Transcription
7/10/2014Idiopathic Toe Walking: CurrentConcepts in Evidence-BasedPracticePresented byBetty A. McNeff PT, DPT PCSSurvey QuestionCourse ObjectivesBy the end of this course the student should be able to:1.Define and discuss toe walking from a historical perspective to current accepted concepts.2.Compare and contrast toe walking associated with disease and toe walking in the absence ofa medical condition.3.Identify and discuss a comprehensive evaluation for a patient referral due to toe walking.4.Analyze and synthesize current research and clinical criteria in the diagnosis of idiopathictoe walking.5.Describe and apply current research findings on gait kinematics and kinetics in idiopathictoe walkers.6.Analyze and synthesize current research into suggested relationships with other bodysystems.7.Discuss and analyze the proposed long-term consequences of idiopathic toe walking for thepurpose of supporting an appropriate plan of care.8.Identify and discuss current evidence-based management options in the treatment ofidiopathic toe walking.9.Identify the indications, contraindications, risks, and benefits of the different managementoptions available for the treatment of idiopathic toe walking.10. Discuss the role of the physical therapist as a part of an inter-professional team member inthe management of idiopathic toe walking.11. Discuss and analyze current evidence-based physical therapy intervention protocols in themanagement of idiopathic toe walking.12. Discuss and analyze an evidence-based physical therapy clinical practice algorithm in themanagement of idiopathic toe walking from referral to discharge.1
7/10/2014Definition Toe walking is the absence orlimitation of heel strike in thegait cycle Toe walking: symptom of diseaseprocesses, trauma, neurological dysfunction Idiopathic Toe walking: in the absence of medicaldiagnosis First described by Hall et. al. in 1967: “congenitalshort tendo calcaneus” Video Clip: 3 year old toe walkerhttp://www.youtube.com/watch?v IQRkSrmcH5EEtiology**UnknownSpeculations: Sensory processing deficits caused by lack ofbarefoot walking in developed countries Myopathy: different proportions of Type 1muscle fibers in gastrocsoleus found on biopsy Genetics/Family history (autosomal dominant)General Points Toe walking is a natural part of gait development:-Wide BOS, hips ER, knees flexed, ankles PF Considered normal up to the age of 2 years Considered “idiopathic” if it persists beyond age 2years in the absence of other medical diagnosis. Treatment for ITW is complex due to its unknownetiology. Research available on expensiveapproaches while lacking inconservative managementoptions.2
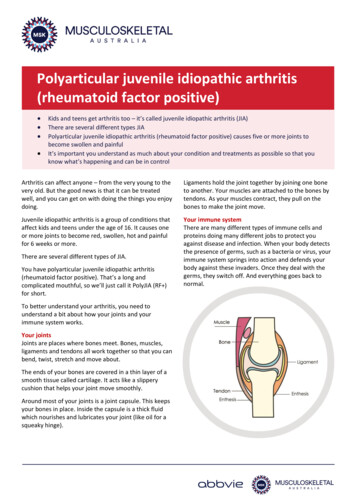
7/10/2014EvaluationRequires thorough evaluation1.History-Birth history-Past medical history-Developmental milestones (particularly related to gait)-Family history2. Physical Examination-Thorough neuromuscular exam (sensation, tone, strength, ROM, deeptendon reflexes)-Integumentary (skin inspection)-Pain assessment-Gait analysis-Speech/language and Sensory processing screen3. Diagnostic Tests (if warranted)-EMG activity, muscle biopsy (myopathy), blood test (creatinephosphokinase levels), Toe Walking ToolPolling Question #1Diagnosis Persisting beyond age 2 Heel accelerometry data: being tested with heel sensors in boot. Medical conditions associated with toe walking must be ruled out:neurological or orthopaedic conditions, physical injuries Classic presentation: Neurologically normal Normal muscle strength and selective musclecontrol Prefer to walk on balls of feet Varies in form and frequency: bouncing to tip toe 100% time to intermittent Normal or tight ROM heel cords Most can self-correct (use a heel-toe pattern) whenprompted Self Corrected Toe Walking Gait Video3
