Transcription
Do Response TimesReally Matter?Matt Zavadsky, MS-HSA, EMTDirector of Public AffairsMedStar Mobile Healthcare, Ft. Worth, TXAdjunct FacultyUniversity of Central FloridaCollege of Health and Public Affairs
What we’re gonna do Figure out how we got “here” Review the science of clinical impact ofresponse times Focus on improving response times that matter Figure out how to ‘un-get’ here!
Disclaimer Response time discussions volatileCheck your weaponsSet your Phasers on ‘stun’Local community discussion!!Help them ‘look forward’ and ‘see beyond’
A Word About Texas
Where did this “Need forSpeed” come from
Cardiac Resuscitation in the CommunityImportance of Rapid Provision and Implications for ProgramPlanning Mickey S. Eisenberg, MD, PhD; Lawrence Bergner, MD, MPH; Alfred Hallstrom, PhD“If CPR was initiated within four minutes and if definitive care was provided within eightminutes, 43% of patients survived. If either time was exceeded, the chances of survival felldramatically.The time to initiation of CPR and definitive care are factors directly influenced by emergencymedical service program decisions.A realistic option to improve time to initiation of CPR is widespread citizen CPR training. Apossible option to improve the time to definitive care is the training of emergency medicaltechnicians in defibrillation.”
1979!!
What Matters? EMS has a history of “feel good”innovationsoWith little to no scientific basis Good thing we can change! MAST pants Water bumpers
Measuring What Matters Patient outcomes ooEMS is healthcareNeed to look at patient outcomes Risk vs. BenefitoIs faster really “better”? 74% of crashes occur while driving “HOT”
Consequences of Speed
Consequences of Speed
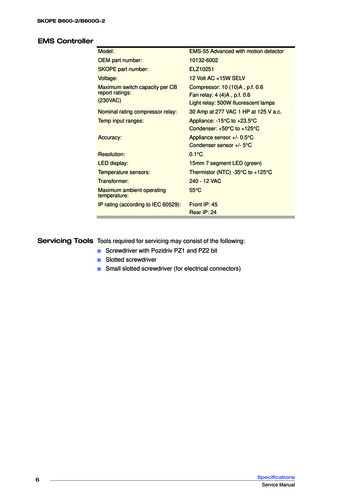
CAEMS StudyFractile,Average,BothHOTDavenport, IABoth7:59Fort Wayne, INFractile8:30Fort Worth, TXBoth9:0015:00Kansas City, MOFractile9:0020:00Little Rock, ARFractile8:5912:59Mecklenburg County, NCFractile10:5920:00Nova Scotia, CanadaFractile8:5914:59Pinellas County, FLFractile10:0020:00Reno, NVFractile8:2929:59Both8:5959:59Tulsa, OKFractile8:5912:59Oklahoma City, OKFractile8:5912:59LocationRichmond, VACOLD
The Current Science Paramedic Response Time: Does it affect patientsurvivaloo9,559 ‘unselected’ patientsUrban setting, DenverCONCLUSIONS:A paramedic response time within 8 minutes was not associated with improvedsurvival to hospital discharge after controlling for several important confounders,including level of illness severity. However, a survival benefit was identified when theresponse time was within 4 minutes for patients with intermediate or high risk ofmortality. Adherence to the 8-minute response time guideline in most patients whoaccess out-of-hospital emergency services is not supported by these results.Acad Emerg Med. 2005 Jul;12(7):594-600
The Current Science Lack of association between pre-hospital responsetimes and patient outcomesooo373 study patients 10:59Compared to 373 10:59 patientsUrban community – 750,000 - CharlotteCONCLUSIONS:Compared with patients who wait 10:59 minutes or less for ALS response,Priority 1 patients who wait longer than 10:59 minutes could experiencebetween a 6% increase and a 4% decrease in mortality, and do not have anincrease in critical procedures performed in the field. Our data are mostconsistent with the inference that neither the mortality nor the frequency ofcritical procedural interventions varies substantially based on this pre-specifiedALS RT.Prehosp Emerg Care. 2009 Oct-Dec;13(4):444-50
