Transcription
2017 Annual MeetingPROGRAM and AbstRActsOctOber 27– 28, 2017StOwe, Vt
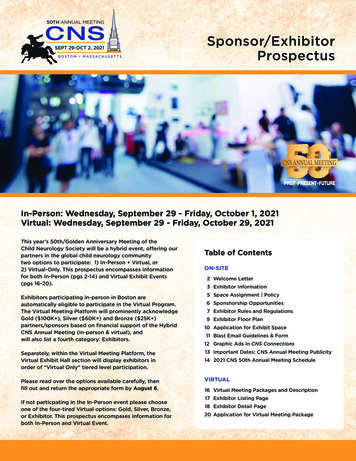
Welcome to Stowe and the2017 NNECOS Annual Meeting!Thank you for joining us at this year’s annual meeting at the StoweflakeMountain Resort. Our planning committee is pleased to present a carefullythought out program of concise, interactive, interdisciplinary sessions withmeaningful takeaways to bring back to your practice. We invite you totake advantage of the additional networking time built into the scheduleto network with colleagues from across the region. Now, more than ever,professionals must participate in the political, economic, and scientificdebates that challenge the cancer care community nationwide.As you enjoy the delicious refreshments in the Atrium and Collins Receptionareas, please take the time to visit with our exhibitors and thank themfor supporting this meeting. A special note of thanks to the 24 companiessupporting the society as corporate members this year!At the conclusion of the meeting, we ask that you complete and submityour evaluation, allowing you to obtain educational credit, and providingfeedback to help shape future educational events.2017 Annual Meeting Planning CommitteeSteven Ades, Lori Aubrey, Diana Barnard, Erica Bernhardt, BrendaClements, Amelia Cullinan, Andrew Hertler, John Hill, Thomas Keating,Rodrigo Maegawa, Elizabeth McGrath, Ken Meehan, Carl Nelson, TomOpenshaw, Sunil Patel, Hibba Rehman, Shirley Roy, Christian Thomas, PaulUnger, Doug Weckstein, Marie WoodCONTENTSWelcome. 2Agenda. 3Research Funding Opportunities. 6Abstract Table of Contents. 7Annual Meeting Abstracts. 10Member Practices. 37Conference Center Map. 38Corporate Members. 402
NNECOS 2017 Palliative Care SymposiumFRIDAY, OCTOBER 27, 20177:30 AM REGISTRATION CHECK INGallery7:30 AM - 8:30 AM CONTINENTALBREAKFAST / COFFEE / EXHIBITSAtrium8:00 AM - 8:45 AM IntegratingOncology and Palliative Care:Lessons Learned - Stowe RoomMarie Bakitas, DNSc, APRN, AOCN,ACHPN, FAAN - University of Alabama atBirmingham8:55 AM - 9:45 AMDistress Due to PrognosticUncertainty, Prognosis Talk, andQuality of Life in Palliative CareConsultations - Stowe Room10:15 AM - 11:00 AMUnderstanding and ManagingPrognostic Uncertainty in CancerCare - Pinnacle B/CPaul K. J. Han, MD, MA, MPH - MaineMedical Center11:10 AM - 12:00 PM Panel DiscussionModerator: Diana Barnard, MD- University of Vermont Medical Center Marie Bakitas, DNSc, APRN,AOCN, ACHPN, FAAN - University of Alabama at BirminghamRobert E. Gramling, MD - Universityof Vermont Medical CenterPaul K. J. Han, MD, MA, MPH- Maine Medical CenterRobert E. Gramling, MD, DSc -12:00 PM LUNCHUniversity of Vermont Medical CenterStowe Room & Beatrice9:45 AM - 10:15AM REFRESHMENTBREAK / EXHIBITS / NETWORKINGAtrium / Collins ReceptionAtrium / Collins ReceptionEXHIBITS/NETWORKING/DESSERTNNECOS 2017 Annual MeetingFRIDAY, OCTOBER 27, 201711:00 AM - 5:30 PMREGISTRATION CHECK IN - GalleryPanel Moderator:12:50 PM WELCOME - Pinnacle B/CDartmouth-Hitchcock Medical Center1:00 - 2:10 PMA Cancer Survivor’s Story: MyJourney to Becoming an Oncologist Dia Draper, MS - Dartmouth Kathleen McBeth, Psy/MAElizabeth B. McGrath DNP, APRN,AGACNP-BC, AOCNP, ACHPN -Panelists:Pinnacle B/CTrevor Bayliss, MD - Berkshire HealthSystem College, Tuck School of Business- University of Vermont MedicalCenterCarissa Morton RN, BSN, BMTCN- Dartmouth-Hitchcock MedicalCenter3
