Transcription
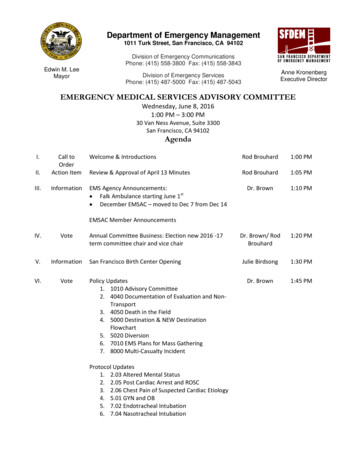
Department of Emergency Management1011 Turk Street, San Francisco, CA 94102Division of Emergency CommunicationsPhone: (415) 558-3800 Fax: (415) 558-3843Edwin M. LeeMayorAnne KronenbergExecutive DirectorDivision of Emergency ServicesPhone: (415) 487-5000 Fax: (415) 487-5043EMERGENCY MEDICAL SERVICES ADVISORY COMMITTEEWednesday, June 8, 20161:00 PM – 3:00 PM30 Van Ness Avenue, Suite 3300San Francisco, CA 94102AgendaI.Welcome & IntroductionsRod Brouhard1:00 PMII.Call toOrderAction ItemReview & Approval of April 13 MinutesRod Brouhard1:05 PMIII.InformationEMS Agency Announcements: Falk Ambulance starting June 1st December EMSAC – moved to Dec 7 from Dec 14Dr. Brown1:10 PMDr. Brown/ RodBrouhard1:20 PMJulie Birdsong1:30 PMDr. Brown1:45 PMEMSAC Member AnnouncementsIV.VoteV.InformationVI.VoteAnnual Committee Business: Election new 2016 -17term committee chair and vice chairSan Francisco Birth Center OpeningPolicy Updates1. 1010 Advisory Committee2. 4040 Documentation of Evaluation and NonTransport3. 4050 Death in the Field4. 5000 Destination & NEW DestinationFlowchart5. 5020 Diversion6. 7010 EMS Plans for Mass Gathering7. 8000 Multi-Casualty IncidentProtocol Updates1. 2.03 Altered Mental Status2. 2.05 Post Cardiac Arrest and ROSC3. 2.06 Chest Pain of Suspected Cardiac Etiology4. 5.01 GYN and OB5. 7.02 Endotracheal Intubation6. 7.04 Nasotracheal Intubation
VIII.VoteAmbulance Turnaround: Data policy review Vote on whether to continue with tracking.Dr. Brown/Libbie Bessman2:15 PMIX.InformationSpecial Event Medical Plans – Website DemonstrationAram Bronston2:30 PMX.InformationEMS Core Measures ReportJohn Brown2:40 PMXI.InformationItems from the PublicRod Brouhard2:55 PMXII.Action ItemAdjournmentRod Brouhard3:00 PMContact Mary Magocsy at 487-5019 or mary.magocsy@sfgov.org for questions regarding the meeting.2
EMERGENCY MEDICAL SERVICES ADVISORY COMMITTEEWednesday, April 13, 20161:00 PM – 3:00 PM30 Van Ness Avenue, DPW ClassroomSan Francisco, CA 94102MinutesItemDiscussionActionI. Welcome &IntroductionsCommittee Chair, Rod Brouhard, called the meeting to order. Quorumpresent.Meeting called toorder at 13:00II. MeetingMinutesMinutes from Dec 19, 2015 EMSAC meeting reviewed. Corrections togrammatical error and name misspelling requested.III. AnnouncementsEMS Agency Announcements: Several new policy updates will go out for public comment soon.Will include changes to Destination/Diversion policies updates toprotocols to accommodate changes in 2015 AHA ALS Guidelines.th EMS Awards are on May 19 at City Hall with Bd of Supervisors.Submit nominations by April 19. SFFD now has their cloud-based ePCR system up and running fortransmission of their ePCRs to the EDs. Pediatric Disaster Response & Emergency Preparedness course atUC Mission Bay June 2 -3. Dr. Brown noted that the all EMS Agencies in California submit datato the state for the “Core Measures” project. Noted that SF doeswell in some EMS performance measures and less well in others.Will report on the Core Measures in future meetings.Minutes approvedwith minorcorrections.New policy publiccommentdistribution at endof April.EMSAC Member Announcements None.IV. Strategies toInnovateEmeRgENcyCare ClinicalTrials (SIREN) –NIH NeuroStudy ProposalClaude Hemphill, MD, Chief Neurology at SFGH: V. HospitalDiversion PublicDataDashboardsSIREN is a proposed network for national emergencymedicine clinical research. Goal is to put together a nationalnetwork of hospitals and pre-hospital systems that willconduct large clinical trials of emergency treatments forneuro, cardiac, pulmonary, trauma, and others. Organizationof SIREN is via a hub-spoke system where a regionalcoordinating center (Hub) will work with several otherhospitals (Spokes) to conduct these clinical trials. The specifictrials to be conducted under SIREN have not yet beendetermined.UCSF/SFGH is submitting a proposal to serve as a regionalHub. UCSF/SFGH already has substantial