The Current Science Optimal defibrillation response intervalsfor maximum out-of-hospital cardiacarrest survival ratesoooPart of the OPALS Study9,273 treated cardiac arrest patients1991 - 1997
Study objective: Many centers optimize their (EMS) systems to achieve a targetdefibrillation response interval of “call received by dispatch” to “arrival at scene byresponder with defibrillator” in 8 minutes or less for at least 90% of cardiac arrestcases. The objective of this study was to analyze survival as a function of time totest the evidence for this standard.Results: Overall survival 4.2% (392 out of 9,273 cases worked). There was a steepdecrease in the first 5 minutes of the survival curve, beyond which the slopegradually leveled off. 9 minutes (4.6%; 18 lives) 8 minutes (5.9%; 0 lives) 7 minutes (7.5%; 23 lives) 6 minutes (9.5%; 51 lives) 5 minutes (12.0%; 86 lives)Conclusion: The 8-minute target established in many communities is not supportedby our data as the optimal EMS defibrillation response interval for cardiac arrest.EMS system leaders should consider the effect of decreasing the 90th percentiledefibrillation response interval to less than 8 minutes.Ann of Emerg Med Volume 42, Issue 2 , Pages 242-250, August 2003
The Current Science Response time effectiveness: comparison ofresponse time and survival in an urbanemergency medical services systemooooooCarolinas Medical System – 2002Urban county (620,000)10:59 RT standard for P1 calls5,424 transports studied71 did not surviveOf those:Acad Emerg Med. 2002 Apr;9(4):288-95.
Results:No significant difference in median RTs between survivors (6.4 min) andnon-survivors (6.8 min) was noted (p 0.10). “However, mortality riskwas 1.58% for patients whose RT exceeded 5 minutes, and 0.51% forthose whose RT was under 5 minutes (p 0.002). The mortality riskcurve was generally flat over RT intervals exceeding 5 minutes.Conclusion:In this observational study, emergency calls where RTs were less than 5minutes were associated with improved survival when compared withcalls where RTs exceeded 5 minutes. While variables other than timemay be associated with this improved survival, there is little evidence inthese data to suggest that changing this system's response timespecifications to times less than current, but greater than 5 minutes,would have any beneficial effect on survival.Acad Emerg Med. 2002 Apr;9(4):288-95.
The Current Science Eight minutes or less: does the ambulanceresponse time guideline impact trauma patientoutcomeoooEvaluate effect of exceeding the 8 min RT guideline onpatient survival for victims of traumatic injury treatedby an urban paramedic ambulance EMS system andtransported to a single Level I trauma center – Denver3,490 patients evaluatedPatients were grouped according to ambulance RT: or 8 min (n 2450) or 8 min (n 1040)J Emerg Med. 2002 Jul;23(1):43-8.
Results:After controlling for other significant predictors, there was nodifference in survival after traumatic injury when the 8 minambulance RT criteria was exceeded (mortality odds ratio 0.81,95% CI 0.43-1.52). There was also no significant difference insurvival when patients were stratified by injury severity scoregroup.Conclusion:Exceeding the ambulance industry response time criterion of 8min does not affect patient survival after traumatic injury.J Emerg Med. 2002 Jul;23(1):43-8.
