Transcription
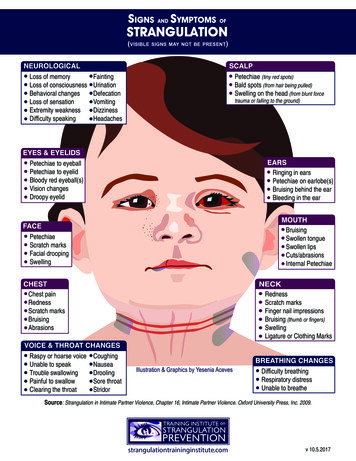
SIGNS AND SYMPTOMS OFSTRANGULATION(visible signs may not be present)Loss of memoryLoss of consciousnessBehavioral changesLoss of sensationExtremity weaknessDifficulty ssHeadachesPetechiae (tiny red spots)Bald spots (from hair being pulled)Swelling on the head (from blunt forcetrauma or falling to the ground)Petechiae to eyeballPetechiae to eyelidBloody red eyeball(s)Vision changesDroopy eyelidRinging in earsPetechiae on earlobe(s)Bruising behind the earBleeding in the earBruisingSwollen tongueSwollen lipsCuts/abrasionsInternal PetechiaePetechiaeScratch marksFacial droopingSwellingChest painRednessScratch marksBruisingAbrasionsRaspy or hoarse voiceUnable to speakTrouble swallowingPainful to swallowClearing the throatRednessScratch marksFinger nail impressionsBruising (thumb or fingers)SwellingLigature or Clothing MarksCoughingNauseaDroolingSore throatStridorIllustration & Graphics by Yesenia AcevesDifficulty breathingRespiratory distressUnable to breatheSource: Strangulation in Intimate Partner Violence, Chapter 16, Intimate Partner Violence. Oxford University Press, Inc. 2009.strangulationtraininginstitute.comv 10.5.2017
Diana Faugno MSN, RN, CPN, SANE-A, SANE-P, FAAFS, DF-IAFNDiana Faugno graduated with a Bachelor of Science in Nursing-University ofNorth Dakota and a Master of Science in Nursing-University of Phoenix. Ms.Faugno is a Founding Board Director for End Violence Against WomenInternational (EVAWI) She is a member of the Board of Directors for theCalifornia American Professional Society on the Abuse of Children.She is thecurrent president of the Acadmey of Forensic Nurses as well as a retired-fellow inthe American Academy of Forensic Science and a Distinguished Fellow in theInternational Association of Forensic Nurses. She currently is the nurse examinerat the Barbara Sinatra Childrens Center and a nurse examiner for EisenhowerMedical Center’s SART team. She is the co-author on numberous textbooks andpapers on dealing with the forensic medical aspects of violence.
RECOMMENDATIONS for the MEDICAL/RADIOGRAPHICEVALUATION of ACUTE ADULT, NON-FATAL STRANGULATIONPrepared by Bill Smock, MD and Sally Sturgeon, DNP, SANE-AOffice of the Police Surgeon, Louisville Metro Police DepartmentEndorsed by the National Medical Advisory Committee: Bill Smock, MD, Chair; Cathy Baldwin, MD; William Green, MD;Dean Hawley, MD; Ralph Riviello, MD; Heather Rozzi, MD; Steve Stapczynski, MD; Ellen Tailiaferro, MD; Michael Weaver, MDGOALS:1. Evaluate carotid and vertebral arteries for injuries2. Evaluate bony/cartilaginous and soft tissue neck structures3. Evaluate brain for anoxic injuryStrangulation patient presents to the Emergency DepartmentHistory of and/or physical examwith ANY of the following: History of and/or physical examwith: No LOC (anoxic brain injury) No visual changes: “spots”, “flashing light”,“tunnel vision” No petechial hemorrhage No soft tissue trauma to the neck No dyspnea, dysphonia or odynophagia No neurological signs or symptoms (i.e.LOC, seizures, mental status changes,amnesia, visual changes, cortical blindness,movement disorder, stroke-like symtoms) And reliable home monitoringLoss of Consciousness (anoxic brain injury)Visual changes: “spots”, “flashing light”, “tunnel vision”Facial, intraoral or conjunctival petechial hemorrhageLigature mark or neck contusionsSoft tissue neck