDS TO DO TO STAY ON TOP OF THIS CHANGEDEVICECONNECTIVITY ANDULTRA-LOW COST TA ANALYTICSAND ience-37-sanofi-introduce-new-partnership/
CLINICAL TRIALS: HOW TECHNOLOGY IS DRIVING DIGITISATIONWHITE PAPERWHAT PHARMA NEEDS TO DO TO STAY ON TOP OFTHIS CHANGEDisruption in clinical trials requires the masterful convergenceof multiple technologies and technical capabilities. Theircombination will reinvent the way data is captured, analysedand processed and, in doing so, re-define the role of thepatient in a clinical study. Below, we outline the technologiesand tools that will drive this change17.DEVICE CONNECTIVITY AND ULTRA-LOW COST IOTConnected drug delivery devices and smart primarypackaging are both disrupting the way patient adherencedata is being captured. Connected devices will helpovercome the misinterpretation of data when it comes tothe impact of drug dose related side effects, outcomes andthe patients’ general well-being. A great deal has been doneto enable the connectivity of drug delivery devices for bothrespiratory and parenteral devices. One example comesfrom Novartis, with the introduction of the connectedBreezHaler18 to closely monitor patients’ drug intake duringclinical trials. Information can be shared in real time, andallows clinical trial sponsors to respond and tackle low levelsof adherence. Another example of investment in deviceconnectivity involves Janssen19, which recently invested ina novel clinical trial system that uses smart blister packs.Ultra-low cost connectivity components, coupled withdirect-to-cloud technologies, such as NB-IoT/LTE-M,will fuel the transformation towards fully connected anddigitised clinical trials. Drastically reducing the cost of IoTdevices will remove a key barrier towards the adoption ofnot only connected drug delivery devices but also wearablesensors. To date, the cost of a radio has been determinedby its analogue components, but work to replace theanalogue component with a fully digital radio transceiverhas progressed. Cambridge Consultants’ Pizzicato enablesflexible software-defined radios that can change frequency,bandwidth or radio standard in an instant, allowing a muchmore dynamic use of the radio spectrum. Such systemscould justify economically the use of connected wearablesensors and even connected low-cost drug delivery devices,such as syringes.17181920BLOCKCHAINBlockchain has already proven its value in building atransparent transaction network between parties who do notnecessarily trust each other. Blockchain-based solutions mayalso hold the key to providing more efficient ways of handlingthe early stages of clinical trials, particularly in relation torecruitment. As blockchain provides a controlled way ofaccessing proof of the existence of an entity, it may be usedfor monitoring the existence of consent. This could be ofkey value to clinical trial stakeholders across multi-centredstudies. It means that investigators, sponsors and regulatorswill all be able to share consent information and bettermanage re-consent requirements for each batch of patientdata corresponding to a specific version of a trial protocol.A mechanism like this would warrant proof of existence forconsent and would be timestamped before sharing any data.Benchoufi et al.20 have described a gold-standard, open andsecure consent collection form, using blockchain.As a shared ledger, blockchain can be used to enable andmonitor access to clinical trial data, allowing a transparentyet controlled way of sharing patient information. A systemlike this may help patients to access their data – often heldin data silos – and benefit by sharing it with their healthcareprofessionals (e.g. their GPs). Being able to share personaldata and potentially even use it to update patient healthrecords means that patients may be more incentivised to takepart in clinical trials, and keep high levels of engagementwhen it comes to taking part in the different activities andassessments planned.SENSING TECHNOLOGIESThere are many advances in the field of sensing technologythat could disrupt data collection for clinical trials. Thetypes of sensors, and what they can monitor, has advancedand sensors could feasibly replace manual surveys andassessments. Moreover, sensors are becoming smaller,easier to integrate and use continuously without interferingwith a patient’s everyday life.Clinical trial management solutions for siteless studies are outside the scope of this report and not covered here.Colthorpe et al. Adding Electronics to the Breezhaler : Satisfying the Needs of Patients and Regulators, Respiratory Drug Delivery 2018, in rticles/6-66/v1#ref-1105
WHITE PAPERCLINICAL TRIALS: HOW TECHNOLOGY IS DRIVING DIGITISATIONFor example, contactless sensing may play a key role in howdata is collected. Typically, vital sign monitoring requires onbody electrodes, which of course need direct skin contact andoften some sort of skin preparation to reduce interference.Today there is evidence that even for vital sign monitoring– with the use of near field coherent sensing (NCS) – it ispossible to avoid skin contact. Hui et al.21 demonstrated thatsuch systems could be used to monitor heart rate, bloodpressure, respiration rate and breath effort. The systemtested comprised passive tags which were integrated intogarments at the chest and wrist areas. This type of sensingcould revolutionise the way physiological and PRO data isgathered during clinical trials. Innovation in this space willaddress not only data quality issues but also catalyse animprovement in patient engagement.Advances in materials will also boost efforts to improvesensing technology. With the use of graphene and metalnanowires22, a Korean team developed prototype contactlenses that measure glucose levels and intraocular pressure.