7/10/2014Polling Question #2Kinematic Profiles:Cerebral Palsy versus ITWCPITW Ankle: Sagittal plane: lack of 1 strocker Knee: Sagittal plane: flexion duringstance phase Frontal plane: significantdisruptions*additional impairments: deficits instrength, balance, selectivemotor control. Ankle: Sagittal plane: significant increase ofplantarflexion during stanceand swing phase of gait initial swing dorsiflexionfollowed by suddenplantarflexion midwaythrough swing phase Frontal plane: Normal Knee: Sagittal plane: mild kneehyperextension during stancephase Frontal plane: NormalKinetic Profiles-ITW1st Rocker (heel strike, eccentriccontraction of anterior tibialis): Absence of ankle DF moment Loading response power absorptionphase2nd Rocker (midstance, eccentriccontraction of gastrocsoleus): Elevated PF moment Power generation phaseSwing Phase (concentric contraction of anterior tibialis): Increased PF3rd Rocker (terminal stance “push off”, concentric contraction ofgastrocsoleus) Diminished PF moment Diminished ankle power generation phase4
7/10/2014Gait Cycle Profile-ITW(Westberry et. al., 2008)Prevalence Small studies report up to 7% rate in generalpopulation Problem: cultural bias and small sample sizesmake it difficult to generalize to entirepopulation (prevalence unknown). Genetic basis exists (family history) No sex differences (1:1 ratio)Polling Question #35
7/10/2014Relationship to Motor DevelopmentCharacteristics of Typical Early Ambulation: Limited ankle strength push-off absent Compensation co-contraction ofopposing muscle groups Initial heel strike appears at approximately age 18-24months Forward inclination of body to erect trunk Co-contraction to reciprocal activation Heel strike with active dorsiflexion: after age2 yrs Push off with active plantarflexion: refined up toage 4-5 years Reaching mature level: age 7-8 yearsRelationship to Other Systems Handedness: a left hand dominance associationhas been described(Williams et. al., 2011) Sensory Processing: the neurological process that organizes sensation fromthe body and environment in order to effectivelyrespond to such stimuli. Sensory processing dysfunction: a failure in thisprocess. Tactile defensiveness and deficits in proprioceptionare speculated to contribute most to ITWITW and NeuropsychiatricSymptomsEngstrom et. al., 20126
7/10/2014Long-Term Consequences? The natural history of ITW is mixed Habitual toe walking Shortened Achilles tendon/contracturedevelopment External tibial rotation Improper balance/increased risk of falling:center of mass shifted anteriorly Slower running speeds/shorter strides to compensate forbalance deficits Increased weight bearing on metatarsal heads/forefoot anddecreased weight bearing on heel: early on this reduces heelbone development leading to risk of pain when child is forcedto bear weight onto heels later in life.Polling Question #4Treatment Options Nonsurgical Management: Physical TherapyFootwearOrthoticsWhole body vibration? (Williams et. al, 2013)Casting/Serial casting*Botulinum toxin A* Surgical Management: Surgical lengthening of triceps surae muscle-tendoncomplex**have best evidence for improved outcomes7
7/10/2014Footwear/Orthotics Most support based on clinicalopinion Suspected mechanisms of action provides tactile input that maychange neurological input andinfluence gait pattern Provides a mechanicaladvantage that alters motionand influences gait pattern Full length carbon fiber footorthosis Plantar-flexionstop/Dorsiflexion assist Night time bracingWhole Body Vibration No research exists in children with ITW Current available evidence: improvementsin muscle length and strength after shortbursts of whole body vibration. Current research question (Williams et. al., 2013):Will whole body vibration have an immediatemechanical and/or neuro-modulation effect on gaitpattern and heel strike?Serial Casting Most evidence exists (with or without Botulinum ToxinA) Postulated mechanism of action: Elongation of noncontractile elements and increase in number ofsarcomeres. Complications: Skin irritation Pressure wounds Permanent tissue damage(Less likely in ITW population due to normal skinsensation in these children)8
