Transcription
JANUARY 2019TRICARE Mental Health andSubstance Use Disorder ServicesMental health and substance use disorder services are available for you and your familyTRICARE mental health and substance use disorder (SUD)services are available for you and your family during timesof stress, depression, grief, anxiety, mental health crisis,or misuse or abuse of alcohol or drugs. This fact sheetprovides information to help you get the care you need.Visit www.tricare.mil/mentalhealth or contact your regionalcontractor for more information.COVERED OUTPATIENT SERVICESReferrals may be required for certain outpatient services. Inmost situations, prior authorization is not required for anyoutpatient mental health or SUD visit. Active duty servicemembers (ADSMs) should always seek nonemergency mentalhealth care at military hospitals or clinics when available.If services are not available, ADSMs must get referrals andprior authorizations from their primary care managerbefore getting civilian care. Care access and rules vary bybeneficiary type, location and TRICARE program option.Refer to the Getting Care section of this fact sheet for details.Physician referral and supervision may be required whenseeing mental health counselors and is always required whenseeing pastoral counselors.PsychotherapyPsychotherapy is discussion-based mental health therapy.Outpatient psychotherapy is covered when medically orpsychologically necessary to treat a mental health disorder.Outpatient psychotherapy is covered for any combination ofindividual, family, group or collateral sessions for a diagnosedand covered condition from a TRICARE-authorized provider.Beneficiaries who require multiple sessions on the sameday may require a higher level of care (Refer to the IntensiveOutpatient Program and Partial Hospitalization Programsections of this fact sheet for details). The following types ofpsychotherapy sessions are covered: Individual psychotherapy: Therapy may be used whenmedically or psychologically necessary for adults andchildren to ease emotional issues that impact the abilityto function, to reverse or change troubling behavior andto assist with coping in times of personal crisis. Sessionsare covered up to 60 minutes; crisis sessions may extendup to 120 minutes. Family or conjoint psychotherapy: Therapy designed totreat the entire family. Regular sessions are covered up to90 minutes; crisis sessions may extend up to 180 minutes. Group psychotherapy: Therapy in which multiplepatients are treated together as a group. Sessions arecovered up to 90 minutes.Note: Certain mental health and SUD services may not beavailable overseas.This fact sheet is not all-inclusive. For additional information, go to www.tricare.mil.GLOBAL
T R I C A R E M E N TA L H E A LT H A N D S U B S TA N C E U S E D I S O R D E R S E R V I C E S Collateral visits: Collateral visits are not therapy sessions.These visits are used to gather information and to implementtreatment goals. Collateral visits are counted as individualpsychotherapy sessions and can last up to 60 minutes.You have the option of combining collateral visits withother individual or group psychotherapy visits.Note: Marriage counseling is not a TRICARE-covered benefit.PsychoanalysisPsychoanalysis is long-term mental health therapy that exploresunconscious thoughts to gain insights into behaviors andsymptoms. Treatment must be given by approved providerswho are specifically trained in psychoanalysis and alwaysrequires prior authorization.Suicide PreventionTRICARE urges beneficiaries to seek help duringtimes of difficulty. TRICARE offers mental health careservices for beneficiaries coping with mental healthissues, including those who have thoughts of suicide.If you or a loved one has suicidal thoughts, call theNational Suicide Prevention Lifeline at 1-800-273TALK (1-800-273-8255). To read about the warningsigns and steps you can take to help preventsuicide, visit www.tricare.mil/mentalhealth and clickon the “Programs and Resources” tab to find linksto Department of Defense and other resources formental health care and suicide prevention.Psychological Testing and AssessmentTesting and assessment are covered when medically orpsychologically necessary and provided in conjunctionwith otherwise covered psychotherapy or as a requiredpart of the assessment and reassessment process for appliedbehavior analysis under the Comprehensive Autism CareDemonstration. For more information about testing andassessment related to autism care services,visit www.tricare.mil/autism.Exclusions:Psychological testing must be medically or psychologicallynecessary and is not covered for the following circumstances: Academic placement Testing related to diagnosed specific learning disordersor learning disabilities2Job placementChild custody disputesGeneral screening in the absence of specific symptomsTeacher or parental referralsTesting to determine whether a beneficiary has a learningdisorder or learning disabilityMedication Assisted TreatmentMedication assisted treatment (MAT) combines drugand mental health therapies to treat a SUD. A