Transcription
JUNE 2022ANALYSIS OFCOMMUNITYTREATMENTOBSERVATORYDATA FOR HIV ANDHEPATITIS C VIRUSSERVICES ININDIA ANDINDONESIA
We sincerely acknowledge and appreciatethe time and effort of care recipients, serviceproviders, HIV and hepatitis C treatmentcenters, and community networks in the datacollection and advocacy processes sharedin this report. Without their assistance, thiswork would not have been possible.Photography courtesy ofCommunity Network for Empowerment (CoNE) and Yayasan Peduli Hati Bangsa
TABLE OF CONTENTSACRONYMS3BACKGROUND4CTO Program4DATA ANALYSIS METHODOLOGY6SUMMARY OF MAIN FINDINGS7DETAILED FINDINGS9INDIA9Manipur, India HIV Quantitative Results9Manipur, India HIV Qualitative Results10Manipur, India HCV Quantitative Results14Manipur, India HCV Qualitative Results15INDONESIA18HIV Quantitative and Qualitative Results18HCV Quantitative and Qualitative Results21DATA FROM STOCK-OUT MONITORING25NEXT STEPS27
WTCTGTLDTNDVLVLT3Antiretroviral Treatment CenterComplete Blood CountCommunity Health CenterCommunity-Led MonitoringCommunity Treatment ObservatoryFaith-Based OrganizationHepatitis C VirusIntegrated Counseling and Testing Center[India] Jawaharlal Nehru Institute of Medical SciencesKidney Function Test[India] Link ART CenterLiver Function Test[India] Manipur State AIDS Control SocietyMen who have Sex with Men[India] Model Treatment Center[India] National AIDS Control OrganizationNon-Governmental OrganizationNational Health InsuranceNational Viral Hepatitis Control ProgramOutpatient DepartmentPrimary Health CenterPeople Who Inject Drugs[India] Regional Institute of Medical Sciences[India] State AIDS Clinical Expert Panel[India] State Nodal OfficerSustained Virologic ResponseSex WorkerTreatment CenterTransgenderTenofovir, Lamivudine and DolutegravirTarget Not DetectedViral LoadViral Load Testing
BACKGROUNDamfAR’s TREAT Asia program worked with partners to initiate twoCommunity Treatment Observatories (CTOs) in two sites in India andIndonesia. The two national partners are the Community Networkfor Empowerment (CoNE) in India and Peduli Hati in Indonesia. Theproject has been implemented with the International TreatmentPreparedness Coalition (ITPC) as a technical partner, which assistedin training the national partners in India and Indonesia and TREAT Asiastaff, and currently hosts the CTO databases of the two sites on itsonline portal.In collaboration with TREAT Asia, ITPC organized and led trainingson the CTO model, including indicator development, CTO/Community-Led Monitoring (CLM) principles and the CLM cyclefrom data collection to advocacy. Country-specific quantitative andqualitative indicators on HIV and hepatitis C virus (HCV) serviceswere developed for the CTOs of CoNE and Peduli Hati.Each organization carried out data collection from February/Marchto December 2021 for their selected health facility sites and enteredthe data into the databases hosted by ITPC. This report presentsthe findings and analyses of the data to help guide the ongoingimplementation of the CTOs and to inform advocacy for HIV and HCVservice improvements for people living with HIV (PLHIV) and peoplewho inject drugs (PWID).Project implementation and data collection were conducted duringthe COVID-19 pandemic. The consequent restrictions on clinicalcare and transportation proved difficult both for service providersand recipients, and impacted the quality and continuity of services.The CTO staff and service providers put in extra efforts to ensurecontinuity of CTO data collection and service provision. The programpartners are grateful for the time and effort provided to the CTOsby all health care providers, data collection sites, key populationrepresentatives and government departments.CTO ProgramCommunity Treatment Observatories in Manipur state in India andin Indonesia were aimed at documenting the availability, continuity,and quality of local HIV and HCV services. CLM data collection wasguided by a set of country- and disease-specific quantitative andqualitative indicators. For India, a total of six sites were selected forquantitative and qualitative data collection for both HIV and HCV(see Table 1). For Indonesia, quantitative data for HIV and HCV werecollected from two Ministry of Health (MOH) websites, and frominterviews and focus group discussions (FGDs) for qualitative data(see Table 1). The primary target populations for qualitative datacollection for both countries were health service providers, PLHIVand PWID. In Indonesia, services for children living with HIV werealso explored (see Table 2).The implementation of the proposed CTOs followed the ITPC model,which includes four components: 1) Education enabling communitiesto identify barriers to accessing and shortfalls in the quality of HIV andHCV services; 2) Evidence of the identified issues provided throughthe collection and validation of relevant community-level data;3) Engagement with partners representing a variety of stakeholders;and 4) Advocacy to encourage all engaged partners to work togetherto address the identified gaps in HIV services.Each CTO was supported by a data supervisor and two datacollectors who each had direct experience working with localcommunities, including key populations (i.e., PLHIV and PWID) whoare at highest risk for HIV and HCV. The data collected focused onthe state of HIV and HCV programs, treatment procurement systems,drug stocks, and diagnostics facilities that test for viral load and forcommon co- and opportunistic infections.4
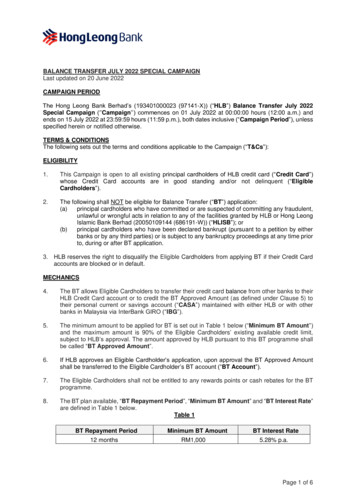
Table 1. Selected monitoring sites and data sources for data collection for HIV and HCVMANIPUR STATE, INDIAMONITORING SITES FOR QUANTITATIVE & QUALITATIVE DATAFACILITY LOCATIONJawaharlal Nehru Institute of Medical Sciences and HospitalHIV – ART Center, HCV – Model Treatment CenterImphal East DistrictRegional Institute of Medical Sciences and HospitalHIV – ART CenterImphal West DistrictChandel District HospitalHIV – ART Center, HCV – Treatment CenterChandel DistrictUkhrul District HospitalHIV – ART CenterUkhrul DistrictCommunity Health CenterLink ART CenterSaikul, Kangpokpi DistrictNGO implementing the Targeted Intervention projectState-wideINDONESIAMONITORING SITES / DATA SOURCESTYPE OF DATAMinistry of Health Hepatitis Information System, official websiteQuantitative HCVMinistry of Health HIV Sub-Directorate websiteQuantitative HIVMinistry of Health Hepatitis Sub-Directorate staffQualitative HCVLentera Anak Pelangi - NGO representing children living w/HIV in Jakarta who were accessingART and HIV viral load testing from the following hospitals:- Koja Hospital- Sulianti Saroso Infectious Diseases Hospital- Tarakan Hospital- Cipto Mangunkusumo Hospital- Puskesmas (Community Health Center)- Cengkareng Hospital- Dharmais HospitalQualitative HIVFocus group discussion participants accessing HIV and HCV services from the following health facilitiesCity/ProvinceFacilityServices discussedWest KalimantanDr. Soedarso HospitalHIV and HCV antibody tests, HIV and HCV viralload tests, ART, direct-acting antivirals (DAAs)Bogor, West JavaBogor Regional HospitalHIV and HCV antibody tests, HIV and HCV viralload tests, ART, DAAsJakartaPengayoman HospitalHIV and HCV antibody tests, HIV and HCV viralload tests, ART, DAAsFatmawati HospitalHIV and HCV antibody tests, HIV and HCV viralload tests, ART, DAAsBekasi, West JavaBekasi Regional HospitalHIV antibody tests, HIV viral load tests, ARTNorth SulawesiKandou HospitalHIV and HCV antibody tests, HIV and HCV viralload tests, ART, DAAsBhayangkara HospitalBuprenorphine5 Puskesmas (Community Health Center):Tikala Baru, Bahu, Teling Atas, Sario, andTumintingHCV antibody tests(note: HIV services can be accessed in allPuskesmas)Bhayangkara HospitalHCV antibody tests, DAAsAdam Malik HospitalHIV and HCV antibody tests, HIV and HCV viralload tests, ART, DAAsPringadi HospitalHCV antibody tests, DAAsWest Nusa TenggaraWest Nusa Tenggara Provincial HospitalHIV and HCV antibody tests, HIV and HCV viralload tests, ART, DAAsAcehDr. Zainoel Abidin HospitalHIV and HCV antibody tests, HIV and HCV viralload tests, ART, DAAsNorth Sumatra5