injury/swelling of theneck/cartoid tendernessIncontinence (bladder and/or bowel from anoxic injury)Neurological signs or symptoms (LOC, seizures,mental status changes, amnesia, visual changes, corticalblindness, movement disorders, stroke-like symtoms.)Dysphonia/Aphonia (hematoma, laryngeal fracture,soft tissue swelling, recurrent laryngeal nerve injury)Dyspnea (hematoma, laryngeal fractures, soft tissueswelling, phrenic nerve injury)Subcutaneous emphysema (tracheal/laryngeal rupture)Discharge home with detailed instructionsto return to ED if:neurological signs/symptoms, dyspnea,dysphonia or odynophagia developsor worsensRecommended Radiographic Studies toRule Out Life-Threatening Injuries*(including delayed presentations of up to 6 months) CT Angio of carotid/vertebral arteries(GOLD STANDARD for evaluation of vessels and bony/cartilaginous structures, less sensitive for soft tissuetrauma) or CT neck with contrast (less sensitive than CT Angiofor vessels, good for bony/cartilaginous structures) or MRA of neck (less sensitive than CT Angio for vessels,best for soft tissue trauma) or MRI of neck (less sensitive than CT Angio for vesselsand bony/cartilaginous structures, best study for softtissue trauma) or MRI/MRA of brain (most sensitive for anoxic braininjury, stroke symptoms and intercerebralpetechial hemorrhage) Carotid Doppler Ultrasound (NOT RECOMMENDED: leastsensitive study, unable to adequately evaluate vertebralarteries or proximal internal carotid)(-)( )Continued ED/Hospital Observation(based on severity of symptoms andreliable home monitoring) Consult Neurology Neurosurgery/TraumaSurgery for admission Consider ENT consult for laryngeal traumawith dysphonia*References on page 2Brochure Design byYesenia AcevesStrangulationTrainingInstitute.comVersion 17.9 9/16WSS
RECOMMENDATIONS for the MEDICAL/RADIOGRAPHICEVALUATION of ACUTE ADULT, NON-FATAL STRANGULATIONREFERENCES(Recommendations based upon case reports, case studies, and cited medical literature)1.Christe A, Thoeny H, Ross S, et al. Life-threatening versus non-life-threatening manual strangulation:are there appropriate criteria for MR imaging of the neck?. Eur Radiol 2009;19: 1882-18892.Christe A, Oesterhelweg L, Ross S, et al. Can MRI of the Neck Compete with Clinical Findings in AssessingDanger to Life for Survivors of Manual Strangulation? A Statistical Analysis, Legal Med 2010;12:228-2323.Yen K, Thali MJ, Aghayev E, et al. Strangulation Signs: Initial Correlation of MRI, MSCT, and Forensic NeckFindings, J Magn Reson Imaging 2005;22:501-5104.Stapczynski JS, Strangulation Injuries, Emergency Medicine Reports 2010;31(17):193-2035.Yen K, Vock P, Christe A, et al. Clinical Forensic Radiology in Strangulation Victims: Forensic expertise basedon magnetic resonance imaging (MRI) findings, Int J Legal Med 2007;121:115-1236.Malek AM, Higashida RT, Halback VV, et al. Patient Presentation Angiographic Features and Treatment ofStrangulation-Induced Bilateral Dissection of the Cervical Carotid Artery: Report of three cases, J Neurosurg2000;92(3):481-4877.Di Paolo M, Guidi B, Bruschini L, et al. Unexpected delayed death after manual strangulation: need for careexamination in the emergency room, Monaldi Arch Chest Dis 2009;Sep;71(3):132-48.Dayapala A, Samarasekera A and Jayasena A, An Uncommon Delayed Sequela After Pressure on the Neck:An autopsy case report, Am J Forensic Med Pathol 