Transcription
The quarterly membership publication of the National Hospice and Palliative Care Organization Winter 2017INSIDEHighlights from Factsand Figures2017 StrategicAccomplishmentsA Physician’s PersonalReflectionShort Takes, MemberNews and More HOSPICE LESSONSLEARNEDSurviving the 2017 Hurricanesand Wildfires
Table of Contents6CoverStoryHospice Lessons Learned:Surviving the 2017 Hurricanes andWildfiresNHPCO’s Jennifer Kennedy along with Ted Kennedy from the HHS Office ofEmergency Management spoke with providers who were affected by recentnatural disasters and they provide tips and pearls of wisdom. With theEmergency Preparedness Condition of Participation now in effect, this articleoffers helpful insight.11Las VegasTragedyOne Hospice’sExperience30Social SecurityDisabilityWhile inHospice Care34New VideosRaisingAwareness
1420NHPCO’s report released earlier this year reflects anew methodology for this well-regarded resource;NewsLine shares a snapshot of key statistics.Learn about NHPCO activities from 2017 thatadvance our shared mission and support thehospice and palliative care community.Facts and Figures: Hospice Carein America2017 StrategicAccomplishments26The Other Side of the ConversationDr. Christopher Thompson reflects on his family’s experience andconnects his personal and professional caregiver roles in this powerfulreflection from a hospice physician.Council of States SpotlightA list of 2018 conferences and events from CoS.35Short TakesHelpfulInformation46MemberNews5052News FromNationalHospiceFoundation54News FromWe HonorVeterans
ourEnvisionEdFuturEStrategic planning for the year 2020 and beyond is well underway. In 2018 and 2019, NHPCO will take measurablesteps to create a future that will provide a seamless delivery model from diagnosis to bereavement – the ultimate goalof providing the right care at the right time. This envisioned future unifies hospice and palliative care providers, as wellas the payment stream, under one umbrella.In realizing this vision, NHPCO has developed the following strategic priorities:StrAtEgIc PrIOrItIESContinue to assure access to high quality hospice care to a broad cross-section of patients and families.Broaden the spectrum of services to foster a seamless continuum of care for seriously ill patients and families.Develop a campaign to demonstrate the value of hospice and palliative care services.Expand access to data and analytics to support the efforts of the hospice and palliative care community.Foster an environment of collaboration with other entities focused on serving patients and families.Explore innovative membership models to better meet the needs of the hospice and palliative care community and NHPCO.Expand non-dues revenue sources for NHPCO.MISSIONVISIONVALUESTo lead and mobilize socialA world where individuals andNHPCO believes in:change for improved carefamilies facing serious illness, Service: Engaging Customersat the end of life.death, and grief will experience Respect: Honoring Othersthe best that humankind can offer. Excellence: Exceeding Expectations Collaboration: Fostering Partnerships Stewardship: Managing Resources
Message From EdoAs the year comes to a close, many of us will enjoy time with loved ones. Otherswill find quiet time away from the office to reflect and recharge. Still others –including many of our care providers – will spend this time caring for patients andfamilies. All of us will welcome the New Year and I hope we are able to do thiswith a sense of gratitude for the work we do and the lives we touch.As I reflect upon this past year, I am particularly grateful of the opportunity to serveas your president and CEO. These are important times for all health care providersand I see a wealth of promise as we work collaboratively to build solutions toAmerica’s challenges that we know so well as the leading providers of care forpatients and families with serious and life-limiting illness.Edo Banach on the panel at the NationalAcademies Roundtable.Two weeks ago, I participated on a panel for the National Academies Roundtableon Quality Care for People with Serious Illness. I was able to talk about theimportance of person-centered, family-oriented interdisciplinary care that hasbeen a hallmark of hospice, and I stressed the knowledge that we as a providercommunity have to share with the broader health care system. The NationalAcademies event was followed by a speaking opportunity at the BRG HealthcareLeadership Conference. Hosted in Washington, DC, this conference is designedexpressly for top executives from healthcare, financial, private equity, and policyarenas. It afforded another valuable opportunity for our organization and ourcommunity to contribute to the dialogue about care issues facing society andwhere solutions might be found. Given our collective experience of providinginterdisciplinary, person-centered care, we must be at the table for conversationsabout providing the most appropriate, high-quality care to those with or at risk ofserious illness.As the year comes to a close, I would like to thank each one of you who have doneso much to support NHPCO throughout this busy year. I invite you to look overthe list of representative accomplishments from this past year that you’ll find onpage 20. I also invite you to review NHPCO’s Strategic Priorities (page 4) that willguide our work together.On behalf of our dedicated board member, our staff and our affiliateorganizations, I wish you a peaceful holiday season and a happy New Year!Edo Banach, JDPresident and CEOWinter 2017 NHPCO NewsLine5