NNECOS 2017 Annual MeetingFRIDAY, OCTOBER 27, 20172:40 - 3:20 PM Intervening on theFinancial Toxicity of Cancer CarePinnacle B/CYousuf Zafar, MD - Duke Cancer InstituteCONCURRENT SESSIONS3:20 - 4:20 PM Financial ToxicityPanel - Pinnacle B/CYousuf Zafar, MD - Duke Cancer InstituteLauren Neves, JD - PhRMADavid Debono, MD - AnthemTorrie Lavoie - New England Cancer Specialists3:30 - 4:20 PM PalliativeRadiotherapy: Old Lessons &Current Controversies - Stowe RoomNirav Kapadia, MD, MS - DartmouthHitchcock Medical Center4:20 - 4:50 PM REFRESHMENTBREAK / EXHIBITS / NETWORKING5:00 PM - 5:50 PM ELAINETOWLE LECTURE: AchievingValue in Oncology: A Brave NewWorld - Stowe RoomBlase Polite, MD - University of Chicago6:00 PM - 6:55 PM ABSTRACTPOSTER SESSION & COCKTAILRECEPTIONPinnacle A & Collins Reception7:00 PM DINNER PROGRAMPinnacle B/CSTEVEN M. GRUNBERGMEMORIAL KEYNOTE:Developing Innovative TherapyLawrence Einhorn, MD - IndianaUniversityAtrium / Collins Reception9:00 PMANNUAL BUSINESS MEETING OF MEMBERSHIP(Immediately following Grunberg Keynote)Pinnacle B/C1.2.3.4.5.6.4Call to Order - Dr. HillElection Results - Dr. UngerMembership Update - Dr. ThomasFinancial Update - Dr. UngerOther Business - Dr. HillAdjourn
NNECOS 2017 Annual MeetingSATURDAY, OCTOBER 28, 20177:15 AM REGISTRATION CHECK-INGallery7:30 AM BREAKFAST/EXHIBITS/NETWORKING - Grand BallroomSPECIAL INTEREST BREAKFASTS Platinum Roundtable - 6:30 AM 10:20 - 10:50 AM EXHIBITS /REFRESHMENTS / NETWORKINGAtrium / Collins Reception10:50 AM - 11:40 AMCONCURRENT SESSIONS Cancer Immunotherapy ToxicityStowe RoomFrederick R. Aronson, MD - NewStowe Room - by InvitationFellows Breakfast - 7:00 AMMansfield Roomall fellows/trainees welcomeNAHPAC Breakfast - 7:15 AMStuart Roominterested allied healthprofessionals welcome8:30 AM - 9:20 AM KEYNOTEA Paradigm Shift: Melanoma Leadingthe Way to the ImmunotherapyRevolution -Pinnacle B/CMarc Ernstoff, MD - Roswell ParkCancer Institute9:30 AM CONCURRENT SESSIONSCAR T Cell Therapy for CancerStowe RoomCharles L. Sentman, PhD - Geisel Schoolof Medicine at DartmouthNavigation in Cancer Care PanelPinnacle B/CModerator - Nicole Messier RN, BSN,OCN,ONN-CG - University of VermontMedical CenterPanelistsKatie Hall, BSN, RN-BC, OCN - Lahey atParklandCharlene Forcier, RN, MS, CHPN,ONN-CG - Dartmouth-HitchcockPatti-Ann Douglas, RN, OCN - Stephen'sMemorial HospitalEngland Cancer Specialists Cardiovascular Disease inCancer Survivors - Pinnacle B/CSanjeev Francis, MD - Maine MedicalCenter11:45 AM - 12:45 PMChallenges in ImmunotherapyPanel - Pinnacle B/CModerator - John Hill, MD - DHMCMarc Ernstoff, MD - Roswell ParkFrederick R. Aronson, MD - NECSCharles L. Sentman, PhD - Dartmouth12:45 PM LUNCH / AWARDS /PLENARY SESSION - Pinnacle B/C1:15PM - 2:15PM AbstractPodium Presentations - Pinnacle B/CModerator - Ken Meehan, MD - DHMCRaphael A. Lizcano III, MD Dartmouth-Hitchcock Medical CenterSundis Mahmood, DO - DartmouthHitchcock Medical CenterHyunsoo Joshua No, BS, CMD - TheUniversity of Vermont Larner College ofMedicine2:15 PM MEETING CONCLUDES5