2012;33:80-829.Hori A, Hirose G, Kataoka, et al. Delayed Postanoxic Encephalopathy After Strangulation, Arch Neurol1991;48:871-87410.Iacovou E, Nayar M, Fleming J, Lew-Gor S, A pain in the neck: a rare case of isolated hyoid bone trauma,JSCR 2011;7(3)11.Oh JH, Min HS, Park TU, Sang JL, Kim SE, Isolated Cricoid Fracture Associated with Blunt Neck Trauma;Emerg Med J 2007;24:505-50612.Gill JR, Cavalli DP, Ely SF, Stahl-Herz J, Homicidal Neck Compression of Females: Autopsy and SexualAssault Findings, Acad Forensic Path 2013;3(4):454-45713.Sethi PK, Sethi NK, Torgovnick J, Arsura E, Delayed Left Anterior and Middle Cerebral Artery HemorrhagicInfarctions After Attempted Strangulation, A case report; Am J Forensic Med Pathol 2012;33:105-10614.Clarot F, Vaz E, Papin F, Proust B, Fatal and Non-fatal Bilateral Delayed Carotid Artery Dissection after ManualStrangulation, Forensic Sci Int 2005;149:143-15015.Molack J, Baxa J, Ferda J, Treska V, Bilateral Post-Traumatic Carotid Dissection as a Result of a StrangulationInjury, Ann Vasc Surg 2010;24:1133e9-1133e1116.Plattner T, Bollinger S, Zollinger U, Forensic Assessment of Survived Strangulation, Forensic Sci Int2005;153:202-20717.Miao J, Su C, Wang W, et al. Delayed Parkinsonism with Selective Symmetric Basal Ganglia Lesion afterManual Strangulation, J Clin Neurosci 2009;16:573-575Purvin V, Unilateral Headache and Ptosis in a 30-Year-Old Woman, Surv Ophthalmol 1997;42(2):163-16818.19.Nazzal M, Herial NA, MacNealy MW: Diagnostic Imaging in Carotid Artery Dissection: A case report andreview of current modalities; Ann Vasc Surg 2014;28;739.e5-739.e920.Chokyu TT, Miyamoto T, Yamaga H, Terada T, Itakura T: Traumatic Bilateral Common Carotid Artery DissectionDue to Strangulation: A case report; Interventional Neuroradiology;12:149-154, 2006Brochure Design byYesenia AcevesStrangulationTrainingInstitute.comVersion 17.9 9/16WSS
PHYSIOLOGICAL CONSEQUENCES OF STRANGULATIONOcclusion of Arterial Blood Flow: Seconds to Minutes TimelineCreated by: Ruth Carter; Bill Smock, MD; Gael Strack, JD; Yesenia Aceves, BA; Marisol Martinez, MA; and Ashley Peck1minute0146.81530secondssec.(5-10 sec.range)sec.(11-17 dTime TorenderAnoxicseizure1,2loss ofBlAdderconTrol1loss us 6.8 secondsAdult Male1RefeRencesand62 sec.152 sec.deATh/resPirATionceAsesdeATh/resPirATion ceAsesBeginning Time2(First patient, 1/14dead at 62 seconds)Ending Time2(All patients, 14/14 deadbetween 62 and 152 seconds)ResouRces1 Acute Arrest of Cerebral Circulation in Man, Lieutenant Ralph Rossen (MC), U.S.N.R.; Herman Kabat, M.D., PH.D. Bethesda, MD.and John P. Anderson Red Wing, Minn.; Archives of Neurology and Psychiatry, 1944, Volume 50, #5.2 Anny Sauvagneau, MD, MSc; Romano LaHarpe, MD; David King, MD; Graeme Dowling, MD; Sam Andrews, MD; Sean Kelly, MD;Corinne Ambrosi, MD; Jean-Pierre Guay, PhD; and Vernon J. Geberth, MS; MPS for the Working Group on Human Asphyxia, ForensicMed Pathol 2011;32: 104 – 107.3 Training Institute on Strangulation Prevention: ulationtraininginstitute.comThis project is supported all or in part by Grant No. 2016-TA-AX-K067 awarded by the Office on Violence Against Women, U.S. Department of Justice.The opinions, findings, conclusions, and recommendations expressed in this publication/program/exhibition are those of the author(s) and do notnecessarily reflect the views of the Department of Justice, Office on Violence Against Women.