Table 2. List of interviews and focus group discussions (FGDs) by country, viral infection and type of intervieweeType of intervieweeIndia HIVIndia HCVIndonesia HIVIndonesia HCVHealth Service Provider3 interviews2 interviews1 interview (servicesfor children)1 interview (MOH HepatitisSub-Directorate staff)1 FGDPLHIV12 interviews1 interview4 FGDsPWID4 interviews2 FGDs14 interviews5 FGDsDATA ANALYSISMETHODOLOGYAnalysis of data as presented in this report was carried outby an external consultant under the guidance of TREAT Asia.The consultant conducted a desk review of country indicatorframeworks and data collection tools. The consultant alsoreviewed and analyzed country indicator data for the periodof 1 March 2021 through 31 December 2021 for India and1 February 2021 through 31 December 2021 for Indonesia,which country CTO implementers had uploaded to a virtualproject database.Data on the virtual database were in the form of Excel-basedindicator tracking sheets for the quantitative data for bothcountries. For qualitative data, each country uploaded amaster Excel-based tracking sheet with details on dateand time, facility code, type of qualitative data collectionmethod (interview or FGD), infection (HIV or HCV) and typeof interviewee (health service provider [HSP], PLHIV, PWID)and reporting period. Qualitative data included scannedcopies of completed paper questionnaires, typed transcriptsand audio recordings of interviews and FGDs. Findings underthe sections on qualitative data for HIV and HCV capturemain (frequent) responses that were raised by each type ofinterviewee and by participants in FGDs. Responses werenot extensively edited in order to retain the voice of therespondent. Where relevant, these responses were furtherorganized by the Availability-Accessibility-AcceptabilityQuality (AAAQ) framework areas.6
SUMMARY OF MAIN FINDINGSTables 3 and 4 below summarize the main findings from reportedcountry data for HIV and HCV. Findings are organized by the AAAQframework1 for assessing health services. It should be noted that theindicators and associated data collection tools were not the sameacross the two countries; rather, they were CTO-specific. Therefore,there are variations in the data presented.Table 3. Main findings from India CTO dataAAAQ categoryHIVHCVAvailabilityInsufficient number doctors or staff to provide services,including for regular health check-upsNot all services are available due to broken downmachines, staff shortageNot all services are available due to broken downmachinesAccessibilityFinancial barriers due to services not consistentlyavailable for free at the government facilities and sopeople have pay for the services out of pocket at privatefacilities; additional out of pocket costs to travel a longway to reach facilitiesFinancial barriers due to services not consistentlyavailable for free at the government facilities and sopeople have pay for the services out of pocket at privatefacilities; additional out of pocket costs to travel a longway to reach facilitiesPhysical barriers due to ART centers not being a closedistance for some people to access convenientlyPhysical barriers due to services not being a closedistance for some people to access convenientlyAdministrative barriers such as the requirement to obtainan outpatient department (OPD) ticket in order to accessservices resulting in long queues and waiting times;working hours not long enough to accommodate allthe patients; some lack a government ID card which isrequired for ART initiationAdministrative barriers such as the requirement to obtainan OPD ticket in order to access services resulting inlong queues and waiting times; working hours not longenough to accommodate all the patients; some lack agovernment ID card which is required to access servicesat the government facilitiesAcceptabilityHealth facility staff not always community-friendly –instances of PLHIV being teased, humiliated and scoldedfor missing appointmentsHealth facility staff not always community-friendly –instances of PWID not feeling comfortable with treatmentby staff because of possible stigma and discriminationfor being a person who uses/used drugs, missingappointments (drug use habits as a main reason for this)QualityWeak referral system between Integrated Counsellingand Testing Center (ICTC) and ART centerIt takes one week to over a month to receive a HCVconfirmatory viral load test resultPoor quality of counselling in some health facilitiesHealth facility infrastructure is inadequate due to lackof drinking water, proper waiting rooms, seatingarrangement and toilet facilitiesStaff not always on time or punctual which createsovercrowding and unnecessary waiting17World Health Organization Availability, accessibility, acceptability and quality infographic can be accessed edge/aaaq-infographic/en/.