Collaborative researCh Funding opportunitiesSince the program’s inception in 2008, the NNECOS ResearchFunding Program has awarded more than 135,000 to worthyprojects of value to the Northern New England region.nnecos.org/researchCall for Proposalsforinfo morennecos rmation:.org/researchThe Northern New England Clinical Oncology SocietySuBmiSis seeking research funding proposals for investigativedeadli SionJune 1sneS:projects of value to the entire Northern New EnglandDec. 15t andthcommunity of cancer care providers. The society seeks toaward one or more research grants to worthy proposals, upto a total of 20,000 per application cycle. Eligible candidates will be a currentNNECOS member in good standing. Projects should be in alignment with thesociety’s mission to assure access to high quality oncology care in our region.Preference will be given to projects promoting collaboration amongst NNECOSinstitutions (academic and community). Fellows and others are stronglyencouraged to apply.BudgetPlease note NNECOS is unable to fund indirect costs or investigator salaries aspart of the grant budget. Funds for services of collaborating facility employeesrequired in the operations of a project (i.e. research coordinator, statistician, etc.)will be considered, but should not exceed national averages for their role.Awardees will be notified within 45 days of the submission deadline, be requiredto submit progress reports to NNECOS, and may be asked to present a finalreport of the research to the NNECOS annual meeting.Completed applications must be received through online submission no laterthan 11:00 pm on December 15th or June 1st.paSt projectS funded include: Clinical Trial Barrier Study Exercise for Individuals withStage IV Cancer Head and Neck Cancer TrialInvolving Response to NeoadjuvantChemotherapy Inhibition of Stem Cell Pathwaysin a Patient-Derived GBM TumorModel System. Coagulation Activation in BrainNeoplasms DNA Repair Landscape in Individualswith Increased Risk of Breast Cancer Social Media Usage Within the CancerCommunity of Northern New England66 Thrombin Generation as aPredictive Biomarker for VenousThromboembolism in Patientswith Pancreatic and Lung CancerUndergoing Chemotherapy Synergistic Targeting of CLL Cellswith DNA Repair and B CellReceptor Inhibitors Pilot Study of the Role of MDSCsand VISTA in Immunology of ChronicGraft-Versus-Host Disease FollowingReduced Intensity Allogeneic BoneMarrow Transplantation Pilot Study Involving ActiveSurveillance with CT Imaging andLiquid Biopsy for Inoperable Stage 1ALung Cancer in the Elderlynnecos.org/student-researchCall forProposals:Student-LedResearchProjects 2,500 in fundingavailaBle perapproved project,up to a total of 7,500 annually!NNECOS is also seekingStudent-Led fundingproposals for projectsof value to the entireNorthern New Englandcommunity of cancercare providers and cancersurvivors. The societyseeks to award one ormore project grants toworthy proposals, upto a total of 2,500 perproject.new!applications reviewedon a rolling basis!