experience doingthis type of work through the NETT network and many otherclinical trials (e.g. RAMPART that compared Lorazepam vs.Midazolam for treatment of pre-hospital status epilepticus).Need support from all EMS system participants (ambulanceproviders, hospitals, etc.). Letters of support are non-binding.Heather Littleton & Celeste Berg – SF Controller’s Office: SF Controller’s Office has a Performance Audit Unit that providesinternal management consulting and technical assistance to citydepartments to improve efficiency of city services. They have beenHospitals shouldcontact SFFD to getset up to receivetransmitted SFFDePCRs.Submit EMS Awardsnominations byApril 19.Course flyer on PediDisaster coursedistributed.Contact Dr Brown orDr Hemphill foradditionalinformation oraddress letters ofsupport to them.Motion approved.Diversion dashboards to go live in1-2 weeks.
ItemDiscussion working with EMS on improving EMS response times. Also createdpublic data dashboards that displays and compares EMS responseperformance. Now goal is to look at hospital diversion.Diversion public data dashboard demonstrated. Dashboard hadsection on the destination and diversion policies to give context tohospital diversion data (called a “storyboard” in website lingo) thatwill explain what the numbers mean. Dashboard uses rolling 13month that is updated monthly when it goes live. Source ofdiversion data is the monthly EMS Agency diversion reportsActionEmail notificationwill be done whenthe site is live.Group comments included: Diversion is complex issue due to supply-demand mismatch. EDs do not control diversion, it’s also a hospital issue. Changelanguage on website to reflect that. Destination “pyramid” is not accurate. Need to add explanation. Need to get health educator to bring down the reading level of thewebsite so the general public will understand it. Diversion suspension is a system problem not a proxy metric. There are 2 scales presented on the diversion suspension graph – donot include if they are not statistically related.Motion proposed to go ahead with posting the diversion public datadashboards and to do any “tweeks” based on experience with publicreaction at future EMSAC meetings.VI. AmbulanceTurnaround –Data UpdateLibbie Bessman was not able to present ambulance turnaround data dueto recent changes in the ambulance provider ePCR software. Libbieasked if there were any anecdotal reports of issues with obtaining theambulance turnaround data. One ambulance company noted a 50% compliance rate with gettingthe RN signature on the pre-hospital ePCR.VII. RTT MobileLanguageInterpretationJeff Munks, RTT Mobile demonstrated smart phone application forhands free language interpretation. Application had noise cancellationfeature that filters out loud ambient noise to minimize disruptions inlanguage interpretation between professional interpreters andemergency personnel.VIII. ZuckerbergSFGH OpeningDr. Mercer presented:st Opening May 21 . New name is Zuckerberg San Francisco GeneralHospital (abbreviation is ZSFG). New ED had larger floor plan; more beds; 2 CT scanners in theresuscitation area; allow for bedside triage; required keypad accessto ED, etc. New Carepoint system at Base Hospital will improve datacapture.nd New ambulance entrance on 22 Street. PES patients will still gothrough old ED entrance. New hospital has fewer med-surg beds, but more critical care beds. Questions raised about the impact of the lower med-surg in-patientcapacity and impact on diversion. Dr. Mercer and Jeaux Rinehardt noted that hospital leadership isaware. Hospital staff have been working on improving throughputprocesses especially focusing on lower acuity patients.2At June meeting,will review data andpolicyimplementation andvote whether tocontinue datacollection.RTT mobilehandoutsdistributed.Opening date onstMay 21 at 0700hrs.Final details oftransition for incoming EMSpatients will beannounced.ED Open House on4/26 and 4/28.MCI exercise onthMay 12 .