HOSPICE LESSONSLEARNED:Surviving the 2017 Hurricanesand WildfiresBy Jennifer Kennedy, MA, BSN, RN, CHCand Ted Kennedy6NHPCO NewsLine Winter 2017
Three major hurricanes in the Eastand devastating wildfires in the Westin August through October 2017were the lead up to Medicarehealthcare providers of all typestesting their recently craftedemergency preparedness plans.Hospice providers were not spared inthese disasters and many of themimplemented their newly mintedemergency plans only months beforethe compliance implementation dateof the emergencypreparedness finalrule for Medicareand MedicaidPrograms(EmergencyPreparednessRequirements forMedicare andMedicaidParticipatingProviders and Suppliers (CMS3178-F)). NHPCO was able to speakwith some hospice providers postdisaster to hear about theirexperience and lessons learned.The Centers for Medicare andMedicaid Services (CMS) developedspecific emergency preparednessregulations to establish nationalemergency preparednessrequirements for Medicare andMedicaid participating providers andsuppliers to ensure that theyadequately plan for both natural andman-made disasters, and coordinatewith federal, state, tribal, territorial,regional, and local emergencypreparedness systems. Hospiceproviders were expected to showcompliance with the new emergencypreparedness Condition ofParticipation (CoP) for emergencypreparedness (§418.113) byNovember 15, 2017.The CoP for hospice providerscontains four main standards thatspecify requirements for the hospiceto develop: an emergency plan,specific policies and procedures foremergency preparedness, acommunication plan, and a programfor preparednesstraining andtesting that isbased on theemergency plan.There are alsospecificrequirements inthe CoP forhospices that havetheir own inpatient facility or are partof an integrated healthcare system.NHPCO would like to thankthe hospice providers fromFlorida and Georgia thattook the time to sharetheir disaster experienceand valuable insight aboutlessons learned.Florida Hospices Chapters Hospice Hospice of Health First Inc Suncoast Hospice Avow HospiceDisaster EventsHurricane Harvey made landfallalong the Texas gulf coast on August25 as a Category Four hurricane. Thestorm moved inland and hoveredover Southeast Texas for days causinghistoric flooding. On the heels ofHarvey, Hurricane Irma hit Floridaon September 10 as a Category Fivehurricane bringing high winds andlife-threatening storm surges. At itsstrongest, the storm’s wind speedshovered around 185 mph, with gustsof more than 215 mph. Irma made itsway to Georgia as a tropical storm onSeptember 11 generating tropicalstorm-force winds and flash foods. Gulfside Hospice andPasco Palliative Care, Inc Tidewell HospiceGeorgia Hospice LHC Group - GAvWinter 2017 NHPCO NewsLine7
continued from previous pageLess than a week later, CategoryFive Hurricane Maria devastatedPuerto Rico with flooding anddestruction of its recently damagedelectrical grid from hurricane Irma.before, during and after all ofthese disaster events to keep theirpatients safe and ensurecontinuation of hospice services tothe best of their ability.As hurricane recovery wasunderway in the East, multiplewildfires broke out in California inlate Summer and early Fall causinglarge scale damage to land andhomes, and causing thousands ofpeople to evacuate from theirhomes and community. Hospiceproviders in Texas, Florida,Georgia, Puerto Rico, andCalifornia implemented theiremergency preparedness programsLessons LearnedNHPCO was able to speak with 10hospice providers from Florida andGeorgia post Irma and severaladditional providers from Californiaafter the wildfires about theirdisaster experience and lessonslearned. No matter the disastertype, all providers agreed thatpre-disaster planning was critical inpreparing for what was to come.As part of their disasterpreparedness practices, providersin Florida completed disasterassessments and preparation planswith each patient as they areadmitted to service. Theydetermine what the patient andfamily’s plan would be if a disasteraffected their community andeducate them about the hospiceprovider’s emergency plan. It isimportant to know if patients andfamilies plan to shelter in place orevacuate. If they plan to evacuate,providers needs to know where thepatient is going and if the hospiceneeds to make travel or temporaryinpatient facility arrangements.There are many moving partshappening when a disaster isapproaching and pre-planning asmuch as possible can reduce asignificant amount of stress forboth the hospice provider and theirpatients. Coordination of services,supplies, staff, medications, andeverything else that may be neededpre and post disaster requires adetail oriented approach, out of thebox thinking, and diligent followup. For example, one Floridaprovider shared that theycoordinated the provision of tirerepair for their staff post disaster.Hurricanes cause debris on roadsand debris causes flat tires. Staffmembers who were able to visitpatients after Irma experienced tireissues because of debris, but theyhad access to tire repair because ofthis hospice provider’s out of thebox thinking, planning, andcoordination.8NHPCO NewsLine Winter 2017