What do the Eagles Think?EVIDENCE-BASED PERFORMANCE MEASURES FOR EMERGENCY MEDICALSERVICES SYSTEMS: A MODEL FOR EXPANDED EMS BENCHMARKINGA STATEMENT DEVELOPED BY THE 2007 CONSORTIUMU.S. METROPOLITAN MUNICIPALITIES’ EMS MEDICAL DIRECTORS“In many jurisdictions, response-time intervals for advanced life support unitsand resuscitation rates for victims of cardiac arrest are the primary measures ofEMS system performance.”“The association of the former with patient outcomes is not supported explicitlyby the medical literature, while the latter focuses on a very small proportion ofthe EMS patient population and thus does not represent a sufficiently broadselection of patients.”PREHOSPITAL EMERGENCY CARE 2008;12:141–151
“Over-emphasis upon response-time interval metrics may lead tounintended, but harmful, consequences (e.g., emergency vehiclecrashes) and an undeserved confidence in quality and performance ”“ much of the clinical research utilized to establish an acceptable“advanced life support (ALS) response time interval” was conducted in aperiod when only paramedics could operate a defibrillator, and thecompression component of basic cardiopulmonary resuscitation (CPR)received much less emphasis.”“Now that basic life support (BLS) providers and lay rescuers can providerapid automated defibrillation as well as basic CPR, the relativeimportance of the ALS response-time interval has been challenged, bothfor cardiac arrest as well as for other clinical conditions.”PREHOSPITAL EMERGENCY CARE 2008;12:141–151
“Many communities are still not measuring the intervals for themost important predictive elements for optimal outcome: timeelapsed until initiation of basic chest compressions and timeelapsed until defibrillation attempts.”PREHOSPITAL EMERGENCY CARE 2008;12:141–151
So What!? What is the ‘cost’ of insanityKeep doing the same thing and expecting adifferent outcomeo “It’s what the community wants ”oReally?
Well, maybe somecommunities overfocus on speed?
Time / Quality Tradeoff How do we reduce ALS response times?ooAdd more paramedics!Not a problem, right?
Back to the Eagles “As more paramedics are added to a particular system, however, thefrequency with which each individual paramedic has theopportunity to assess and manage critically ill or injured patients inthe primary or “lead” paramedic role may decrease.Pragmatically, considering that ALS cases constitute a small minorityof all EMS 9-1-1 responses, adding more paramedics into the systemmay actually reduce an individual paramedic’s exposure to criticaldecision-making and clinical skill competencies.”PREHOSPITAL EMERGENCY CARE 2008;12:141–151
Back to the Science The effect of paramedic experience onsurvival from cardiac arrestoExamine the relationship between the years ofexperience of paramedics and survival fromout-of-hospital cardiac arrest. Seattle – 2009oAll witnessed, out-of-hospital VF cardiacarrests (n 699) that occurred betweenJanuary 1, 2002, and December 31, 2006.Prehosp Emerg Care. 2009 Jul-Sep;13(3):341-4
RESULTS:“We found that every additional year of experience of the medic in chargeof implementing procedures such as intravenous line insertions,intubations, and provision of medications was associated with a 2%increase in the likelihood of survival of the patient (95% CI: 1.00-1.04). Thenumber of years of experience of the paramedic who did not performprocedures but instead was in charge of treatment decisions was notsignificantly associated with survival (odds ratio [OR] 1.01, 95% CI: 0.991.03). When we combined both paramedics' years of experience, we saw a1% increase in the odds of survival for every additional year of experience(95% CI: 1.00-1.03).”CONCLUSIONS:This study suggests that the amount of experience of the paramedic whoperformed procedures on cardiac arrest patients was associated withincreased rates of survival. However, we did not find an associationbetween survival from VF and the number of years of experience of theparamedic who made treatment decisions.Prehosp Emerg Care. 2009 Jul-Sep;13(3):341-4
Does the number of paramedics affectclinical benchmark thresholds?METHODS:This was a retrospective review of annual experience profilesfor paramedics working during 2001-2005 using the MCEMSpatient care record (PCR) database.The number of patient contacts, role as team leader/reportwriter, adult and pediatric endotracheal intubations, adultand pediatric intravenous (IV) access initiations, medicationadministration, and 12-lead electrocardiogram (ECG)acquisitions were analyzed. t-tests and descriptive statisticswere performed for comparison with the 1997 study.Prehosp Emerg Care. 2008 Jul-Sep;12(3):302-6
Results:Over the five-year study period, 1,215 paramedic profiles gleaned from107,524 PCRs documented a total of 297,900 patient contacts.The 1997 analysis (1987-1996 data) included 1,450 paramedic profilesrepresenting 467,559 patient contacts generated from 172,131 filed PCRs.All comparable experiences decreased significantly between the 1997analysis and the current study, except medication administration, whichincreased 25%.Conclusion:These data show a decreased opportunity and a wide variability in thefrequency of successfully completed paramedic technical skills andexperiences in this EMS system. Limited exposure to critically ill adult andpediatric patients reaffirms that high-risk skills are performed infrequently. Amultifaceted approach should be considered for maintaining providercompetency.