For India for HCV, in addition to the AAAQ issues listed in Table3, the following issues facing PWID also created barriers to theiraccessing HCV services:o Low HCV literacy among PWID related to different steps fromscreening to treatment to sustained virologic response (SVR;marker of cure and treatment success)o Drug use habits can lead to relapses for those on treatment andprevent PWID from testing and initiating treatmento Misinformation among PWID regarding taking HCV treatmentand using drugs at the same time, including around whether itis required to stay at a drug rehabilitation center while on HCVtreatmentFor Indonesia, out of 12 HIV quantitative indicators monitored bythe CTO, data for only seven indicators were available. Quantitativedata of the indicators related to access to HIV viral load testing,monitoring and dolutegravir use (DTG) were unavailable.Table 4. Main findings from Indonesia CTO dataAAAQ categoryHIVAvailabilityNot all Community Health Centers have HIV testing linked The 2020-2024 Hepatitis National Plan has beento HIV treatment servicesdisseminated to all 34 provinces, but only implemented(i.e. services available) in 18 priority provinces – thegovernment plans to add four more provinces for a totalof 22 in 2022HCVHCV antibody screening is available in community healthcenters and hospitals, but confirmatory viral load testingis only available at facilities in the 18 provincesServices are sometimes not available due to HCV testingmachines being used for COVID-19-related testingAccessibilityNo major issues were raised related to HIV testing, asrespondents shared that the testing procedure is simpleHIV testing is offered for free at the community healthcenterAccess to multi-month supply of antiretrovirals (ARVs)varies across provincesBarriers related to accessibility include: 1) limitedoperating days; 2) not all HCV services are covered bythe National Health Insurance program, resulting in theneed to pay for some services out of pocket which createsa financial barrier; for those without insurance, the out ofpocket costs are higher and differ based on location andtype of service neededViral load testing is not available to all due to differingguidelines where if you have National Health Insurancesome locations cover it and others do notViral load testing for children is not covered by theNational Health Insurance program and the price variesby locationAcceptabilityNone notedNone notedQualityHIV test results are received within a dayStock-outs in recent years created treatmentinterruptions, but also created reluctance by those ontreatment because a viral load test is required for retreatment and some did not want to pay the cost if notcovered by National Health Insurance or they did nothave insuranceRegarding HIV treatment, the combination of tenofovirlamivudine-DTG (TLD) is offered to those who are newlyinitiating ART or suffering side effects from a differentregimenQuality of services is compromised due to the additionalresponsibilities placed on health facility staff to carry outCovid vaccination and Covid testingFor children living with HIV, national guidelines have notbeen updated since 2014; information on pediatric drugformulations and dosages are only available via webinarsand not from a national guidelinePediatric formulations are unavailable, resulting inhaving to use crushed tablets and smaller doses of adultformulations; application in the field varies by doctor8
DETAILED FINDINGSINDIAThe following data are presented by country and by infection/virus.For India, the data cover the period of March through December2021 for Manipur state. For HIV, issues monitored included accessto HIV treatment, baseline tests (complete blood count, kidney andliver function tests) and viral load testing. For HCV, issues monitoredfocused on access to HCV antibody testing, treatment and HCVconfirmatory RNA viral load testing. For Indonesia, the data are fromFebruary through December 2021. For HIV, issues monitored wereaccess to HIV testing, treatment and routine viral load testing. ForHCV, issues monitored included status of national viral hepatitis plan,access to HCV antibody testing, HCV confirmatory RNA viral loadtesting, treatment and HCV drug stock-outs.HIV QUANTITATIVE RESULTSQuantitative data are presented