As each disaster approached, providers kept in constant communication withtheir county emergency management agency (EMA) and with their patients.It was important to confirm that hospice plans were integrated into thecounty’s emergency plans and hospice patient needs were recognized. Anexample of this coordination included working with the county EMA relatedto provision of designated care areas in shelters that was suited to the uniqueneeds of hospice patients. Field staff reconfirmed each patient’s plan andreinforced messages related to mandatory evacuation and safety. Providerstook proactive measures to ensure that they could support all of theirpatients so they stopped admitting patients a week before Irma madelandfall, they arranged travel contracts for patients that were leaving thearea, and pre-registered patients for placement in special needs shelters whowere unable to travel or wanted to stay in the area.One Florida provider closed and evacuated their inpatient unit because itwas in Irma’s predicated path and at high risk. They never closed theirinpatient facility before, but with a plan, they were able to successfullyrelocate every patient to a safe temporary facility with no issues. Luckily,their inpatient unit sustained very little damage and they were able to moveback once power was restored.All providers agreed that having a well-developed and rehearsed emergencyplan was essential to them being prepared, but even the best planningcannot mitigate all problems, particularly post disaster. It is difficult to knowthe extent of damage after an incident and the long term ramifications whendeveloping a plan proactively. Florida providers prepared for everything thattheir past experience taught them, but no one was prepared for such longterm power outages, fuel shortages, and patients and staff not being able toreturn to their homes for an extended period or not at all.A rule of thumb in disasterpreparedness is to beready to self-sustain for3-5 days.A rule of thumb in disaster preparedness is to be ready to self-sustain for 3-5days. However, this recent string of disasters has left providers and patientswithout power and sometimes re-supply for weeks. Some providers inFlorida and Puerto Rico are essentially starting from scratch related to theircensus because their patients evacuated and cannot return to their homes,or their staff has been reduced for similar reasons.Pearls of WisdomProviders from Florida shared insight with NHPCO about actions thathelped them prepare for the disaster and observations that will update theiremergency preparedness plans for the future. P rovide real cash advances to staff before a disaster event. ATMmachines and credit card processors will not work during power outagespost disaster and cash may be the only currency accepted to buy gas,food, and supplies.Winter 2017 NHPCO NewsLine9
continued from previous page T ake care of your staff. Give them time before thestorm to take care of their family and makearrangements. Plan for the potential support of staff and familieswho may lose their home. One hospice providercoordinated shelter, clothing, childcare, meals, andlaundry help for several staff members and theirfamilies who lost everything during Irma. C oordinate with the state and local emergencymanagement agency to discuss staging areas forsupplies, fuel, generators, and charging stations.Homecare providers in Florida were using their carsto charge their cell phones because of extendedpower outages. T hink out of the box to solve problems. One Floridaprovider asked Verizon to ship 50 charged cellphones for staff pre-disaster to ensure they had cellphone communication ability as long as possible.Another provider used Zello, a Walkie-Talkie appthat works via Internet, to communicate with staffwhen cell phone service was down. C ommunicate with providers outside of your servicearea pre-disaster to discuss care and placement ofpatients as needed.10NHPCO NewsLine Winter 2017 Arrange travel contracts with hospice providers tomaintain hospice service Develop memorandums of understanding withtemporary facilities for inpatient careResourcesNHPCO developed an emergency preparednessresource guide and other resources in 2017 to helphospice providers with compliance requirements. Thisresource will be updated in early 2018. The U.S.Department of Health & Human Services, AssistantSecretary for Preparedness and Response (ASPR), alsodeveloped a healthcare emergency preparednessinformation gateway website called TechnicalResources, Assistance Center, and InformationExchange (TRACIE) to meet the needs of healthcarecoalitions, healthcare providers, healthcare providers,emergency managers, public health practitioners, andothers working in disaster medicine, healthcare systempreparedness, and public health emergencypreparedness. Access NHPCO resources and link toTRACIE from our Emergency Preparedness webpage.Development, testing, and maintenance of anemergency plan is now a CoP for hospice programs. Itwould benefit providers to treat their plan as not just aregulatory requirement but as a roadmap to guide themthrough pre and post disaster action.