ItemDiscussionActionIX. ProjectSenoia –Database forSpecial EventMedical PlansAram Bronston presented on new database for special event medicalplans. Noted EMS receives 1,000 plans/year. On-line database willcentralize submission, approval and dissemination of event medicalplans. Will allow for public access. Have additional features such asgeospatial mapping.Special Eventmedical planwebsite goes live onstJuly 1 .X. Items fromthe PublicTheresa Farina noted that CPR and AED Awareness Week is June 1 – 7 .This is an opportunity for organizations to host public CPR trainings orother related public promotional events.CPR AwarenessWeek materials willbe emailed out.XI.AdjournmentRod Brouhard ended meeting at 1500 hours.Next meeting:Wed. June 8, 2016from 1300 – 1500hrs.thSan Francisco EMS Advisory Committee MembersBolded names present at meetingOrganizationZSFG - Base HospitalZSFG - TraumaSFFD Medical DirectorSFFD EMSDept Emergency CommunicationsCPMC: Pac, Davies, St Lukes, CalChinese HospitalKaiser San FranciscoKaiser South San FranciscoSt. Mary’s Medical CenterSt. Francis Memorial HospitalSeton Medical CenterUCSFUCSF-Mission BayVA Medical CenterAmerican Medical ResponseBayshore AmbulanceKing-American AmbulanceNorCal AmbulancePro Transport-1 AmbulanceSt. Joseph’s AmbulanceSF Emergency Physicians Assoc.City College Paramedic Training ProgramDept. Public HealthSF ALS Field ProviderSF BLS Field ProviderPublic RepresentativePediatric AdvisorResearch CoordinatorEMS FellowEMS FellowGuest NameDavid MalmudPrimary RepresentativeAlternate RepresentativeSue PetersonClement YehJeff MeyersClement YehLisa DuffyAnnette WilliamsScott CampbellRaymond HanMichael ThomasCarl RowlandMichael CohenChristopher RuckmanBarbi FeldhauserEvangeline RicoBrad WhiteDavid BockholtJosh NultemeierSteven ColmanChad ArchilaRichard AngottiMickey RokeachMegan CorryNaveena BobbaJoshua SmithRyan SeymourTheresa FarinaDavid StaconisOpenTony MolloyAnnette GoleyPatti TaylorStuart FongTimone MikkoRebecca SymmonsOpenWes VickroySeraphin CoLaura JacobsonRajesh DaftaryJonathan GarberRod BrouhardJeff DelmarMelyssa FarmerDan BobierJames MacadangdangJim PointerOpenJimmy ChoiCindy LambdinAndrew ChristophersonOpenRichard PekelneyMary MercerRajesh Daftary, MDPrasanthi Govindarajan, MDBrian Savino, MDEric Silverman, MDOrganizationAMR3Sharon KennedyEMSA StaffJohn Brown
Kameron DirksLaura DempseyDoug WalshHeather LittletonCeleste BergBen TannerMaria LunaBrendan MartinezJeff MunksJulie BirdsongJeaux RinehardtDoug WalshPeg StevensonChris BonnSrihari NamfeumalClaude HemphillFern CudlipAMRMedtronicsDPHSF Controller’s OfficeSF Controller’s OfficeDPHDept Emergency CommunicationsCity College Paramedic Training ProgramRTT MobileSF Birth CenterZSFGDept. Public HealthSF Controller’s OfficeSFFDUCSFUCSFUCSF4Mary MagocsyAram BronstonMike DaytonElizabeth (Libbie) BessmanCrystal Wright
Public Comment Response EMSAC meeting June 8, 2016Policy evisionsRemoved San Francisco ParamedicAssociation.Added UCSF Mission Bay, Falk Ambulance,and NorCal Ambulance Edit out or alter the SFPA in the Trauma subcommittee membership list [TSAC] on page 4;appendix A: “Falck” spelling ‐ page 6;appendix B: Seton and Kaiser SSF are listed twice, just keep the ones annotated as being inSan Mateo County? ‐ page 6; appendix C: note that UCSF receiving center is the Parnassus campus ‐ page 7‐Jeffrey Delmar, Bayshore AmbulanceMedical Director ResponseSFPA has ceased operations. Will remove frompolicy.Agree with all other comments.TSAC: SFPA representative still shows on the membership. We look forward to representing theEMS education community on the advisory committee.‐Megan Corry, CCSF Paramedic Program4040Documentationof Evaluationand NonTransportRevised to allow EMTs from [USF}on‐campus Emergency Medical Responseservices to allow patients to refuse transportwith 100% on‐line involvement of BaseHospital Physicians.Section III Policies and Procedures. B .3. I. Witness Signature if Available. Does this person needto be defined or can it be anyone at scene? Does the campus Department of Public Safety, in thepolice role, constitute a witness? A Resident Advisor or Faculty?Added a definition for who is considered apatient.Section III. AMA. E. 3. (over the phone) consider [over the phone or electronic device (tablet orcomputer)].