TRICAREauthorized physician, physician assistant or nurse practitionermay provide MAT services. Eligible providers must have aspecial certification from the Drug Enforcement Agency toprescribe buprenorphine (for example, Suboxone ).MAT care is generally only available in the U.S. and U.S.territories. In overseas locations, see the host country’srequirements for practicing overseas providers.TRICARE covers the settings listed to provide MAT services:Opioid Treatment ProgramAn opioid treatment program (OTP) is recommended whena qualified mental health provider believes it is necessary toprovide a comprehensive, individually tailored program ofmedication therapy integrated with psychosocial and medicaltreatment and support services.1 Treatment in OTPs caninclude detoxification from opioids and medically supervisedwithdrawal from maintenance medications. OTP care isgenerally only available in the U.S. and U.S. territories.GLOBAL
T R I C A R E M E N TA L H E A LT H A N D S U B S TA N C E U S E D I S O R D E R S E R V I C E SOffice-Based Substance Use Disorder TreatmentOffice-based SUD treatment may be provided by TRICAREauthorized providers acting within the scope of their specificlicensure or certification to prescribe outpatient supplies toassist with detoxification and/or maintenance.2Telemedicine ServicesUnder some conditions, mental health services maybe provided via telemedicine services, which usessecure video conferencing to connect beneficiariesto providers. Telemedicine services has the samerequirements for referrals and prior authorizations asmental health care services.Overseas, see the host country’s specific licensure orcertification requirements for providers.Intensive Outpatient ProgramFor more information about telemedicineservices, contact your regional contractor or visitwww.tricare.mil/mentalhealth.An intensive outpatient program (IOP) is recommendedwhen a mental health provider believes it is necessary toprovide an organized day or evening program that includesassessment, treatment, case management and rehabilitationfor individuals who don’t require 24-hour care for mentalhealth and SUD.3 The program is regularly scheduled,individualized and shares monitoring and support with thepatient’s family and support system. IOPs provide at least sixhours of therapeutic services per week. Those services maybe provided during the day, evening, night or weekend.COVERED INPATIENT SERVICESAvailability, care access and referral and prior authorizationrequirements for inpatient services may vary by beneficiarytype, location and TRICARE program option. Refer to theGetting Care section of this fact sheet for details.Partial Hospitalization ProgramReferral and prior authorization is required for allnonemergency inpatient mental health care services.Psychiatric emergencies do not require prior authorization,but authorization is required for continued stay.Admissions resulting from psychiatric emergencies shouldbe reported to your regional contractor within 24 hoursof admission or on the next business day, and must bereported within 72 hours of an admission. Authorizationfor continued stay is coordinated between the inpatient unitand the regional contractor.A partial hospitalization program (PHP) is recommendedwhen a mental health provider believes it is necessaryto stabilize a critical mental health disorder that doesn’trequire 24-hour care in an inpatient psychiatric setting, orto transition from an inpatient program to an outpatientprogram.4 Those services may be provided during the day,evening, night or weekend. PHP care is generally onlyavailable in the U.S. and U.S. territories.Medication ManagementADSMs who get care at military hospitals or clinics do notrequire prior authorization.If you take prescription medications for a mental healthdisorder, you must be under the care of a provider who isauthorized to prescribe those drugs. Your provider will managethe dosage and duration of your prescriptions. Always ask yourprescribing provider what services are being provided.123The following rules apply: Facilities must be TRICARE-authorized.OTPs must agree to participate in TRICARE, which includes acceptingthe TRICARE reimbursement rate.The following rules apply: Providers must be TRICARE-authorized.Providers must possess the required host country credentials to prescribeoutpatient supplies that assist in detoxification and/or maintenance.Note: Certain mental health and SUD services may not beavailable overseas.34The following rules apply: Facilities must be TRICARE-authorized. IOPsmust agree to participate in TRICARE, which includes accepting theTRICARE reimbursement rate.The following rules apply: Facilities must be TRICARE-authorized. PHPmust agree to participate in TRICARE, which includes accepting theTRICARE reimbursement rate.GLOBAL