PEDIATRIC-ADOLESCENT FOLLOW-UP EVALUATIONName of Examining Agency:Address:Date of Initial Exam:Date of Today’s Exam:Time:Case Number(s):Name of Patient:Date of Birth:Address:Accompanied By:Others Present:PATIENT RELEASE STATEMENTI,, hereby request and authorize the staff of;(agency/agencies)to conduct a medical-forensic follow-upevaluation and clinical procedures, including collection and examination of specimens as arenecessary for diagnosis and treatment as well as investigation. Furthermore, I hereby authorize andrequest the medical staff to supply all items of evidence ( initials) and copies of medical andlaboratory reports ( initials) to the appropriate investigative agency for use in the investigationand any resulting legal proceedings.Patient ExaminedDateParent or GuardianWitnessPHOTOGRAPHIC RELEASEI,, hereby request and authorize the staffof;(agency/agencies)to capture and produce photographs ofbody surface or colposcope images of injury, healing injury or normal anatomy. The release of thesephotographs is conditioned upon the images being viewed only by those persons officially involved inthe investigation or legal proceedings. De-identified photos may be used and viewed foreducation/teaching purposes.Patient PhotographedParent or GuardianDateWitness1
Patient’s NameHISTORY1. Review of initial exam documentationYesNo2. Reason for follow-up examinationPhysical AbuseN/AStrangulationOtherSummary of acute strangulation evaluation:Description of injury/abuse event(s) in patient’s own words:Name of examiner:Date:Signature:Patient Label2
PHYSICAL ASSESSMENTVital Signs: TP R B/P Pulse OxNeck Circumference (Anterior) (Lateral)Mental Status/Behavior/Appearance:Review of Muscle/BonePsych/SocialSince the strangulation, has the patient noted any of the following iaHeadacheLightheadednessNeck painNeck swellingNose painNauseaVomitingCrepitusUncontrolled ise altered mental status Describe:Voice changesDescribe:Vision changesDescribe:BleedingDescribe:Weakness/numbness of extremitiesDescribe:Name of examiner:Date:Signature:3
PHYSICAL ASSESSMENT (continued)Pain score:Numbered scale usedWong Baker scale used (insert score)On a scale of 0-10, with 0 being no pressure and 10 being the worst pressure you can imagine, how strongwas the grip during your strangulation (Circle one):0123Is the patient pregnant?45678910Yes ; How many PalateEarsN/AScalpTympanic Membrane(s)Tongue or oral cavity injuryDescribe:Neurological findingsPtosisFacial droopParalysisUnilateral weaknessOther:Absence of normal crepitus when manipulating cricoid cartilageVisible injury (describe on body maps below)Digital photography completeLoss of sensationMethod/Manner of Strangulation:One handEstimated length of time:secondsTwo handsEstimated length of time:seconds“Chokehold”Estimated length of time:secondsApproached from the frontApproached from behindMultiple strangulation attempts during incident How many?Jewelry on patient’s neck during strangulationLigature usedDescribe if possible:Smothering sDuring the strangulation did the patient note any of the following:Loss of consciousness/blacking out/passing outIncontinence of urineIncontinence of stoolBleedingDescribe:Patient’s feet lifted off the groundPatient’s shirt was tightened around their neckNumber of times:During the follow up evaluation were symptoms noted by the examiner?Yes:NoName of examiner:Date:Signature:4
Cranial Nerve AssessmentNerveCN I OlfactoryCN II OpticCN III OculomotorCN IV TrochlearCN V TrigeminalCN VI AbducensCN VII FacialCN VIII Acoustic/VestibularCN IX GlossopharyngealCN X VagusAssessmentIdentifies a familiar scent with eyesclosed (coffee)Read one eye at a time, visual fieldstested by having patient cover one eyeand identifying number of fingers ineach visual fieldCheck pupillary response with light,check accommodation by moving yourfinger towards the patient’s nose, checkfor EOMsHave patient look down and inAsk patient to open mouth while youattempt to close it, have them attemptto move jaw laterally. Have patientclose their eyes, touch their face withcotton and have patient identify wherethey were touched.Have patient move their eyes from sideto sideAsk patient to smile and raiseeyebrows, ask them to keep eyes andlips closed while you try to open themTest hearing with rubbing fingers orwhisperingObserve patient swallow and check gagreflexAssess gag and swallowing with IX,assess patient’s voice characteristicsNotesWNLUnable to assessWNLUnable to assessWNLUnable to assessWNLWNLUnable to assessUnable to assessWNLUnable to assessWNLUnable to assessWNLUnable to assessWNLUnable to assessWNLUnable to assess5