NNECOS 2017 Annual Meeting Abstracts: Volume 12Table of ContentsThrombin Generation as a Predictive Biomarker for Venous Thromboembolism inPatients with Pancreatic and Lung Cancer Undergoing Systemic TherapyA. Ajala, M. Cho, L. Salvatore et. al. 10Food Insecurity at New England Cancer Specialists: An Exploratory StudyR. Ali, T. Weisberg. 10The Maine Cancer Genomics Initiative (MCGI): Launching a Community GenomicMedicine Programin Community Practice in MaineA. Antov, P. Helbig, J. Bourne, et al. 11Precision Medicine: The challenges and successes of molecular profiling atDartmouth-Hitchcock Medical CenterM. Chamberlin, E. Bernhardt, et. al. 12Use of a validated survey instrument to assess functional outcomes of rectalcancer treatment in a community hospital settingK. Cole, K. Lehman, and D. DiCesare. 13Relapse of follicular lymphoma: a bevy of buttock cellsC. Del Prete, J.H. Feng, et. 13Is Brain MRI necessary in the pretreatment evaluation of early stage NSCLC?C. Del Prete, G. Wasp, J. Farrelll, et al. 14H3 K27M-mutated gliomas in adults: is there a potential role for immunotherapy?V. Forbes, S. Coker, and P. Rauschkolb. 15Dual-Tandem Brachytherapy for Stage I Endometrial CancerH. Gagne, D. Arsanious, T. Ashikaga . 15Scheduling to ALL Infusion LimitsM. Howe, M. Brown, G. Brooks, et. al. 16Pancytopenia and hemolysisW. Jehangir, E. Umyarova, H. Tul Rehman. 17A Case of Metastatic Dedifferentiated ChordomaS. Kodali, K. Victoria and E. Tipirneni. 17Haploidentical Stem-Cell Transplant for Hematologic Malignancies: Rationale andEarly Experience from a Single, Rural-Based Transplant Center*R. Lizcano, D. McKenna, C. Lowrey, et. al. 187
Cancer patients with self-identified food insecurity report a higher symptomburden than food secure patientsE. Longnecker, T. Weisberg, C. Thomas. 19Improving Oral chemotherapy adherenceR. Macpherson, and C. Moores. 20Transportation barriers and solutions for Maine cancer patientsP. Madden, A. Sheikh, and J. Charles. 21Sharing HintsK. Magni. 22Analysis of Next Generation Sequencing results for Pathogenic gene mutations*S. Mahmood, J. He, F. De Abreu, et. al. 22Establish Validation of CIPN Pretreatment Screening using TNSr, NCI-CommonToxicity Criteria V.3 and EORTC-20 prior to neurotoxic chemotherapyE. McGrath, L. Ronan, and L. Teulings. 23Radioactive seed versus wire guided localization in breast lumpectomy: analysis ofpathologic factors and adequacy of excisionA. Meader, W. Jones, P. Teller, and M. Jones. 24Influence of patient navigators on care coordination within an institutional Lynchsyndrome screening programS. Miesfeldt, W. G. Feero, et. al. 24Drug-Anticoagulant Interactions in Cancer Patients at High Risk for VenousThromboembolism Initiating Outpatient ChemotherapyH. Ng, B. Rogala, J. Schwartz, et. al. 25Effect of Tumor Volume Doubling Time (VDT) on Prognosis for Stage I Non-SmallCell Lung Cancer: An Update*H. J. No, D. Seward, T. Ashikaga, et. al. 26Enhancing Bone Marrow Transplant Care through the Patient ExperienceA. Prokopik, L. Wesigner, et. al. 27Lynch associated adrenocortical tumor with a rare MSH6 pathogenic variantB. Pulluri, W. McKinnon, et. al. 28The Nurses’ Self-Efficacy ProjectJ. Pushee, J. Coffey, and E. McGrath. 28Development of a supportive care intervention for caregivers of patientsundergoing hematopoietic stem cell transplantation: The Ready to CARE programL. Root, L. Blodgett, et. al. 29Potential herb-chemotherapy or radiation interactions in patients with cancer:8
A prospective study of the pharmacist and student-pharmacist run herbalassessment service at the University of Vermont (UVM) Cancer CenterJ. Schwartz and A. Tran. 30Incidence of Potential Germline Mutations in Cancer Patients with Genomic TestingP. Sharma,H. Wright, et. al. 30Targeting CLL and MCL cells with DNA repair and B cell receptor inhibitorsL. Shopland, A. Curtis, et. al. 31Thrombotic Thrombocytopenic Purpura Associated with PazopanibU. Syed, D. Douce, and J. Sprague. 