Transcription
Journal of 0ORIGINAL COMMUNICATIONA comparison of telemedicine and in‑person neurology visits: whatare the factors that patients consider when selecting future visit type?Carly Olszewski1 · Sharon Thomson1 · Kelly Pring1 · Siobhan Cox1 · Rebecca Merrill1 · Emily Fishman1 ·Alexander Ambrosini1 · Kevin Alexander Soltany1 · Gabby Bognet2 · Lauren Strauss3 · Rachel Graham3 · Amy Guzik3 ·Roy E. Strowd3Received: 20 December 2021 / Revised: 17 April 2022 / Accepted: 18 April 2022 The Author(s), under exclusive licence to Springer-Verlag GmbH Germany 2022AbstractObjective To identify factors that patients consider when choosing between future in-person, video, or telephone visits.Background Telemedicine has been rapidly integrated into ambulatory neurology in response to the COVID-19 pandemic.Methods Ambulatory neurology patients at a single center were contacted via telephone to complete: (1) a survey quantifying likelihood of scheduling a future telemedicine visit, and (2) a semi-structured qualitative interview following their visitin March 2021. Data were processed using the principles of thematic analysis.Results Of 2493 visits, 39% assented to post-visit feedback; 74% were in-person visits and 13% video and telephone.Patients with in-person visits were less likely than those with video and telephone visits to “definitely” consider a futuretelemedicine visit (36 vs. 59 and 62%, respectively; p 0.001). Patients considered five key factors when scheduling futurevisits: “Pros of Visit Type,” “Barriers to Telemedicine,” “Situational Context,” “Inherent Beliefs,” and “Extrinsic Variables.”Patients with telemedicine visits considered convenience as a pro, while those with in-person visits cited improved qualityof care. Accessibility and user familiarity were considered barriers to telemedicine by patients with in-person and telephonevisits, whereas system limitations were prevalent among patients with video visits. Patients agreed that stable conditionscan be monitored via telemedicine, whereas physical examination warrants an in-person visit. Telemedicine was inherentlyconsidered equivalent to in-person care by patients with telephone visits. Awareness of telemedicine must be improved forpatients with in-person visits.Conclusion Across visit types, patients agree that telemedicine is convenient and effective in many circumstances. Futurecare delivery models should incorporate the patient perspective to implement hybrid models where telemedicine is an adjunctto in-person visits in ambulatory neurology.Keywords Clinical neurology · Practice management · COVID-19 · Telehealth · TelemedicineIntroductionAlthough telestroke has existed since the mid-2000s, telemedicine in ambulatory neurology evolved rapidly inMarch 2020 [1–3]. In our facility, telemedicine was theonly option for ambulatory care during the first 8 weeks* Roy E. Strowdrstrowd@wakehealth.edu1Wake Forest School of Medicine, Winston‑Salem, NC, USA2Wake Forest University, Winston‑Salem, NC, USA3Department of Neurology, Wake Forest Baptist Health, 1Medical Center Boulevard, Winston‑Salem, NC 27104, USAof the COVID-19 pandemic. As mask mandates and socialdistancing guidelines were instituted, in-person visits werereintroduced. For the first time, amidst a persistent globalhealth crisis, patients were given the option of scheduling inperson, video, or telephone visits. By March 2021, a hybridmodel of care incorporating both in-person and telemedicinevisits became common at many institutions in the US [4].Previous studies have discussed numerous patientreported benefits of telemedicine. Telemedicine eliminatescommute time and cost, which is especially beneficial forpatients traveling long distances to access subspecialtycare [5–7]. Telemedicine also benefits patients with limitedaccess to transportation, mobility concerns, and caregiverdependence [8]. However, barriers to telemedicine exist. At13Vol.:(01234 electing future visit type:(1) “Pros of Visit Type,” (2) “Barriers to Telemedicine,”(3) “Situational Context,” (4) “Inherent Beliefs,” and (5)“Extrinsic Factors.” Each meta-theme subsequently comprised three to four sub-themes.Factors that patients with in‑person visits considerwhen selecting future visitsWhen selecting a future visit type, patients who completedin-person visits predominantly described “Pros of VisitType” (Table 2). Patients were most likely to acknowledgeelimination of commute time and associated cost as a pro oftelemedicine (8% of total in-person responses), followed byseveral pros of in-person visits: improved communication(7%), improved quality of care (5%), and greater personability of the provider (5%). Patients deliberated these pros ofvisit types, stating, “We have a long drive, so we would doit [virtually],” and “I just like it in-person because you geta better sense of what’s going on and communicate better.”Patients completing in-person visits also frequently commented on “Barriers to Telemedicine.” The most prevalentbarriers were user limitations such as the challenge of keeping children engaged (2%) and unfamiliarity with telemedicine (2%). Unfamiliarity was expressed by statements suchas, “I’m old school—I like to see the doctor in-person.”13