‐Octavia Struve, USFWe will specify that a witness is a third party personwho is not a patient or a provider.Minor edit done.Section III. Patient Refusal. C. 3. "if they refused" consider "if they refuse"Need to clarify whether “over the phone orelectronic device” is referring to the Base Physicianconsultation. 3.m. spelling “determined” ‐ page 4 [add the ‐d]; o. spelling “members’ ” ‐ page 4 [add the possessive apostrophe]; p. spelling “paramedics’ “ ‐ page 4 [add the possessive apostrophe] C.3. spelling “if they refused” ‐ page 4 [delete the ‐d]‐Jeffrey Delmar, Bayshore AmbulanceMinor edits done. “Flag downs” are covered by an “individual who self‐identifies.”Definition of patient: does this include “flag down”? (i.e. it reads as though they must call911 to be considered a patient) B.3.m) typo should say “determined” not “determines” Recommend using the national standard terminology “EMT” and “Paramedic” (instead ofEMT‐B and EMT‐P) E. 3. 11) suggest deleting or specifying since an ALS intervention could include treat andrelease patients (ex. Hypoglycemic episode with resolution after dextrose)‐Megan Corry, CCSF Paramedic ProgramMinor edit done.Agree with just using Paramedic and EMT. NOTE:Will replace EMT‐P with paramedic and EMT forEMT‐B in the final version.Agree with deleting ALS intervention.
A clear difference between "PDT" criteria vs "AMA" criteria would be welcome. The currentpolicy is vague on PDT.The "two medic rule" that states two paramedics must sign off on an AMA, in addition tobase contact, that was put in place as I understand as a reaction to a bad outcome with onemedic's bad decision, is difficult to follow. As you know most of our medic ambulances arestaffed by one medic and one EMT. An AMA often involves waking up a medic engine in themiddle of the night just to obtain the second signature, and the engine medic perhapsdoesn't do a thorough assessment of the patient. Many medics feel one medic along withbase contact would be sufficient to sign an AMA. It is explained in the academy as, A PDT isa patient that you don’t anticipate having the need for any ALS intervention or assessment ifthey go to the hospital. An AMA is for a patient that you do anticipate ALS interventions orassessments (X‐rays, medications, etc) or a patient that has had some level of ALS care priorto arrival (D‐50 for hypoglycemia by engine medic, etc). Please define the difference betterbetween the two.Proposed Changes in 4040 concerns: EMT AMA – ? Every patient needs an ALSassessment Proposed definition of a patient.‐Joshua Smith, SFFDIII DefinitionThank you for developing a definition of a patient in our system. It is much needed.I would also suggest modifying a “or for whom the 911 system has been activated” type clausebelow with some formatting clarificationA Patient: ‐ An individual with a presumed need for acute medical care or evaluation, and:1) Identifies him/herself as needing emergency medical care2)Has activated an EMS response by requesting medical assistance or3)is identified by another party (including EMS providers) as needing emergency medicalcareIV, B Documentation: Consider adding:“Receiving hospitals shall maintain the capability to receive PCR documentation in an electronicformat”IV, B, Section 3, l‐pThe witness signatures seem inconsistent with the following section on AMA refusals.If two EMT‐Bs can perform an AMA refusal with BHMD involvement, should an EMT‐P(potentially with an EMT‐B partner) be required to have a second paramedic called to scene?Personally, I feel comfortable with a single paramedic evaluation accompanied by BHMDconsultation without second paramedic signature.IV, DAny person at the scene of a prehospital emergency who requested an EMS response, or for2Unclear on 2nd bullet comment. Will clarify atEMSAC meeting whether this references a lifethreatening condition or minor medical condition.The intent is that life threatening conditions requireBase Hospital contact.Need clarification on comment in last bullet.Agree with improving the definition. Will discussyour suggestion at the EMSAC meeting.Agree with requiring hospitals to have thiscapability. However, this belongs in Policy 5010Receiving Hospital Standards.Will discuss your suggestion at the EMSAC meeting.Agreed with your suggestion and added to policy.