32Concurrent Trimethoprim-Sulfamethoxazole Induced Immune Hemolytic Anemiaand Thrombocytopenia Following Allogeneic Stem Cell TransplantE. Tsui, A. Gero, et. al. 32Evaluation of Kindred Connections cancer survivor peer support programA. Verbyla, J. Chu, et. al. 33Acute Heart Failure due to Autoimmune Myocarditis from PembrolizumabS. Waldstein, S. Kodali, and M. Barry. 34Clinical Utility of PET/CT in Non-Small Cell Lung CancerG. Wasp, C. Del Prete, et. al. 34Venous Thromboembolism (VTE) Increases the Healthcare Burden in Patients withMalignant Glioma (MG)H. Wright, D. Douce, et. al. 35Skeletal Muscle Metastases Masquerading as Micro-abscessesH. Wright, S. Kodali, F. Kahn and K. Butnor. 36* Indicates abstract selected for podium presentation.NNECOS 2017 Annual Meeting AbstractsThe Northern New England Clinical Oncology Society (NNECOS) ispleased to present the following abstracts from across the regionand beyond in this our eleventh year of the abstract program. Theseabstracts have been reviewed by the NNECOS abstract committeeand approved by the NNECOS Board of Directors for presentationat this year’s meeting. Thanks to all who took the time to shareinformation and ideas with colleagues through this means. We’ll lookforward to another group of abstracts for presentation at our 2018Annual Meeting.9
Thrombin Generation as a Predictive Biomarkerfor Venous Thromboembolism in Patients withPancreatic and Lung Cancer Undergoing SystemicTherapyA. Ajala, M. Cho, L. Salvatore, D. Ornstein, M. DrescherDartmouth Hitchcock Medical CenterBackground: The Khorana score (KS) predicts the risk for chemotherapy-associatedVTE, but is assessed only at one time prior to treatment. The aim of our study wasto determine if assessment of TG (both peak TG and endogenous thrombin potential(ETP)) improves VTE risk prediction compared to the KS alone and to evaluate theimpact of systemic therapy on TG over time.Methods: We enrolled 15 adults with newly diagnosed lung or pancreatic cancer. KSwas calculated once. TG blood samples were obtained at the beginning of each of thethree chemotherapy cycles.Results: TG were 341, 324, 641 and 890 nmole, and mean ETP were 1459, 1685, 2155,2051 nmole/min for KS 1,2,3 and 4, respectively. Both peak TG and ETP decreasedover time after cancer therapy. VTE occurred 27%, and the median KS was 2 forpatients with and without VTE. Mean peak TG was similar in patients with and withoutVTE but mean ETP was higher in patients with VTE.Conclusions: Preliminary results suggest that there is a direct correlation betweenKS and peak TG and ETP, and that ETP may be a more reliable predictor VTE than KSin cancer patients. Peak TG and ETP decreased after initiation of systemic therapy,suggesting that the degree of coagulation activation is proportional to tumor burden.These data suggest that TG is a promising biomarker of VTE risk.Food Insecurity at New England Cancer Specialists:An Exploratory StudyR. Ali, T. WeisbergUniversity of Southern Maine, New England Cancer SpecialistsBackground: Food insecurity is a state of being without reliable access to a sufficientquantity of affordable and nutritious food. In this study we identified the prevalenceof food insecurity among patients at New England Cancer Specialists. An observationalhypothesis prior to data collection was that an underinsured state would correlatewith more food insecurity.Methods: Over 6 months, 5135 patients were screened for food insecurity usinga validated 3-item screening tool. We performed descriptive statistics to examinepatients’ demographics, health insurance status, cancer diagnosis, and therapy.10
Results: 104 patients screened positive for food insecurity. 61% women and 39%men. Age of patients ranged from 18 to 80 years with the highest percentage ofpatients being age 50-59. 