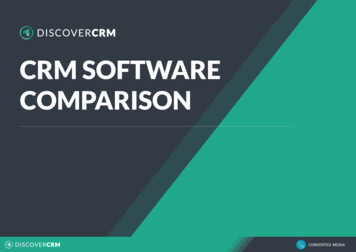
Journal of NeurologyFig. 1 Patient responses toQuestion 2 of the quantitativetelephone survey stratified bypatient-reported visit type (inperson: n 939; video: n 120;telephone: n 120). A significant difference (p 0.01*) wasfound between the (1) patientswho had in-person and videovisits and (2) patients who hadin-person and telephone visitswho would “definitely” considera future telemedicine visitLikelihood Of Patient To Consider A Future Telemedicine Visit FollowingAn In-person, Video, or Telephone telyForty-five percent of responses described “SituationalContext,” or situations that are best suited for differentvisit types. In-person visits were preferred when a physical examination is required (10%), for worsening symptoms(5%), for an initial visit with an unknown diagnosis (4%),or for instances when a patient perceived their diagnosis tobe more severe (e.g., Parkinson’s, ALS, or pediatric epilepsy; 4%). Telemedicine was preferred when patients didnot require an in-person service (such as adjustments to deepbrain stimulator settings; 6%) or for follow-up visits of stableconditions (5%).Nine percent of in-person responses described “Inherent Beliefs.” At times, patients noted a lack of preferencebetween telemedicine and in-person visits (2%), stating thattelemedicine’s utility depends on their specific needs without providing further detail (3%). Other patients shared theirbelief that in-person visits are superior to telemedicine visits, in which case, they would only consider telemedicine asa last resort (2%). For instance, “If an in-person visit was notan option, then I would have done a telehealth appointment.”Seven percent of responses cited “Extrinsic Variables”such as lack of awareness about telemedicine visits (5%).Factors that patients with telemedicine visits considerwhen selecting future visitsFor patients who completed a telemedicine visit, the mostcommonly reported “Pros of Visit Type” was convenienceof telemedicine, yet greater personability of the physicianat in-person visits was also frequently acknowledged (6% ofvideo and 7% of telephone) (Table 3). Convenience includedthe elimination of commute time and cost (12% for both visittypes) and the ease for patients with limited mobility (3% forboth). One patient’s spouse remarked, “Telephone was finebecause it takes a lot of work with the wheelchair to get into13MightOnly If RequiredTelephoneNeverthe office now.” Others commented, “I just felt it [the videovisit] was not as personable. There’s something about beingface-to-face. Even though we can still see each other, it is notthe same.”“Situational Context” was highly considered by patientswith telemedicine visits (40% of video responses and39% of telephone). Patients commented on telemedicine’s utility for: follow-up of stable conditions (5% forboth), annual visits (2% and 3%), or instances wherein-person services were not needed (6 and 3%, respectively). In-person visits were preferred for worseningsymptoms (7% and 16%) or physical examination (10%and 11%). Patients often emphasized physical examination as a driving factor for in-person visits: “If there wassomething that I felt needed to be physically examined,then we would come in.”Within “Inherent Beliefs” (12% of video responses and14% of telephone) some patients commented that telemedicineoffers an equivalent quality of care to in-person visits (3% and4%), with no general preference for visit type (4% for both).One patient remarked, “It did not matter one way or the other.She was just as effective on video.” Patients also commentedthat the use of telemedicine may “depend on what the appointment was for” (2% and 3%).Both visit types were influenced by “Extrinsic Variables”such as alternate decision-makers (1% for both). One patientsaid, “I did not choose [the video visit]. That’s just what they[clinic staff] told me.”