“Invisible” sensing will play a key role in the creation ofsensing systems that gather multi-parameter data and allowthe holistic quantification of an individual’s disease status,including that person’s response to treatment during aclinical trial.Data analytics platforms will make or break how impactfulthe clinical trial connected ecosystem can be. This mayinvolve systems that can be calibrated to reflect the weightedcontribution of an individual’s ‘ecology’. Similarly, using AIit will become possible to filter out any data generated bythe individual’s environment, and remove any unwantedbiases. Such objective data analytics platforms will be ableto calculate reasonable benchmarks against which individualpatients will be assessed. Gathering meaningful data for amedical assessment in a non-controlled environment is asignificant challenge and is key in providing trustworthy andimpactful insights.The use of AI will not be limited to data analysis solutions.Instead, we envisage that AI will play a key role in establishingcentre-less clinical trials. It will drive recruitment, patientengagement and will allow trials to run remotely with lessintervention from clinical trial staff. One such technologyexample is Orbita’s voice-based home health assistant23,which claims to provide a more user-friendly way of completingclinical assessments at home. There is great potential in thisspace, which could drive clinical trials beyond the need for aclinical trial centre.DATA ANALYTICS & ARTIFICIAL INTELLIGENCEConnected devices, connected wearables and the possibilityof continuous monitoring during clinical trials open newavenues in terms of the quality of data captured and theoverall insights that could be generated. Nevertheless,to generate these insights, we will need to deal with verylarge datasets, derived from diverse patient populations.Accounting for diversity is particularly important as themanifestation of complex conditions and their symptomsdiffers among individuals. This will require “diverse”and personalised benchmarks against which a person’sprogress can be assessed. For example, let’s assume thatactivity levels are considered an important indicator for thewellness of a patient in a clinical trial. Measuring activityis easy, but analysing the data and associating it with thatpatient’s disease state is far more challenging. For the datato make sense, we must be able to determine how closely itis correlated with the disease, the clinical trial interventionand, hence, validate those correlations before generalisingany findings.21 2 ular-pressure.html23 deployed-in-clinical-trials/06
CLINICAL TRIALS: HOW TECHNOLOGY IS DRIVING DIGITISATIONWHITE PAPERAND SOMETHING ELSEThere is strong evidence of escalating costs for runningclinical trials and a clear need to improve certain processes.Clinical trial digitisation offers a solution for most of thechallenges that need to be addressed, but how easy is it tointegrate new technologies and digitise clinical trials?Could the cost of developing and adopting clinical trials proveto be a barrier in making the switch to digital? When assessingthe positive impact of digital technologies on recruitment,patient engagement, quality of data, adjusting treatmentsand protocols, and improving the agility of studies, it is easyto recognise the value these changes will bring. The averagecost of a patient in a clinical trial is approximately 38,00024.We can assume that the cost of introducing digital tools – thatwill be used again and again, even in commercial settingspost development – will only be a fraction of that total. Ifanything, it is likely that the digitisation of clinical trials willintroduce many cost efficiencies. More importantly, the costof a failed or mismanaged clinical trial will always be farmore significant than the cost of digitisation. To that point, areport commissioned by the U.S. Department of Health andHuman Services concluded that home testing alone could,on average, reduce the cost of a Phase I study by 16%, aPhase II study by 22%, and a Phase III study by 17%. Theimpact on net cost for each phase is significant, consideringthat in the same report the average cost of a phase trial wasestimated to be 20 million25.Clinical trials are slowly changing in order to addressconcerns around their efficiency. These changes have thepotential to offer competitive advantage to clinical trialsponsors. Companies can streamline their clinical trials,improve their R&D efficiency, cut costs and minimise the riskof development. They will be able to increase the numberof their clinical studies, develop and test more treatmentssimultaneously, reach remote and even smaller patient groupsand create better protocols to test their treatments. To do sothey will need to demonstrate an appetite for adopting newtechnologies. Failure to do so could have a long-term impacton their business.WHY DIGITAL TECHNOLOGIES WILLDISRUPT CLINICAL TRIALSThere is a NEED for more clinical trials across more sitesStudies267,88835% are US onlyThe NEED will continue to growRegistered Studies300,000402%annual percent growth rate020002019COSTS can be managed ifwe tackle INEFFICIENCIESThis increase comesat a significant COSTIn 2013 only, biopharma INVESTED 10billion in trials in the USRecruitmentPatient engagementData quality and data sharingAgility in planning & executionaverage cost per patientCompliance 38,000ConsentDigital technologies could reduce trial COSTSand the BENEFITS could be significantPHASE 116%PHASE 222%PHASE 317%DOWNLOAD THE WHITEPAPER24 als-impact-on-state-economies.pdf25 Clinical trial trendsClinical trial costsBiopharma and trials07
WHITE PAPER08CLINICAL TRIALS: HOW TECHNOLOGY IS DRIVING DIGITISATION
About Cambridge ConsultantsCambridge Consultants is a world-class supplier of innovativeproduct development engineering and technology consulting. Wework with companies globally to help them manage the businessimpact of the changing technology landscape.With a team of more than 750 staff in the UK, the USA, Singaporeand Japan, we have all the in-house skills needed to help you – fromcreating innovative concepts right the way through to taking yourproduct into manufacturing. Most of our projects deliver prototypehardware or software and trials production batches. Equally, ourtechnology consultants can help you to maximise your productportfolio and technology roadmap.We’re not content just to create ‘me-too’ products that makeincremental change; we specialise in helping companies achievethe seemingly impossible. We work with some of the world’slargest blue-chip companies as well as with some of the smallest,innovative start-ups that want to change the status quo fast.Cambridge Consultants is part of the Altran Group, a global leaderin innovation. www.Altran.comFor more information, or to discuss how thisapproach could fit your business, please contact:Jaquie Finn, Head of Digital HealthJaquie.Finn@CambridgeConsultants.comHarshal Shah, VP, Global MedTechHarshal.Shah@CambridgeConsultants.com
UK § USA § SINGAPORE § JAPANwww.CambridgeConsultants.comCambridge Consultants is part of the Altran group, a global leaderin innovation. www.Altran.com
HOW CLOSE ARE WE TO CHANGING CLINICAL TRIALS? Clinical trials are a necessity for pharmaceutical companies, as they need to comply with the demand for safe and effective treatments at justifiable prices. With so much at stake, the time has come to improve the efficiencies of clinical trials, and there is evidence that this change is underway.