T R I C A R E M E N TA L H E A LT H A N D S U B S TA N C E U S E D I S O R D E R S E R V I C E SAcute Inpatient Psychiatric Care A patient may be referred to acute inpatient psychiatric careif the health care provider believes the patient has a mentalhealth disorder that threatens the patient’s physical well-beingor the well-being of others, to the extent that medical andpsychiatric care is needed on a 24-hour-a-day basis for safetyand stabilization. Acute inpatient psychiatric care may becovered on an emergency or nonemergency basis. Priorauthorization from your regional contractor is always requiredfor nonemergency inpatient admissions. In emergencysituations, authorization is required for continued stay.In an emergency, psychiatric inpatient hospitalizationmust first be sought. Admission primarily for substance use rehabilitation isnot authorized for psychiatric RTC care. Care must be recommended and directed by a TRICAREauthorized independent provider.Psychiatric Residential Treatment Center CareA psychiatric residential treatment center (RTC) providesextended care for children and adolescents who have mentalhealth disorders (SUD cannot be the primary diagnosis)requiring treatment in a therapeutic environment 24/7.Residential treatment may be required for children andadolescents who are stable enough to not require acute inpatienthospitalization, but do require a structured, therapeutic,residential setting to stabilize their condition so they canfunction at home and in an outpatient setting in the future.Psychiatric RTC care always requires a referral and priorauthorization, because psychiatric RTC placement is never apsychiatric emergency. Psychiatric inpatient hospitalizationshould be sought in a psychiatric emergency. PsychiatricRTC placement sometimes occurs after an inpatientpsychiatric hospitalization as a step-down level of care.Psychiatric RTC placement can also be a step-up level ofcare when a beneficiary can no longer function at home andin the community. The following rules apply: Facilities must be TRICARE-authorized, and must agreeto participate in TRICARE, which includes accepting theTRICARE reimbursement rate. Unless therapeutically contraindicated, the family and/or guardian should actively participate in the continuingcare of the patient through either direct involvement atthe facility or geographically distant family therapy. Prior authorization from your regional contractoris required. Psychiatric RTC care is not considered an emergency.4Note: Psychiatric RTC care is only covered for beneficiariesuntil reaching age 21.INPATIENT AND RESIDENTIAL SUBSTANCEUSE DISORDER REHABILITATIONFACILITY CARETRICARE only reimburses the cost of a care if you visit aTRICARE-authorized institutional provider. A TRICAREauthorized institutional provider is defined as an authorizedhospital or dedicated substance use disorder rehabilitationfacility (SUDRF). This can be either a freestanding facility orlocated inside a hospital.Inpatient Management of Withdrawal Symptoms(Detoxification)TRICARE covers emergency and inpatient hospitalservices for the treatment of the acute phases of substanceuse withdrawal (detoxification) when the patient’s disorderrequires the personnel and facilities of a hospital or SUDRF.You need prior authorization for non-emergency inpatienthospital or SUDRF services.Residential Substance Use Disorder RehabilitationPreauthorization is required for inpatient/residential SUDRFlevels of care. Your TRICARE regional contractor may haveadditional authorization requirements.GLOBAL
T R I C A R E M E N TA L H E A LT H A N D S U B S TA N C E U S E D I S O R D E R S E R V I C E SEXCLUSIONSGETTING CAREThe following mental health care services are not coveredunder TRICARE. This list is not all-inclusive.Emergency Care Aversion therapy Biofeedback for psychosomatic conditions Custodial care TRICARE defines an emergency as a serious medicalcondition that the average person would consider to be athreat to life, limb, sight or safety. In an emergency, call 911or go to the nearest emergency room. If you need emergencycare overseas, go to the nearest emergency care facility or callthe Medical Assistance number for the area where you arelocated. Referrals and prior authorizations are not requiredfor emergency care.Mental health care services and supplies related solely toobesity and/or weight reductionCounseling services that are not medically necessary inthe treatment of a diagnosed medical conditionADSMs who are admitted for emergency care should workwith the facility to get a continued-stay authorization fromtheir military hospital or clinic primary care managers (PCMs),Defense Health Agency—Great Lakes or TRICARE OverseasProgram (TOP) Regional Call Centers within 24–72 hoursof admission.Educational programsExperimental proceduresMarathon therapyMegavitamin or orthomolecular therapyPsychological testing and assessment as part of anassessment for academic placement. This exclusionencompasses all psychological testing related to educationalprograms, issues or deficiencies; or testing to determinewhether a beneficiary has a learning disability if theprimary or sole basis for the testing is to assess for alearning disability.When non-ADSMs are admitted for emergency care, theirPCMs, regional contractors or TOP Regional Call Centersshould be notified within 24–72 hours of an admission.If an