Emergency Medical Services Advance LifeSupport Response Times:Lots of Heat, Little Light“Looking beyond cardiac arrest, few clinical conditions can beidentified for which and ALS response standard seems warranted.The Emergency Medical Services Outcomes Project (EMSOP) identified seven clinical conditions that account for 65% of alladult EMS transports and seven that account for 85% of allpediatric transports.Of these, only cardiac arrest, the 2nd least frequent, appears torequire rapid EMS response.”Swor and Cone CommentaryAcad Emerg Med. 2002 Apr;9(4):320-1
“A wealth of literature has developed identifying the value of firstresponse and early defibrillation on cardiac arrest survival, thoughit is clear that this value varies from system to system.It may even be that an effective first-responder system cancompletely eliminate the need for ALS response time standards.Future efforts must focus on the incremental effect of ALS onsurvival after cardiac arrest and other time-sensitive clinicalentities.Communities need such data to create optimal response intervalstandards, decrease system costs, minimize lights-and siren driving,and evolve cost-effective EMS systems.”Acad Emerg Med. 2002 Apr;9(4):320-1
The MedStar Experience 48 hours of “COLD” responses in February2011oCohort of comparable patients from the weekbefore Chest Pain Stroke Trauma Alerts
Chest PainN 16 HOTResponseN 11 COLDResponseAvg. 1st Response Time04:0005:45Avg. MedStar Resp. Time07:3014:38Call to Destination Time39:3440:111.7 days1.6 days30.0%18.8%51.5 mins184.5 minsData PointALOSAdmit %Symptom Onset to 9-1-1 Access (Median)Very Preliminary Results awaiting peer review
ASM Analysis 0216660010482122324D/C 126/6/20127/15/2012Receiving FacilityJohn Peter Smith HospHarris Methodist - Fort WorthHarris Methodist - Fort WorthHarris Methodist - Fort WorthJohn Peter Smith HospHarris Methodist - Fort WorthHarris Methodist - Fort WorthJohn Peter Smith HospJohn Peter Smith HospHarris Methodist - Fort WorthHarris Methodist - Fort WorthHarris Methodist - Fort WorthHarris Methodist - Fort WorthHarris Methodist - Fort WorthHarris Methodist - Fort WorthHarris Methodist - Fort WorthHarris Methodist - Fort WorthHarris Methodist - Fort WorthHarris Methodist - Fort WorthHarris Methodist - Fort WorthHarris Methodist - Fort WorthHarris Methodist - Fort WorthHarris Methodist - Fort WorthJohn Peter Smith HospHarris Methodist - Fort WorthVital AliveAliveAliveAliveAliveAliveAliveAliveECG MISTEMISTEMISTEMISTEMI ; Other anterior AMI, st elevation STEMISTEMISTEMI
ASM Analysis (2012)1816Length of Stay 310:14:240:17:170:20:10Response TimeRegression-0.114647079
Priority Response January 27-28 2011 (No Ice)Run NumberResponse Times Chief 72931101273481101280591101282201101282386:02 mins9:08 mins7:08 mins6:27 mins5:22 mins6:35 mins6:26 mins4:08 mins8:00 MinsAVG resp. time6:48 MinsCardiac ArrestCardiac ArrestCardiac ArrestCardiac ArrestCardiac ArrestCardiac ArrestCardiac ArrestCardiac ArrestCardiac ArrestAgeOutcome76 Years59 Years63 Years78 Years73 Years50 Years50 Years83 Years58 YearsField TermDOS/No AttemptDOS/No AttemptPronounced in ERPronounced in ERDOS/No AttemptDOS/No AttemptField TermDOS/No AttemptSuspended Priority Response February 3-4 2011 (Ice)Run NumberResponse 11020409211020419511020440710:15 mins6:03 mins8:23 mins8:03 mins10:30 mins7:13 mins17:23 mins3:23 minsAVG resp time8:16 MinsChief Complaint AgeOutcomeCardiac ArrestCardiac ArrestCardiac ArrestCardiac ArrestCardiac ArrestCardiac ArrestCardiac ArrestCardiac ArrestField TermDOS/No AttemptPronounced in ERPronounced in ERDOS/No AttemptDOS/No AttemptPronounced in ERField Term76 Years51 Years3 Mos46 Years92 Years83 Years66 Years83 YearsVery Preliminary Results awaiting peer review