CN XI Spinal AccessoryHave patient shrug shoulders withresistance, have patient move headfrom side to side.Have patient stick out tongue and moveit internally from right to left, assessarticulation.CN XII HypoglossalWNLUnable to assessWNLUnable to assessDescribe abnormalities here:Cranial nerve assessment normalDIAGRAMS (Document any injuries):RIGHT CONJUNCTIVARIGHT INNER EYE LIDRIGHT OUTER EYE LIDLEFT OUTER EYE LIDLEFT INNER EYE LIDLEFT CONJUNCTIVAName of examiner:Date:Signature:6
Name of examiner:Date:Signature:7
SUMMARY ASSESSMENT:PLAN of CARE & RECOMMENDATIONS:Pediatric Strangulation Discharge InstructionsName of examiner:Date:Signature:8
DETAILED BODY SURFACE 18.19.20.If more space is required, please use a progress note and check the box below.Please see progress note for additional findings.Please see age appropriate diagrams (appendices) for additional findings9
APPENDIX AFEMALE INFANT BODY MAP/DIAGRAMNumerically mark each finding (1, 2, 3 ) and provide a detailed description.10
APPENDIX BMALE INFANT BODY MAP/DIAGRAMNumerically mark each finding (1, 2, 3 ) and provide a detailed description.11
APPENDIX CFEMALE CHILD BODY MAP/DIAGRAMNumerically mark each finding (1, 2, 3 ) and provide a detailed description.12
APPENDIX DMALE CHILD BODY MAP/DIAGRAMNumerically mark each finding (1, 2, 3 ) and provide a detailed description.13
APPENDIX EFEMALE ADOLESCENT BODY MAP/DIAGRAMNumerically mark each finding (1, 2, 3 ) and provide a detailed description.14
APPENDIX FMALE ADOLESCENT BODY MAP/DIAGRAMNumerically mark each finding (1, 2, 3 ) and provide a detailed description.15
StrangulationVisible Signs (may not be present)Petechiae(red spots)Blood-RedEyesBruisingChild victims of strangulation may feel terror and extremepain. If strangulation continues, unconsciousness willfollow. Before sliding into unconsciousness, a child victimmay resist violently, producing injuries to their own neck orto the face or hands of their attacker. These defensiveinjuries may not be present in young or developmentallydisabled children, or if the victim is physically orchemically restrained.Observing ChangesSwollen LipCord orRope BurnsScratchesAdditional Signs and SymptomsA larger version of the graphic above which contains detailedsigns and symptoms is available for download rary/pediatric/This project is supported all or in part by Grant No.2016-TA-AX-K067 awarded by the Office on Violence AgainstWomen, U.S. Department of Justice. The opinions, findings,conclusions, and recommendations expressed in thispublication/program/exhibition are those of the author(s) and do notnecessarily reflect the views of the Department of Justice,Office on Violence Against Women.TRAINING INSTITUTEStrangulation is often under-recognized in children but noless serious than in adults. Unconsciousness mayhappen within seconds and death within minutes.Children may be strangled when caregivers lose control,as part of physical and/or sexual assault, or as a way ofdemonstrating ultimate power and control over the child.Regardless, strangulation of a child can have long-lastingphysical and mental health effects and can result in deatheven months later.a program stitute.comIllustration & Graphics by Yesenia AcevesDocumentation by photographs organized in order, for aperiod of days after the attack is very helpful inbeginning and building a journal of proof.Victims should be given medical attention if theyexperience difficulty breathing, speaking, swallowing orexperience nausea, vomiting, lightheadedness,headache or holding head, accidental urination and/orbowel movement in children not diapered. A medicalevaluation may be extremely important in detectinginternal injuries and saving a life.Losing ConciousnessVictims may lose awareness or faint by any one or allof the following methods: blocking of the blood vesselsfrom the heart in the neck (taking away oxygen fromthe brain), blocking of the large veins in the neck(preventing deoxygenated blood from exiting thebrain), and closing off the tube from the mouth to thelungs, making breathing impossible.Alliance for HOPE International101 West Broadway Suite 1770San Diego, CA 92101(888) 511-3522allianceforhope.comSTRANGULATIONWhat Parents and CaregiversNEED TO KNOW