7/10/2014Botulinum Toxin AAt recommended doses, complications are rare: Localized: muscle weakness and pain at injection site(temporary, few weeks) Systemic: Flu like symptoms 2-3 daysAt higher doses: Bladder dysfunction: injections to LE muscles Dysphagia (difficulty swallowing): injections to UE and neckSmall cases of death in children with CP GMFCS V duringadministration of large doses under general anesthesiaContraindication: Fixed contracturesBotulinum Toxin A Casting(Engstrom et. al., 2013)Randomized controlled trial26: Casting only (to neutral, 1X for 4wks)21: Casting Botulinum Toxin A (4 injections distal/proximal calf)Baseline Pre-, 3-month Post-, 12 months Post-treatment testingResults: No difference between groups Both groups showed improvement in ankle ROM, frequency of toewalking, and several gait parameters. 38/47 children still toe walked to some extent (only nine ceased toewalking) Neuropsychiatric problems had no influence of treatment effectsLimitations: small sample size, no control group (withoutintervention), some children revealed group allocation to PTevaluator, parent questionnaire regarding toe walking frequency isused not a validated toolSurgical Management Indications: fixed contractures unresolved cases following non-surgical management. Complications: Post operative infectionTendon necrosisDeep vein thrombosisSensory LossOver-correction or over-lengthening9
7/10/2014Over-lengthening and Crouch GaitSurgical Lengthening Considerations Must first determine the location of the posterior tightness. Gastrocnemius, Soleus, or Both Silfverskiöld test: examine the patient supine with knee extended,than flexed. Dorsiflexion limited with knee extension only: Gastroc Dorsiflexion limited with knee flexion only: Soleus Dorsiflexion limited with knee flexion and extension: BothSurgical Lengthening ProceduresGastrocnemius tightness Gastrocnemius LengtheningSoleus tightness Musclelengthening more distalapproaching the muscletendon junctionBoth percutaneous Achillestendon lengthening(Oetgen & Peden, 2012)[Watch video clip of post-opcase]10
7/10/2014Physical Therapy ManagementMotor PerformanceTreatment Dorsiflexion ROMGoal: 10 degrees of DF2. Dorsiflexion Strength1.1.Passive, active, and positionalstretching of gastrocnemiusand soleus2. Stretching of trunk and otherLE muscles3. Strengthening of trunk and LEmuscles:-NMES, taping, resistive ex,gait training4. Manual therapy-massage, joint mob5. Home program6. EDUCATIONDorsiflexion ROM and Strength Manual stretchingPositional stretching gastroc: orthotic prescriptionSelf stretching (standing at wall, off step, or long sitting with belt)Standing on incline/wedgeKicking a ballStair climbing or step upsWalking up an incline (i.e. ramp or inclined treadmill)Squatting or stooping (picking up objects from floor, heel down)Walking backwards on treadmill or pulling a toyHeel or “duck walking” (HEP: pick a hallway)Walking with swim flippersCyclingTheraband: active dorsiflexionToe raises (seated or standing)Kinesiotaping: facilitation technique, anterior tibialisNMES: neuromuscular E-stim or FES (anterior tibialis)Gastroc Strengthening Heel raises off step Plyometrics: vertical and broad jumps (initiatedwith heel contact) Theraband exercises: plantar flexion Heel toe pattern gait training Treadmill/ground Up an incline Kinesiotaping: facilitation of gastroc during fulllength training. NMES or FES (gastrocsoleus)11
7/10/2014Stretching/Strengthening of Trunk andOther LE muscles Prone extension or “superman”All 4’s alternate extensionWall or knee push upsTheraband: back rows, scap retraction, chest pressSit ups/crunches/plankLungesChair squats/wall sitsBridges (single and double leg)Therapy ball activities to strengthen core and pelvisSingle leg stance training (stable to unstable surfaces)Beam walkingBall toss (weighted balls)Polling Question #5Motor Control-Based Intervention(Clark et.al., 2010):1. Stair stepping strategy (3 min)2. Standing balance (DL/SL) X 60 seconds3. Stooping activity (50 reps/hour)4. Controlled stepping and heel toe practice5. Sensory and intrinsic foot activities6. Age appropriate motivation7. Information for parents8. Home activitieshttp://links.lww.com/PPT/A1912
7/10/2014http://www.youtube.com/watch?v QPd4GnSIHw0http://www.youtube.com/watch?v 2dbl2LXAlrIPT Management Algorithm(LeCras et.al., 2011)PT Treatment Algorithm(LeCras et. al., 2011)13