Jennifer Kennedy, MA, BSB, RN, CHC, is Senior Director ofRegulatory and Quality for NHPCO and has been with theorganization since 2006. She has more than 30 years of experience asa leader and nurse in diverse healthcare settings and has worked inhospice and palliative care for the last 18 years.NHPCO developed anemergency preparednessTed Kennedy is a Senior Emergency Management Specialist with U.S.Department of Health and Human Services in the Operations Divisionof the Office of Emergency Management, under the Office of theAssistant Secretary for Preparedness and Response. He has served invarious positions in the Operations Division since 2006 including anassignment for over a year as the Division Director.resource guide and otherresources in 2017 Printer-Friendly PDFLAS VEGAS TRAGEDY: LESSONSFROM ONE HOSPICE PROVIDERby Jon Radulovic, NHPCO Vice President, CommunicationsNHPCO staff had the opportunity to speak with KimAnderson, Infinity Hospice Care’s Vice President ofBusiness Development, and her colleague TracySundberg, RN, Executive Director, regarding ways thattheir organization responded following the Octobershooting in Las Vegas. They hope that by sharing theirexperience, they might give other organizations somethings to consider in crafting emergency response plansand community relationships.Communities often lean on the support and expertisethat hospice can offer when tragedies involving loss oflife occur. There are countless stories of hospicebereavement counselors going above and beyond theireveryday job duties in times of need – from rushing to aschool after a car accident that claimed a young life, tooffering grief support to a local business thatexperienced the unexpected loss of a beloved colleague,to opening its doors for grief support groups that aredeveloped in response to a community’s unique needs.On October 1, 2017, worldwide attention turned to LasVegas following the tragic shooting at an outdoor musicfestival where 58 people died and 546 people wereinjured. The entire Las Vegas community was affectedby the scale of this tragedy – and several hospiceprograms in the area have provided counseling andother forms of support. Examples of the responseactivities include Nathan Adelson Hospice setting up ahotline for community partners to call for support;Community Hospice & Palliative Care and HoffmannHospice Home both offering grief support sessions andcommunity presentations following the tragedy. InfinityHospice Care sent credentialed staff to UMC TraumaCenter the night of the shooting and are involved in thegrief counseling center established by Clark County.October 1News quickly spread throughout the city that therehad been a shooting that involved possible deaths andsignificant injuries. As first responders and cityWinter 2017 NHPCO NewsLine11
continued from previous pageservices went into action, many community providerorganizations began to track the activity. As the extentof the tragedy became apparent, staff at InfinityHospice Care took action.Accounting for Staff and PatientsAt 5:30am, the organization’s emergency response phonetree was activated to contact all staff and ensure that allpatients were accounted for. By 9:00am, 120 staff and allpatients & families had been contacted. Fortunately, noone working for or being cared for at the hospice waskilled or severely injured, yet almost everyone knewsomeone who was affected by the shooting.The organization’s emergency phone tree had been putinto place in preparation of the new Condition ofParticipation (that went into effect on November 15, 2017).At the time it was being developed, staff thought it was alot of work for something that might not ever be used.However, it was used – sooner than anyone could haveimagined – and it worked just as it had been designed.Staff Support at UMC Trauma CenterOnce staff and families were accounted for, and thescope of the shooting became clear, hospice staffwanted to step up and make their skills available.University Medical Center is the only LEVEL I traumacenter in Nevada. A number of clinical professionals atInfinity Hospice are credentialed to work at UMC. Manyof them responded to offer support. As it turned out,serving food to the UMC medical professionals whowere in disaster response mode was one of the criticalneeds at that time. Ensuring that these professionalshad nourishment as they responded to the growingnumber of shooting victims was not a job that could bedelegated to any volunteer – staff from Infinity weremore than willing to do what they could to keep themedical personnel functioning as effectively as possible.An Important Skill SetHospice and palliative care professionals are trained atdealing with issues surrounding death, dying, and loss– while this is