What does this all Mean? For improved clinical outcomes Very few EMS calls require immediateresponseo That time critical response is CPR/AEDo Measure call to CPR/AED times as clinicalbenchmark Invest in THAT process Use saved in a longer ALS response timeo
What does this all Mean? In some cases, the best response time isBEFORE the callooInvest in programs that PREVENT the callCommunity Health/CHF programs Or before dispatching the CalvaryoNurse Advice Triage systems (ECNS ) No such thing as an inappropriate requestoBut there is such thing as an inappropriateresponse to that request
What does this all Mean? Even with Chest Pain ooPatients wait too long to callInvest saved in longer ALS into publiceducation on NOT waiting Clinical PerformanceoooWe’re trading experience for speedLonger term issuesBetter to have an experienced medic in 15minutes vs. inexperienced in 7?
“Red Ink” Opportunities Allows organizations to take on issues thatmight otherwise be ‘undiscussable’Put down sacred cows that have outlived theirusefulnesso Has the “XX” response time standard outlivedit’s usefulness?o
“On Monday, Jan. 12, a leaner Cleveland EMS system emerged.Facing a 23 million city budget gap, the agency saw its ambulancesreduced from 18 to 15, and 13 positions eliminated, including sixlayoffs. Out of both necessity and a longstanding desire tomaximize its resources, the agency determined it would no longerautomatically dispatch an ambulance simply because someonedials 9-1-1.”February 2010
“Comprehensive call triage in the dispatch center forms thefoundation of the agency's new policy. Specific Bravo, Alpha andOmega calls are held until at least 10 ambulances are open andlife-threatening calls are addressed.An ambulance will not be dispatched at all for minor complaints(earaches and the like). However, the agency will provide thesecallers with appropriate referrals and contact numbers toagencies or clinics that can better assist them.”
2012 - The City of San José asked for an operationsefficiency diagnostic of three major departmentsPolice – Fire – Parks & Rec
Steve Athey Strategies forDealing with Dead Horses Buy a stronger whipAppoint a committee to study the horseSay things like, “This is the way we have always ridden this horse.”Change ridersArrange to visit other sites to see how they deal with dead horsesCreate a training session to increase the ability to ride dead horsesHarness several dead horses together for increased speedHave the CEO declare, “No horse is too dead to beat.”Form “quality circles” to find uses for dead horsesPromote the dead horse to supervisor
Moving the Needle Community relations issueoooPublic expectationWe created this problemWe have to fix it Begin the dialogue on “what matters”Now more than ever – communities may bewilling to listeno Budget issues across the U.S.o
Local Challenges?
Questions/Comments? Thank you for this privilege!!MZavadsky@medstar911.org
The Current Science Lack of association between pre-hospital response times and patient outcomes o 373 study patients 10:59 o Compared to 373 10:59 patients o Urban community -750,000 -Charlotte CONCLUSIONS: Compared with patients who wait 10:59 minutes or less for ALS response, Priori 1 pa en who wai longer an 10:59 minutes c ould experience


![MOH STANDARDS FOR EMERGENCY AMBULANCE SERVICE (2017) [Updated 21 Nov 2018]](/img/51/emergencyambulancestandards.jpg)