7/10/2014Discharge from PT1. If child/family are noncompliant with therapyand HEP.2. If child has met established goals:-Ankle PROM DF at least 10 degrees-Heel-toe pattern frequency 75 % time-Independence with HEP(LeCras et al., 2011)-Age-appropriate gross motor skillsQUESTIONS?Thank you for your interest! If youhave further questions, I can bereached at:bamcneff@gmail.comReferencesClark E, Sweeny JK, Yocum A, McCoy SW. (2010). Effects of motor control intervention for childrenwith idiopathic toe walking: A 5 case series. Pediatric Physical Therapy, 22: 417-26.Dietz F, Khunsree S. (2012). Idiopathic toe walking: to treat or not to treat, that is the question.Iowa Orthopaedics Journal, 35: 184-188.Engelbert R, Gorter JW, Uiterwaal C, van de Putte E, Helders P. (2011). Idiopathic toe-walking inchildren, adolescents and young adults: a matter of local or generalised stiffness? BMCMusculoskeletal Disorders 12:61.Engstrom P, Bartonek A, Tedroff K, Orefelt C, Haglund-Akerlind Y, Gutierrez-Farewik EM. (2013).Botulinum toxin A does not improve the results of cast treatment for idiopathic toe-walking: arandomized controlled trial. Journal of Bone and Joint Surgery, 95 (5): 400-407. doi:10.2106/JBJS.L.00889Engstrom P, Gutierrez-Farewik EM, Bartonek A, Tedroff K, Orefelt C, Haglund-Akerlind Y. (2010).Does Botulinum toxin A improve the walking pattern in children with idiopathic toe-walking? JChild Orthop 4:301–308; DOI 10.1007/s11832-010-0263-9Engstrom P, Tedroff K. (2012). The prevalence and course of idiopathic toe walking in 5 year oldchildren. Pediatrics, 130: 279-84; doi:10.1542/peds.2012-0225.Engstrom P, Van’t Hooft I, Tedroff K. (2012). Neuropsychiatric symptoms and problems amongchildren with idiopathic toe-walking. Journal of Pediatric Orthopaedics, 32: 848-52.14
7/10/2014ReferencesFaust KA. (2011). The acute effect of whole body vibration on gait parameters in adultswith cerebral palsy [Masters]. Indiana, IN: Ball State UniversityLe Cras S, Bouck J, Brausch S, Taylor-Haas A; Cincinnati Children's Hospital Medical Center:Evidence-based clinical care guideline for Management of Idiopathic Toe -therapy-physical-therapy/, Guideline 040, pages 1-17, February 15,2011.Oetgen ME, Peden S. (2012). Idiopathic toe walking. Journal of the American Academy ofOrthopaedic Surgery, 20: 292-300; http://dx.doi.org/10.5435/JAAOS-20-05-292McMulkin ML, Baird GO, Caskey PM, Ferguson RL. (2006). Comprehensive outcomes ofsurgically treated idiopathic toe walkers. J Pediatr Orthop 26(5): 606-611.Pendharkar G, Percival P, Morgan D, Lai D. (2011). Automated method to distinguish toewalking strides from normal strides in the gait of idiopathic toe walking children fromheel accelerometry data. Gait and Posture 35: 478-482.Pistilli EE, Rice T, Pergami P, Mandich MB. (2014). Non-invasive serial casting to treatidiopathic toe walking in an 18-month old child. Neuro Rehabilitation 34:215-220.Solan MC, Kohls-Gatzoulis J, Stephens MM. (2010). Idiopathic toe walking and contracturesof the triceps surae. Foot Ankle Clin N Am, 15:297–307; doi:10.1016/j.fcl.2010.01.002Westberry DE, Davids JR, Davis RB, Cesar de Morais Filho M. (2008). Idiopathic toe walking:a kinematic and kinetic profile. Journal of Pediatr Orthop, 28: 352-58.ReferencesWilliams CM, Tinley P, Rawicki B. (2014). Idiopathic toe walking: have we progressed in ourknowledge of the causality and treatment of this type of gait? J Am Podiatr Med Assoc;104 (3): 253-62Williams CM, Tinley P, Curtin M, Wakefield S, Nielson S. (2014). The motor skills and sensoryprocessing abilities associated with idiopathic toes walking gait. Journal of ChildNeurology; 29 (1): 71-78.Williams CM, Michalitsis J, Murphy A, Rawicki B, Haines TP. (2013). Do external stimuliimpact the gait of children with idiopathic toe walking? A study protocol for a withinsubject randomised control trial. BMJ Open; 3:e0002389. doi:10.1136/bmjopen-2012002389Williams CM, Tinely P, Curtin M. (2010). Idiopathic toe walking and sensory processingdysfunction. Journal of Ankle and Foot Research, 3:16Williams CM, Tinely P, Curtin M. (2010). The toe walking tool: A novel method for assessingidiopathic toe walking children. Gait and Posture, 32: 508-11.Williams CM, Tinely P, Curtin M, Nielson S. (2011). Hand preference in children with anidiopathic toe walking gait. Acta Paediatrica: e140-e141; DOI:10.1111/j.16512227.2011.02512.x15
purpose of supporting an appropriate plan of care. 8. Identify and discuss current evidence-based management options in the treatment of idiopathic toe walking. 9. Identify the indications, contraindications, risks, and benefits of the different management options available for the treatment of idiopathic toe walking. 10.