obvious to those in the field, there aresome outside of the community unfamiliar with theskills of the interdisciplinary team. Professionals in our12NHPCO NewsLine Winter 2017field know how to listen, to coordinate, and to refer, allin response to the individual needs of the person beingcared for. These are abilities that are valued in times ofemergency response. As part of their response, InfinityHospice made sure that they were included on a list ofservice providers developed by the City CrisisManagement Team.The site of the tragedy was one familiar to everyone. Thenumber of people traumatized by this shooting wasextensive. What has become apparent in the weeks andmonths following the shooting are the wide range ofindividuals in need of support. Many who were presentat the tragedy but did not sustain physical injuries wereunsure if there needs warranted support, particularlygiven the scale of the situation. Many without physicalinjuries felt that they should not use resources that mightbe needed for the severely injured.Hospice staff volunteering through coordinated effortsof the Red Cross created an intake form that nurses andsocial workers used to assess the needs of those seekingassistance. A 24/7 counseling call line was set up.Active listening, an innate skill for hospiceprofessionals, was essential during this period andallowed for the quick identification of needs andnecessary referrals.The Extend of TraumaAs one would expect, hospices have stepped up to providecounseling support to the community and in the shorttime since the shooting they have served manytraumatized individuals. The impact on people’s lives hasvaried greatly. For example, many of those working at theoutdoor music venue were contract employees, so withthe closure of that entertainment space, they have losttheir employment and means of supporting their families.Many of those same employees do not have access to EAPor human resource departments to help them deal withthe trauma of that night. Hospices are meeting theseneeds and more. Weekly support groups have beenestablished and will continue as long as they are needed.Some of the professionals who responded to the scene andhave taken advantage of counseling services and support
that the hospice has made availableinclude 911 operators, night staff atfuneral homes who were overwhelmedon October 1, and even Red Crossvolunteers who were not fully trainedyet were called into service due to themagnitude of the tragedy.A Safe PlaceThe offices of Infinity Hospicebecame a center of support for thoseon staff who stepped up to serve. Theatmosphere in the city could bedescribed as chaotic at best, and itwas necessary to have a place wherehospice staff could find a safe placeto talk about what they wereexperiencing, find food andnecessary sustenance, and knowthere was a place where they couldget centered and grounded.Leadership SupportSupport to the community and to theInfinity staff came right from the top.Mary Bertram, president, DarrenBertram, CEO, and Brian Bertram,vice president made sure that theorganization’s commitment was clearand strongly affirmed. A core valueof the organization is “making adifference in the lives of others.” Thisis not just about hospice patients, butall people. The opportunity to engagewith the community in many waysreflects this core value.Team members were not obligated tovolunteer in the response efforts, yet90 percent of the licensed staff atInfinity Hospice stepped forward toaddress the needs of the community.And staff time dedicated to responseefforts were done and continue to bedone during the employee’sscheduled work time. No one wasexpected to donate their free time toresponse efforts.Lessons for the FutureThe team from Infinity Hospice hasbeen able to take some time to assesstheir response and they offered somethoughts about steps they areconsidering as they build on theiremergency response plan: T hey will take advantage ofcritical incident training coursesavailable online for staff.R to L: Tracy Sundberg (R)and Kim Anderson (L)of Infinity Hospice Care with Clark CountySheriff Joseph Lombardo at the Night ofHealing event co-sponsored by Infinity. T hey will look at what would berequired to be a possibleemergency triage site for thecommunity for a future large-scalepublic emergency. hey hope to be an official Tdesignated blood donation centerin times of emergency. T hey are strengtheningcommunication and relationshipswith local emergency responders,the city’s crisis managementprogram, and other serviceproviders so coordination ofefforts can happen as seamlesslyas possible in times of need.Dee Williams NCCA, LCPC of Infinity HospiceCare lead a team to support the 911 operatorsthat were on duty the night of October 1.One of the most powerful examplesof the value of their response effortshas been the knowledge that manytraumatized citizens of Las Vegashave learned that they are not aloneand that caring and compassionatesupport is available to help them copewith this life-changing event.Printer-Friendly PDFWinter 2017 NHPCO NewsLine13