whom an EMS response was requested and who presents with one or more of the followingconditions shall be considered incapable of making a competent decision regarding refusal ofmedical care and, when safe to do so, shall be transported to the closest appropriate medicalfacility for further evaluation:Added clarification language regarding refusal and safety of transporting patients against theirwishes.‐Clement Yeh, SFFD40504051Death in theFieldDo NotResuscitateRevised to include the use of End Tidal CO2devices to assist paramedics with cessationof resuscitation decisions.3.b, 4. Presence of documentation describing a patient’s desire to refuse resuscitation as part ofend‐of‐life care under California AB 15: End of Life Act”‐Clement Yeh, SFFDTHIS POLICY WAS NOT SENT OUT FORPUBLIC COMMENTThis one always generates a lively discussion during academies. In section "E" line "3" itstates: "If a DNR directive is not present at the scene, but a person who is present and who canbe identified as an immediate family member or spouse requests no resuscitation and has the fullagreement of any others who are present on scene, resuscitation may be withheld or stopped if ithas already been initiated"Added DNR form.Policy 4051 DNR details which documentation isconsidered valid for prehospital DNRs. Will updatethis policy in the next set of revisions.This policy was not sent out for public comment.Response to comment will be deferred to a nextrevision.Then a few lines down on section K line 1. it states, "EMS personnel may not rely solely on averbal assertion that a DNR directive exists."The policy on section "E" is I assume intended forthe 80 year old with a multitude of medical problems, not for the 60 year old male with a 25year old wife, however the two lines are confusing to our medics who have to decide whichpolicy to abide by. I've been telling them all, "When in doubt call base" but some clarificationwould be welcome.‐Joshua Smith, SFFD5000 /5000.1DestinationPolicy and ChartCriteria for Obstetrical Receiving Centershave been updated to include all complaintsthat are not subject to other medical needcriteria (e.g. trauma or stroke) for pregnantpatients with known gestational age of 20weeks or greater. Like all specialty centers,patients may be transported throughambulance diversion to these centers.Added new category of Sexual Suggested edits: “ transported to the closest a Pediatric Critical Medical receivinghospital ” ‐ page 3 [add the word receiving];2. “. to a Pediatric Critical Medical receiving hospital ” [2 places] ‐ page 3 [add the wordreceiving];chart‐‐main list: spelling fixes: St. Mary’s; St Luke’s [add possessives]specialty care list: Stroke: spelling fixes: St. Mary’s; ZSFG; UCSF‐ParnassusSTEMI: spelling fixes: St. Mary’s; UCSF‐ParnassusOB: spelling fixes: St. Luke’s; ZSFGHReimplantation: spelling fixes: ZSFGH;[in general, overall fixing of SFGH to ZSFG and noting when UCSF refers to Parnassus or3Minor edits done.Moved STAR criteria to follow adult and pedimedical criteria.