Quality of Medical Care (40%)Humanistic Qualities (15%)Safety (6%)Representative patient quotes“We live almost 4 h away, so we would like to have atelehealth appointment in the future.”“Virtual is much better [than in-person]. We do nothave to go all the way there. Especially with myfather—he has a movement disorder. So with hiswheelchair, it [telemedicine] is just more convenient.”Convenience for full-time employees, students, or“Yes, I’d prefer telehealth because it is hard formothers (5%)him [the patient] to get off work.”Convenience due to elimination of need for access to “I would prefer telehealth because I do not havea car or other modes of transportation (14%)transportation.”Convenience due to reduced or absent wait time at“We always have to wait around 45 min to see the docthe physician office (0%)tor when we go in-person.”Telemedicine is a safer option due to Coronavirus or “For this one [visit], I could have done telehealth,other concerns (100%)and it probably would have been better. Just withCOVID, it’s not completely over, so I’m not 100%comfortable going to the doctor’s office more than Ihave to.”“With MS, I stay in the bubble, trying to avoid asmuch contact as possible.”Telemedicine is family-centered by permitting multi- –ple family members to be present at a visit (0%)In-person visits are more personable (100%)“I would prefer to come in to see the doctor, because Ijust like to see the doctor face-to-face.”In-person visits provide improved communication“I do not care for telehealth because sometimes you do(55%)not get your point across. It’s harder to communicateand feel on the same page.”“Sometimes, the doctors do not say exactly whatthey’re thinking, but if I’m there and I see somethingdifferent, I will ask a question. On the telephone, Ido not feel as comfortable asking questions.”In-person visits provide improved quality of care“How can they tell anything over a video?”(41%)“I think there are things that can get missed when youdo a telehealth visit.”In-person visits are more thorough due to a longer“I feel like I am heard more when it is in-person. Theduration of visit (4%)phone appointments seem too quick.”Elimination of commute time, associated gas andparking costs (71%)Convenience for patients with limited mobility (9%)Pros of Visit Type (31%)Convenience (39%)Patient experience (% of sub-theme)Meta-theme (% of total codes) Sub-theme (% of meta-theme)Table 2 Summary of emergent qualitative themes describing factors that in-person patients consider when scheduling future ambulatory neurology visits (n 699)Journal of Neu medicine is a safer option due toCoronavirus or other concernsTelemedicine is family-centered bypermitting multiple family members tobe present at a visitIn-person visits are more personableIn-person visits provide improved communicationIn-person visits provide improved quality of careIn-person visits are more thorough dueto a longer duration of visitNeed for assistance with technologyLack of access to a telemedicine deviceInsurance does not cover telemedicinevisitsSelf-reported symptom limitationsTechnology system difficulty such asWiFi/internet connection, audio/videoquality issuesDifficult for childrenLack of familiarityCommunication difficulties due to hearing impairmentUser technology difficultyTelephone visits Patient experience (% of its (%)52Video visits(%)Table 3 Summary of qualitative themes describing the factors that telemedicine patients consider when selecting future visit type (n 120 for patients with video and telephone visits)Journal of Neurology13
Video visits(%)4012Meta-theme (% of totalcodes)Situational ContextInherent BeliefsTable 3 (continued)13143945In-person ServiceRequirement2829Severe or UndiagnosedConditionEquivalence of Telemedicine and In-person26Video visits(%)Stable ConditionTelephone visits Sub-theme (% of meta(%)theme)In-person visits are preferred whensymptoms are worseningIn-person visits are preferred for severeor undiagnosed conditionsIn-person visits are preferred for postoperative visitsTelemedicine is best for emergent situationsIn-person visits are preferred for initialvisits with a new providerTelemedicine is best when no in-personservices such as labs or imaging arerequiredIn-person visits are preferred when inperson services are requiredIn-person visits a
patients traveling long distances to access subspecialty care [5-7]. Telemedicine also benets patients with limited access to transportation, mobility concerns, and caregiver dependence [8 ]. However, barriers to telemedicine exist. At * Roy E. Strowd rstrowd@wakehealth.edu 1 Wake Forest School of Medicine, Winston-Salem, NC, USA