per indicator. Qualitative data aresummarized per type of interviewee (HSP, PLHIV, PWID, NGO) andper FGD. Where possible, issues raised are further categorized by theAAAQ framework for assessing health services. The percentage of PLHIV on ART out of the total PLHIV enrolled inARTC was 64% (13,366 / 20,732).Summary points: The quantitative data for HIV for the period March-December2021 are reported as total figures. The Manipur State AIDSControl Society (MSACS) could not provide monthly or quarterlydata by indicator to be able to assess for changes. The MSACSinformed CoNE that data are updated annually. The percentage of ART initiation of all the people who testedHIV-positive was 77% (equivalent to the number of PLHIV ontreatment of 20,732 divided by the total number of PLHIV of26,795). The percentage of PLHIV switched to an appropriate regimen(i.e., TLD) out of the total PLHIV on treatment was 29% (3,971 /13,366). The percentage of PLHIV who had an HIV viral load test twice ayear among PLHIV on ART was 30% (4,071 / 13,366). Data were not available for specific key populations. No stock-outs of medicines and diagnostics were reported.Figure 1. India CTO – quantitative data for HIV indicators for the period of March 2021 thru December 20219
Table 5. Quantitative data on access to HIV servicesAccess to HIV treatmentIndicatorsTarget Population*TOTALTotal MaleTotal FemaleTransgender1. Number of PLHIV in the state26,79514,99411,6621392. Number of PLHIV who are ontreatment20,73211,4629,1461243. Number of PLHIV known tobe continuing treatment 12months after initiation13,3666,4956,786854. Number of people testedpositive at IntegratedCounselling and TestingCenters1,756999634NA5. Number of people referredto ART center for treatmentinitiation or pre-ARTregistration1,809NANANA6. Number of people on TLD3,971NANANACOMMENTS FROM DATA COLLECTIONThere is lack of coordination between thecounselling and testing centers and the ARTcenters with regards to referral of peopletesting HIV-positive and needing treatment.As a result, accurate data of the peopletested HIV-positive at the testing centersand referred for treatment initiation are notavailable.Access to baseline tests7. Number of health sites providing baselineinvestigation needed for treatment initiationTotal sites in the stateCOMMENTS FROM DATA COLLECTIONNot availableAll three baseline tests (complete blood count, kidney and liverfunction tests) are available at the government health sites wherean ART center is attached except in some health sites (e.g.,community and primary health centers). However, PLHIV cannotalways access them due to limitations in working hours, lengthyvisit process, overcrowding and transportation requirements.The three tests are available at private labs at a total cost of 30. The tests are more easily accessible at the private lab, butpatients have to pay out of pocket; no provision is available forreimbursement from the government.Access to viral load testingIndicatorsTarget Population*TOTALCOMMENTS FROM DATA COLLECTION8. Number of PLHIV on ART who received aviral load test twice a year4,071The data were collected by manually sitting with MSACS officials.They do not maintain updated data in their computerisedmanagement and information system.9. Number of PLHIV on ART who did notreceive viral load test1,94910.Number of PLHIV who had viral load testingper NACO guidelines11,417This number includes the total number in Indicator no. 8.*Data not available for individual key populations or disaggregated by sex.10
HIV QUALITATIVE RESULTSTable 6: Summary responses from interviews with HSP, PLHIV and PWID on barriers to accessing HIV servicesType ofIntervieweeBarriers to accessing HIV treatmentBarriers to accessingbaseline tests (completeblood count, kidney andliver function tests)Barriers to accessing viral loadtestingHealth serviceproviderLow numbers in pre-ART registration and ARTregistration compared to the total number of PLHIV inthe state due to:1) many people are going to the private lab for HIVtesting (Availability)2) fear of social stigma and self-stigmatization ofPLHIV (Acceptability)3) lengthy process to enrol (administrativeAccessibility)4) privacy issues because Aadhar card (govt ID card)required for ART initiation or people without Aadharcard – contradicts