Assault/Sexual Abuse Receiving Center forpatients who self‐identify as being victims ofthis type of violence within the 72 hoursprior to presentation and are not subject toother medical need criteria (e.g. trauma orburn). Like all specialty receiving centers,patients may be transported throughambulance diversion to these centers.Added new category of LVAD Center.Revised destination table to a destinationflow chart.Mission Bay]add “h. sexual assault” to the list of specialty care services ‐ page 2 [also for IX.A.2. list] ‐page 6‐Jeffrey Delmar, Bayshore Ambulance IV. L. Obstetrics: typo should say “medical”Flowchart: Under Specialty care I see three different designations for the new SFGH. Undertrauma (and most others) it’s called ZSFG, under Stroke it’s ZFG, and under OB andReimplantataion it’s ZFGH.‐Megan Corry, CCSF Paramedic ProgramThe schematic is a little hard to follow, I only see a couple of holes, one is the STAR center alsoneeds to read, for any ongoing arrest being transported to a STAR center only, not justROSC/STEMI and SFGH is still a reimplantation center?.‐Chris Bonn, SFFDAdd LVAD destination.‐Josh Nultemeir5020DiversionDecreased the diversion suspension periodfrom 6 hours to 4 hours.Add NEW diversion category for InternalDisaster defined as when a hospital iscompletely closed to ALL patientstransported via 911 ambulance due to acompromised specialty center function ORwhen an internal disaster status withHospital Incident Command System (HICS) isactivated.7010EMS Plans forMass GatheringsAgree. Added to the policy. UCSF Parnassus andCPMC Pacific Campus are the only two hospitals thatoffer this treatment. We can designate them.Revised to require a basic disaster plan andminimum MCI supplies be present for allmass gatherings of a certain size or nature.AGREE V. typo should say “Diversion” VIII. Suggest spelling out “DEC” first time it is used and then using the acronym thereafter.‐Megan Corry, CCSF Paramedic ProgramNo comments received.No comments received.Revised Guidelines for Medical Resouces inSpecial Events table to improve clarity forrequirements vs. recommended resources.4
8000MultiCasualtyIncidentAutomatic (default) patient distributiontable has been changed to reflect theincreased capacity at SFGH to take categoryred trauma patients (10) and the addition ofthe UCSF Mission Bay Hospital to take thesame patient load as other communityhospitals, with a preference for pediatricMCI patients.Distribution chart: ZSFG immediate red 1st 104? 10? 4? major trauma [is it ZSFG or SFGH?][looks like it should be 10, but unclear ]‐Jeffrey Delmar, Bayshore AmbulanceNew appendix has been added to reflect thepatient tracking information needed forhospitals to complete within 24 hours of theconclusion of an MCI.5It is 10 (ten) red patients.
SAN FRANCISCO EMERGENCY MEDICAL SERVICES AGENCYPolicy Reference No.: 1010Effective Date: September 9XXXX, 20163Supersedes: September 9, 2013August 1, 2012ADVISORY COMMITTEESI.PURPOSETo define the roles, structure, membership and procedural standards for advisorycommittees to the EMS Agency Medical Director.II.POLICYA. Advisory committees, composed of EMS system constituents, shall convene to reviewEMS system issues relevant to their scope of responsibility and recommend actions tothe EMS Agency Medical Director concerning matters of policy, procedure, andprotocol.B. The EMS Agency Medical Director, as mandated by state statute, provides medicalcontrol and assures medical accountability throughout the planning, implementationand evaluation of the EMS System. The EMS Agency Medical Director retains the finaldecision through his/her medical authority for the EMS system.III.OPEN PUBLIC MEETINGSA. All committee and sub-committee meetings are open to members of the public.Meeting agendas, minutes, and other documents pertaining to these committees,except quality improvement documents, are public records and subject to public review.The EMS Agency shall distribute and post on its website an annual meeting schedule.B. The quality improvement portions of the EMS Advisory Committee and its subcommittees are closed meetings because of confidential patient information reviewedduring case discussions.IV.PARLIAMENTARY AUTHORITY / QUORUMA. Proceedings of the advisory committee and subcommittees are conducted under the“Robert’s Rules of Order” when they do not conflict with this policy. This policy shalltake precedence if any procedures are in conflict with “Robert’s Rules of Order.”B. A quorum is required to call the meeting to order and to transact committee business.A committee must maintain a quorum to continue a meeting. Specific quorumrequirements are listed in Section VII.Page 1Formatted: Highlight