emergency care admission occurs while travelingoverseas, beneficiaries should contact their PCMs or TOPRegional Call Centers before leaving the facility, or within24 hours or on the next business day.Psychosurgery (Surgery for the relief of movement disordersand surgery to interrupt the transmission of pain alongsensory pathways are not considered psychosurgery.) Services and supplies not medically or psychologicallynecessary for the diagnosis and treatment of acovered condition Sexual dysfunction therapyNonemergency CareFor nonemergency care, your PCM or primary care providercan provide an initial assessment and possibly treatment,and they can refer you to an appropriate mental health careprovider, if necessary.Therapy for developmental or learning disorders, suchas dyslexia, developmental mathematics disorders,developmental language disorders and developmentalarticulation disordersADSMs should always seek nonemergency mental health careat military hospitals or clinics first. ADSMs must always getreferrals and prior authorizations before getting civilian carefor nonemergency services.All other TRICARE Prime beneficiaries should seek care fromTRICARE network providers. If you seek nonemergency carefrom a TRICARE-authorized non-network provider withouta referral from your PCM, your care will be covered under thepoint-of-service (POS) option at higher out-of-pocket costs.555The POS option does not apply to ADSMs, newborns or newly adoptedchildren in the first 60 days after birth or adoption, emergency care,clinical preventive care from a network provider, beneficiaries with otherhealth insurance to a network provider for a medically diagnosed andcovered condition.GLOBAL
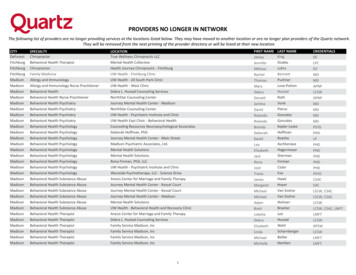
T R I C A R E M E N TA L H E A LT H A N D S U B S TA N C E U S E D I S O R D E R S E R V I C E STRICARE Select beneficiaries may see any TRICAREauthorized provider, but will minimize out-of-pocket costsby visiting TRICARE network providers.A physician referral and supervision is always required to seepastoral counselors and may be required to see mental healthcounselors. Contact your regional contractor to find out ifa mental health counselor requires physician referral andsupervision before getting services.Nonemergency inpatient admissions (including residentialsubstance use disorder treatment) and RTCs always requireprior authorization. Contact your regional contractor forprior authorization requirements. For a list of TRICAREauthorized network and non-network providers, visitwww.tricare.mil/findaprovider. To coordinate referrals andprior authorizations overseas, TOP Prime beneficiariesshould contact their PCMs or military hospitals or clinics.LOOKING FORMore Information?TOP Prime Remote beneficiaries should contact their TOPRegional Call Centers.COSTSADSMs have no costs for mental health care from or authorizedby the Military Health System. Non-ADSMs can minimizecosts by seeking care at military hospitals or clinics, whenavailable, or from TRICARE network providers. TRICAREPrime active duty family members may get nonemergencycare from TRICARE-authorized non-network providerswithout referrals, but POS fees apply.For more information and specific cost details,visit www.tricare.mil/costs.GO TOwww.tricare.mil/contactusTOP Regional Call CentersEurasia-AfricaTRICARE East RegionTRICARE Overseas Program (TOP)Humana e-east.comInternational SOSGovernment Services, Inc.www.tricare-overseas.comFor toll-free contact information,visit this website. 44-20-8762-8384 (overseas)1-877-678-1207 (stateside)tricarelon@internationalsos.comLatin America and Canada 1-215-942-8393 (overseas)1-877-451-8659 (stateside)tricarephl@internationalsos.comPacific (Singapore):Health Net Federal Services, LLC1-844-866-WEST (1-844-866-9378)www.tricare-west.comPacific (Sydney): 61-2-9273-2710 (overseas)1-877-678-1209 (stateside)sydtricare@internationalsos.comAn Important Note About TRICARE Program InformationAt the time of publication, this information is current. It is important to remember that TRICARE policies and benefits are governed bypublic law and federal regulations. Changes to TRICARE programs are continually made as public law and/or federal regulations areamended. Military hospital and clinic guidelines and policies may be different than those outlined in this publication. For the mostrecent information, contact your TRICARE regional contractor or local military hospital or clinic. The TRICARE program meets theminimum essential coverage requirement under the Affordable Care Act.TRICARE is a registered trademark of the Department of Defense, Defense Health Agency. All rights reserved.F S130 4BE T01191WTRICARE West Region 65-6339-2676 (overseas)1-877-678-1208 (stateside)sin.tricare@internationalsos.com
Note: Marriage counseling is not a TRICARE-covered benefit. Psychoanalysis Psychoanalysis is long-term mental health therapy that explores unconscious thoughts to gain insights into behaviors and symptoms. Treatment must be given by approved providers who are specifically trained in psychoanalysis and always requires prior authorization.