Signs of StrangulationMonitor the Child’s SIGNSDate &TimePhotograph and Journal the Child’s SignsHead- pinpoint red spots (petechiae) on scalp, hair pulled,bump(s), skull fracture(crack), concussion.Face- red or flushed, petechiae, scratch marks.Eyes and Eyelids- petechiae to the left or right eyeball,bloodshot eyes.Ear- petechiae (external and/or ear canal), bleeding fromear canal.Nose- bloody nose, broken nose, petechiae.Mouth- bruising, swollen tongue, swollen lips,Diagrams to MarkVisible InjuriesUse a pen or a marker to indicate any visblesigns and/or symptoms.FrontUnder ChinRight SideLeft SideBackInside Mouthcuts/abrasions(scrapes).Under the chin- redness, scratch marks,bruise(s), abrasions.Neck- redness, scratch marks, fingernail marks, bruise(s),abrasions, swelling, ligature(tie) or clothing marks.Chest and Shoulders- redness, scratch marks,bruise(s), abrasions.Monitor the Child’s SYMPTOMSDate &TimeJournal the Child’s SymptomsSymptoms of StrangulationVoice changes- raspy and/or hoarse voice, coughing,unable to speak, complete loss of voice.Swallowing changes- trouble swallowing, painfulswallowing, neck pain, nausea/vomiting, drooling.Breathing changes- difficulty breathing,hyperventilation, unable to breathe.Behavioral changes- restlessness or aggressiveness,problems concentrating, amnesia(loss of memory),agitation, Post-traumatic Stress Syndrome, hallucinations.Vision changes- complete loss or black & white vision,seeing ‘stars’, blurry, darkness, fuzzy around the eyes.Hearing changes- complete loss of hearing, gurgling,ringing, buzzing, popping, pressure, tunnel-like hearing.Date & TimeJournal Any Other SensationOther changes- Memory loss, unconsciousness,dizziness, headaches, involuntary urination or bowelmovement in potty-trained child, loss of strength,going limp.v 10.3.17
Documentation by photographs sequentially for a periodof days after the assault is very helpful in establishing ajournal of physical evidence.Blood-RedEyesPetechiae(Red Spots)Swollen LipBruisingCord orRope BurnsScratchesBrochure Design & Illustrations by Yesenia AcevesA larger version of the graphic above which containsdetailed signs and symptoms is available for downloadat eranzaThis project is supported all or in part by Grant No.2016-TA-AX-K067 awarded by the Office on Violence AgainstWomen, U.S. Department of Justice. The opinions, findings,conclusions, and recommendations expressed in thispublication/program/exhibition are those of the author(s) and do notnecessarily reflect the views of the Department of Justice,Office on Violence Against Women.TRAINING INSTITUTEona program itute.comVictims should also seek medical attention if theyexperience difficulty breathing, speaking, swallowing orexperience nausea, vomiting, lightheadedness,headache, involuntary urination and/or defecation,especially pregnant victims. A medical evaluation maybe crucial in detecting internal injuries and saving a life.Victims may lose consciousness by any one or all ofthe following methods: blocking of the carotid arteriesin the neck (depriving the brain of oxygen), blocking ofthe jugular veins (preventing deoxygenated blood fromexiting the brain), and closing off the airway, makingbreathing impossible.Strangulation has only recently been identified as one of themost lethal forms of domestic violence: unconsciousnessmay occur within seconds and death within minutes.When domestic violence perpetrators choke (strangle) theirvictims, not only is this a felonious assault, but it may be anattempted homicide. Strangulation is an ultimate form ofpower and control, where the batterer can demonstratecontrol over the victim’s next breath; having devastatingpsychological effects or a potentially fatal outcome.Sober and conscious victims of strangulation will first feelterror and severe pain. lf strangulation persists,unconsciousness will follow. Before lapsing intounconsciousness, a strangulation victim will usually resistviolently, often producing injuries of their own neck in aneffort to claw off the assailant, and frequently also producinginjury on the face or hands to their assailant. Thesedefensive injuries may not be present if the victim isphysically or chemically restrained before the assault.Alliance for HOPE International101 W. Broadway, Ste 1770San Diego CA 92101888.511.3522AllianceforHOPE.com