Supreme Court verdict that anAadhar card not needed for free ART (Acceptability,Accessibility)5) weak referral mechanism between the counsellingand testing centers and the ART centers (Quality)6) negative attitudes of health staff discouragingPLHIV from coming (Acceptability)7) possible technical errors or double counting in thatsome PLHIV enrolled but dropped out of treatment,then repeat their HIV test in different counselling andtesting centers to facilitate re-linkage to treatment(and then counted again) (Quality)8) unavailability of medicines for opportunisticinfections particularly for cryptococcal meningitis,as the cost is no longer supported by MSACS(Accessibility)Availability: Some tests notavailable or machines notfunctioning so people go toprivate diagnostic centersQuality: Doing a better job offollowing the NACO viral loadtesting guidelines (i.e., doingviral load testing as part of routinemonitoring rather than just for thepurpose of screening for failurebefore switching to DTG; bloodsample collection daily vs weekly;partnership with Regional Instituteof Medical Sciences (RIMS) whentheir laboratory is overloaded withblood samples)Health facility infrastructure:-PLHIV experience challenges when going to the ARTcenter to collect ARVs, due to lack of drinking water,washroom/toilet facilities, proper waiting room(exacerbated by large numbers of clients who haveto stand, or end up waiting some distance away fromthe ART Center)-Takes almost a full day to collect monthly doses; longqueuesAvailability:-Baseline clinical tests notavailable at the governmenthospital so went to the privatelab and paid out of pocket-Routine investigation issupposed to be provided freeof cost by the hospital, butmost of the time clinical testwas done at private diagnosticcenter either at own cost orsupported by the NGO due tofrequent machine breakdown-Process is very lengthy andtime consuming since thecounter also serves generalpatients and sometimes staffare discriminatory towardsPLHIVPeople living withHIV and peoplewho inject drugsAvailability:-Access to proper health check-ups by the doctor atthe ART center is challenging - consultations with thedoctor are difficult due to overcrowding of patients;sometimes contact private doctors for consultation-Ratio of counselling staff to clients is inadequateAccessibility (administrative):-Working hours of the ART center is a problem withclosing time being fixed, whereas the opening hoursare not consistent/haphazard-PLHIV are inconvenienced while trying to get theirARVs after travelling long distances due to fixedclosing timing (limited working hour) of the ARTcenter11Financial Accessibility orAffordability: Some cannotafford the test at private centers(USD 30 for all three tests)Quality: Some get tested, butthen do not return to pick uptheir medicines/treatmentbecause the testing canters donot provide the test report** ART Center at JawaharlalNehru Institute of MedicalSciences (JNIMS) has startedproviding ART after completionof a physical examinationwithout requiring CD4 counttests and other baselineinvestigations, though PLHIVare asked to come back to theART center with the testingdocumentation within 15 daysfrom the date of initiationFinancial Accessibility: Some preferto pay out of pocket to go to theprivate clinic for viral load testing toavoid busy clinicsQuality: Most patients at ARTcenters are on DTG, however, someare still on different regimens (e.g.,that include efavirenz or nevirapine)due to clinics wanting to use upexisting drug stocks, based onNACO’s instructions. After stock isfinished, they will be switched toDTG.Availability:-Asked to come for viral load testingafter given an appointment but staffin the laboratory refused to collectthe blood sample giving the reasonthat there were no more slots forthe day (16 had been completedalready), so told to come on the nextblood collection dayAccessibility (administrative):-A viral load test is only offered onWednesday, which is inconvenient