FactsandFigures:Hospice Carein AmericaHighlights from the new report released by NHPCO14NHPCO NewsLine Winter 2017
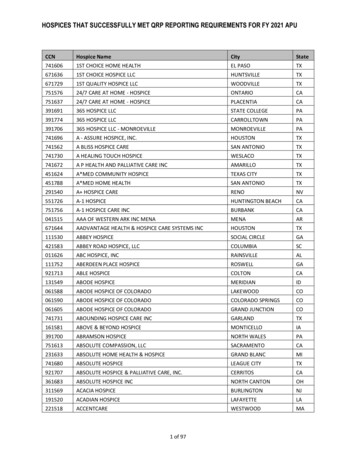
NHPCO Facts and Figures: Hospice Care in Americaprovides an annual overview of hospice care delivery.This overview provides specific information on: H ospice patient characteristics Location and level of care Medicare hospice spending Hospice provider characteristics Volunteer and bereavement servicesIn order to ensure this annual report is as accurate and useful as possible to thefield, NHPCO’s research team is using a new methodology for creating the reportand CMS data is the primary data source, specifically, CMS hospice claims dataincluded in the hospice standard analytical file Limited Data Set.The Hospice Cost Reports, also available from CMS, provided supplementalinformation. The NHPCO National Data Set is the data source for the Volunteerand Bereavement statistics. The MedPAC March 2017 Report to Congress is thedata source for discharges and transfers. This is a significant change from themethodology used in previous editions of NHPCO’s facts and figures report.NHPCO’s research team isusing a new methodologyfor creating the reportand CMS data is theprimary data source.The new report is officially the “2016 Edition” that contains 2015 data. Early nextyear, NHPCO will release the “2017 Edition” that will reflect 2016 data.What follows are representative statistics and graphs from the report.WHO RECEIVES HOSPICE CAREHow many Medicare beneficiaries received hospicecare in 2015?1,381,182 Medicare beneficiaries were enrolled in hospice care for one day ormore in 2015. This includes patients who: Died while enrolled in hospice Were enrolled in hospice in 2014 and continued to receive care in 2015 Left hospice care alive during 2015 (live discharges)Winter 2017 NHPCO NewsLine15
continued from previous pageFIGURE 2. GEOGRAPHIC VARIATION IN THE PROPORTIONOF MEDICARE DECEDENTS WHO DIED WHILERECEIVING HOSPICE CARE IN 2015What proportion of Medicare decedentswere served by hospice in 2015?Of all Medicare decedents in 2015, 46% receivedone day or more of hospice care and were enrolledin hospice at the time of death.As illustrated in Figure 2, the proportion of Medicaredecedents enrolled in hospice at the time of deathvaried across states from a low of 24% to a high of57%.Principal DiagnosisTABLE 3. PERCENTAGE OF PATIENTS BY PRINCIPAL DIAGNOSISPrincipal DiagnosisPercentageThe principal hospice diagnosis is the diagnosis thathas been determined to be the most contributory tothe patient’s terminal prognosis. In 2015 moreMedicare hospice patients had a principal diagnosisof cancer than any other disease.Cancer27.7 %Cardiac and Circulatory19.3 %HOW MUCH CAREIS RECEIVED?Dementia16.5 %Days of Care*Respiratory10.9 %In 2015 hospice patients received a total of96,052,577 days of care paid for by Medicare.Stroke8.8 %Other16.7 %TABLE 4. DAYS OF CARE BY PRINCIPAL DIAGNOSISPrincipal DiagnosisMean #Days of CareMedian #Days of CareCancer47 days19 daysCardiac and Circulatory76 days28 daysDementia105 days56 daysRespiratory69 days19 daysStroke77 days20 daysOther61 days16 days* These values are computed using only days of care that occurred in 2015.Days of care in 2014 and/or 2016 are not included for patients who received care in those years as well. Days of care have been combined forpatients who had multiple episodes of care in 2015.16NHPCO NewsLine Winter 2017In 2015, on average, patients with a principaldiagnosis of dementia received the largest number ofdays of care.Length of Service*The average length of service (ALOS) for Medicarepatients enrolled in hospice in 2015 was 69.5 days.The median length of service (MLOS) was 23 days.A larger proportion of Medicare patients (28.2%)were enrolled in hospice a total of seven days orfewer compared to all other length of servicecategories.In 2015 close to 30% of patients were enrolled inhospice for 7 days or less.
FIGURE 3. PROPORTION OF PATIENTSBY DAYS OF CARE IN 2015TABLE 5. DAYS OF CARE CATEGORIES BYPERCENTAGE OF PATIENTSTotal Days of Care91-180 days11.9% 180 days13.1%61
reflection from a hospice physician. 20 2017 Strategic Accomplishments Learn about NHPCO activities from 2017 that advance our shared mission and support the hospice and palliative care community. 14 Facts and Figures: Hospice Care in America NHPCO's report released earlier this year reflects a new methodology for this well-regarded resource;