Policy Reference No.: 1010Effective Date: XXXSeptember 9, 20163V.Formatted: HighlightCOMMITTEE MEMBERSHIPA. Representative organizations are listed the appendices to this policy. Committeemembers are nominated by their representative organization and appointed by the EMSAgency Medical Director to a two year term. Members may be re-appointed to theirposition with concurrence of the EMS Agency Medical Director and their organization.B. Members who do not attend three meetings within a year may be replaced in theirposition by the EMS Agency Medical Director.VI.COMMITTEE OFFICERSA. Each committee shall elect a Chair and Vice-Chair. The Chair of each committee shall calland preside over all meetings of that committee. The Chair shall develop the committeeagenda in consultation with the EMS Agency Medical Director. The Vice-Chair shallassume the duties of the Chair in their absence.B. Committee Chairs and Vice-Chairs serve a one year term from July 1 – June 30. At thelast meeting of each committee before July 1st, the members shall elect a Chair andVice-Chair. Chair and Vice Chair terms are effective at the first meeting of thatcommittee after July 1st. The committee may vote to extend their term once (for a totalof two years of consecutive service) if the current officers who wish to continue. Pastofficers are eligible for service again after three years from the end of their last term.C. This provision does not apply to the Trauma System Audit Sub-Committee, which hasthe Trauma Medical Director at San Francisco General Hospital as standing Chair.D. The EMS Agency will provide professional and clerical support to the advisorycommittees created by this policy.VII.STANDING ADVISORY COMMITTEE AND ITS SUBCOMMITTEESA. Emergency Medical Services Committee (EMSAC): The standing advisory committeethat is a multi-disciplinary forum for reviewing and making recommendations related tothe following: Prehospital clinical policies and treatment protocol issues involving FirstResponder, Basic Life Support, Advanced Life Support, interfacility transport,and/or critical care transport personnel in the San Francisco EMS system; General system management and operational policies includingcommunications, system performance, destination, ambulance diversion,and development of strategies to optimize the EMS System; Disaster medical emergency management, including mitigation,preparedness, response and recovery, andPage 2Formatted: Font: BoldFormatted: Font: 12 pt
Policy Reference No.: 1010Effective Date: XXXSeptember 9, 20163 Formatted: HighlightApproval of prehospital pilot and research projects.Meetings: Held five times per year in even numbered months or more frequently byrequest of the Committee Chair, vote of the committee, or the request of the EMSAgency Medical Director or his/her designee.Location: As set by agendaEMS Agency Staff: Medical Director, EMS Administrator, EMS Agency SpecialistsQuorum: Consists of: 33% one of the representatives from the prehospital EMS organizationslistedorganizations listed under Appendix A. 33% one of the hospital organizations listed under Appendix B.Membership: Consists of the EMS Agency Medical Director (ex-officio) and oneprimary representative and one alternate representative from: Ambulance Provider Companies listed in Appendix A San Francisco Receiving Hospitals listed in Appendix B San Francisco Emergency Physicians’ Association San Francisco Paramedic Association City College of San Francisco - Paramedic Training Program San Francisco Department of Public Health San Francisco General Hospital Base Hospital Medical Director San Francisco Fire Department EMS Medical Director San Francisco Emergency Communications Department Medical Director Representative from at least one San Francisco approved paramedic trainingprogram. Paramedic field representatives currently accredited in San Francisco andworking for a permitted ambulance company appointed by the EMS AgencyMedical Director EMT field representatives currently certified in San Francisco and working ona permitted ambulance company appointed by the EMS Agency MedicalDirector Members of the public, not affiliated with a regulated provider organization,and appointed by the EMS Agency Medical Director.B. Trauma System Audit Subcommittee (TSAC): A standing subcommittee of the EMSAdvisory Committee that advises on trauma system policy. Its goals are the evaluationand administration of the trauma system with oversight responsibility for systemvulnerabilities, the development of policy and/or approaches to related issues such asPage 3Formatted: Font: 12 pt
Policy Reference No.: 1010Effective Date: XXXSeptember 9, 20163Formatted: Highlightmajor trauma and burn-related prehospital care, injury surveillance, trauma transfers,repatriation, and long-term outcomes.Meetings: Meets four times per year, coincident with dates of the EMS AdvisoryCommittee, or by request of the subcommittee Chair or the EMS Agency MedicalDirector.Location: As set by agendaEMS Agency Staff: EMS Medical Director, EMS Administrator and Trauma CoordinatorQuorum: Consists of: 33% one of the hospital organizations listed under TSAC Membership 33% one of the prehospital EMS organizations listed under Membership One representative from SFGH Trauma Center One representative from St. Francis Bothin Burn CenterFormatted: Font: 12 ptFormatted: Font: 12 ptMembership: Hereby consists of: EMS Agency Medical Director (ex-officio) Zuckberg San Francisco General Hospital Trauma Medical Director (ex-off
Edwin M. Lee Mayor Department of Emergency Management 1011 Turk Street, San Francisco, CA 94102 Division of Emergency Communications Phone: (415) 558-3800 Fax: (415) 558-3843