Type ofIntervieweeBarriers to accessing HIV treatmentBarriers to accessingbaseline tests (completeblood count, kidney andliver function tests)Barriers to accessing viral loadtestingAccessibility (financial, physical):Travel allowance of Rs.150 which was previouslygiven to PLHIV has stopped for many years; washelpful for PLHIV coming from long distances; told togive a photocopy of government ID card and bankaccount number for transferring the travel allowancebut it never workedAccessibility (administrative):-Difficult to keep the dateand time of appointments forroutine investigation especiallyfor people from far-off places– if an appointment is missed,need to reschedule-For routine investigation,need outpatient departmentticket and wait a long time in acrowded queue and then thelaboratory is closed when it isthe PLHIV’s turn-Very poor experience atone hospital to get routineinvestigations done as theprocedure was very lengthyand time consuming, standingin a long queue to get a ticketwithout which the clinical testscannot be done (sometimesarriving at 7:30 am and counterdoesn’t open until 9:30am);after getting the ticket, needto go to the ART center toget a requisition form for theclinical investigations, and thenhave to rush to get the blooddrawn before they stop takingsamples due to large volumesof patients - once was deniedat the laboratory and had torepeat the process all overagain; after all that was givena supply of ARVs for 15 days,on three different instances,for not bringing my clinicalinvestigations reportQuality:-Did a viral load test three times,the first two were part of routinemonitoring (the first was not donefor some reason by the laboratory,and a second sample had to beobtained); was advised that thethird time would help decidewhether or not to switch the ARTregimen to DTG, however there wasan error in the report so was askedto test a fourth time in May 2021,but due to the COVID-19 pandemic,the test was not done; remains onthe same regimen-Supported by the NGO to do viralload testing which resulted in theswitch to TLD-Staff advised to repeat the viralload test to see if suitable to switchto DTG, but since then no one hasfollowed up to remind to come forthe test (could be because of theCOVID-19 situation) nor has theinterviewee followed up to make anappointmentAcceptability:-Reluctant to visit ART center because humiliated byhealth facility staff due to frequent interruptions intreatment due to drug habits-Teased and scolded by ART center staff whenappointments missed-Attitude of ART center staff not community-friendly give more support to patients they know; some staffare very friendly and some were very rudeQuality (ART center):-Was not given treatment until CD4 count was 260despite being diagnosed HIV-positive for severalyears- Was advised to start ART without doing a CD4 counttest by a PLHIV-friendly doctor-Several years after starting ART, transferred froma clinic to a hospital to access free service underthe national program, but tenofovir (TDF) was notavailable there so referred elsewhere; the medicalofficer advised to switch from efavirenz to DTG, butthe patient requested to transfer back to the otherhospital due to unfriendly attitudes of the staff- One time, only received sufficient supply of secondline ART for 5-7 days due to shortage of medicinestocks, so had to visit the ART center numerous timesfrom a long distance- Staff are not punctual so have to wait a long time atthe ART center- Was told to take a TB test before ART initiation butblood sample misplaced so did not receive test result- While going to collect monthly ART doses was givenIsoniazid 300mg without any proper counselling onwhy it was given and how it might interact with ART;experienced side effectsQuality (NGO Targeted Intervention program):-NGO accompanied PLHIV to the ART center tosupport ART initiation and follow-up visits; providedvitamins-NGO program helped re-start ART after starting atanother hospital and then stopping due to bad sideeffects (vomiting)12
Table 7: Summary findings from FGDs with PLHIV on barriers to accessing HIV servicesType of Interviewee / Site13SUMMARY FINDINGSPeople living with HIVFGD 1Sites: ART Center JNIMS andART Center RIMS Under the national ART program, ART
Preparedness Coalition (ITPC) as a technical partner, which assisted in training the national partners in India and Indonesia and TREAT Asia staff, and currently hosts the CTO databases of the two sites on its online portal. In collaboration with TREAT Asia, ITPC organized and led trainings on the CTO model, including indicator development, CTO/