Date &TimeJournal Your SignsHead- pinpoint red spots (petechiae ) on scalp, hair pulled,bump(s), skull fracture, concussion.Face- red or flushed, petechiae, scratch marks.Eyes and Eyelids- petechiae to the left or right eyeball,bloodshot eyes.Ear- petechiae (external and/or ear canal), bleeding fromear canal.Nose- bloody nose, broken nose, petechiae.Mouth- bruising, swollen tongue, swollen lips,cuts/abrasions.Under the chin- redness, scratch marks,bruise(s), abrasions.Neck- redness, scratch marks, fingernail impressions,bruise(s), abrasions, swelling, ligature marks.Chest and Shoulders- redness, scratch marks,bruise(s), abrasions.Date &TimeJournal Your SymptomsVoice changes- raspy and/or hoarse voice, coughing,unable to speak, complete loss of voice.Swallowing changes- trouble swallowing, painfulswallowing, neck pain, nausea/vomiting, drooling.Breathing changes- difficulty breathing,hyperventilation, unable to breathe.Behavioral changes- restlessness or combativeness,problems concentrating, amnesia, agitation,Post-traumatic Stress Syndrome, hallucinations.Vision changes- complete loss or black & white vision,seeing ‘stars’, blurry, darkness, fuzzy around the eyes.Hearing changes- complete loss of hearing, gurgling,ringing, buzzing, popping, pressure, tunnel-like hearing.Other changes- Memory loss, unconsciousness,dizziness, headaches, involuntary urination or defecation,loss of strength, going limp.Date & TimeJournal Any Other SensationUse a pen or a marker to indicate any visblesigns and/or symptoms.
PEDIATRIC STRANGULATION DISCHARGE INSTRUCTIONSBecause your child has reported being “choked” or strangled, we are providing you with the following instructions:Consider a small ice pack to the neck area for relief of pain.Offer popsicles or offer fluids that are cooling to the throat. Kids like this.Make sure someone is with your child for the next 24-48 hours.Please report to the nearest ER or call 911 immediately if you noticethe following symptoms or changes in your child: Difficulty breathing or shortness of breathLoss of consciousness or “passing out”Changes in your child’s voice or difficulty speakingDifficulty swallowing, lump in throat, ormuscle spasms in throat or neck Tongue swelling and/or drooling Swelling to throat or neck, new, worsening orpersisting throat pain (“My throat still hurts”) Prolonged nose bleed (greater than ten minutes) Continues to cough or coughing up blood Continues to vomit or vomiting up blood Left or right-sided weakness, numbness, or tingling(child cannot use arm or leg) New or Worsening headache Seizures (Abnormal, rhythmic or shaking movements) Behavioral changes or memory loss Thoughts of harming self or others ie: (“I do not wantto live”) (“I am going to hurt him”)It is important that the above symptoms be evaluated by a physician.After your child’s evaluation, keep a list of any changes in symptoms for your child’s physician andlaw enforcement.If symptoms worsen, report to your child’s physician or nearest ER. You should follow-up with lawenforcement regarding documentation of any and all information about your child’s symptoms.It is important that you have a follow-up medical screening in 1-2 weeks at the clinic or with yourchild’s physician. Make sure to bring these discharge instructions with you.IF you misplace these instructions call or your provider for a copy.I have been made aware of and understand the importance of following the above outlined instructions.Patient/Parent SignatureProvider Signature1 copy patient fileFlyer design by Yesenia AcevesDate1 copy patientStrangulationTrainingInstitute.comVersion 8.21.17
Strangulation, Forensic Sci Int 2005;149:143-150 15. Molack J, Baxa J, Ferda J, Treska V, Bilateral Post-Traumatic Carotid Dissection as a Result of a Strangulation Injury, Ann Vasc Surg 2010;24:1133e9-1133e11 16. Plattner T, Bollinger S, Zollinger U, Forensic Assessment of Survived Strangulation, Forensic Sci Int 2005;153:202-207 17.