94% of food insecure patients had a primary care physician.97% had healthcare insurance (Mainecare 17%, Medicare with supplemental 39%,Medicare only 6%, and private insurance 34%) with only 3% uninsured. Patients witha solid tumor diagnosis comprised 72% of patients, Leukemia/Lymphoma 12%, benignhematology and other disorders 15%. Patients experienced treatments ranging fromobservation to combined modality therapy.Conclusions: Food insecure patients were more likely insured than uninsured. Onethird of patients had private insurance. Food insecurity was not always associated withaggressive cancers and cancer therapies but was identified in individuals with benignhematology diagnoses. We plan to explore these associations in future studies andattempt to link food insecurity to cancer treatment outcomes.The Maine Cancer Genomics Initiative (MCGI):Launching a Community Genomic Medicine Programin Community Practice in MaineA. Antov1, P. Helbig1, J. Bourne1, R. Male1, H. Reddi1, S. Mockus1, K. Adams1, K. Reed1,E. Edelman1, L. Waterston2, S. Miesfeldt2,P. Han2, J. Rueter1The Jackson Laboratory, 2Center for Outcomes Research and Evaluation (CORE) atMaine Medical Center Research InstituteBackground: Sophisticated NGS-based genomic tests interrogating a large number ofgenetic alterations in tumor tissue have recently been developed but many barriersexist in the integration of these methodologies into community practice. The MCGI,a partnership between JAX and the largely rural Maine oncology community, wasestablished to facilitate the integration of novel genomic technologies into communityoncology practice.1Methods: MCGI goals are enabled by network and governance creation, the provisionof educational opportunities to clinicians and genomic tumor board support as wellas the conduct of a prospective, multi-site study protocol investigating clinician andpatient experience with clinical genomic tumor testing.Results: The MCGI Forum, an initial meeting of clinicians and research staff from theMaine oncology community, was held in Feb 2017. It was attended by 23 cliniciansand 27 research and administrative staff from 16 practices. In May 2017, the Studyprotocol received IRB approval, allowing sites and clinicians to enroll. To date, 3practices have enrolled as sites and 1 practice will refer patients to the central siteat the MCGI office for study participation. Subjects participating to date include 16clinicians and 7 cancer patients. The initial educational module and MCGI-supportedgenomic tumor boards have been launched.11
Conclusions: The Maine Cancer Genomics Initiative is an opportunity for bothtranslational implementation and research by the Maine oncology community.Onboarding and enrollment of sites and clinicians on the study has proceeded swiftly,indicating the potential for additional translational outreach opportunities in otherhealthcare systems and geographic areas.Precision Medicine: The challenges and successes ofmolecular profiling at Dartmouth-Hitchcock MedicalCenterM. Chamberlin1, Erica Bernhardt1, A. Ajala1, D. Findley2, G. Tsongalis2, I. Gorlov2, T.Miller2, L. Tafe2Dartmouth Hitchcock Medical Center1; Geisel School of Medicine at Dartmouth2Background: Dartmouth has been performing next generation sequencing (NGS) ontumor specimens since 2013. The Molecular Tumor Board (MTB) was formed in 2013to assist clinicians in interpreting the results and identifying potential treatments.Clinical triais are increasingly requiring mutation information. We describe theevolution of our molecular oncology program since 2014 and the efficacy of differentdata collection methods.Methods: Data from our clinical trial, MTB, EMR and molecular pathology databaseswere reviewed between 2014 and 2017. A searchable molecular tumor board notewas created to extract data from the electronic medical record and compare tomanually entered dataResults: Results:50 gene panels peryear:Fusion panels peryear:Clinical trialsrequiring mutationdata per year:Enrollments peryear:Reimbursements( ):20142015201630962110652017 (through6/1/17)4560014910641635260411TBA00 617.84/case 617.84/ caseManual DataEMR Data ToolMTB casesClinical trialssuggested95137138% captured bydata tool75%292%EnrolledOff‐label druguse : Molecular profiling is increasingly required for clinical trial enrollment however less than
Conclusions: Molecular profiling is increasingly required for clinical trial enrollmenthowever less than 10% of patients are enrolling on molecularly based trials and lessthan 5% are presented at a Molecular Tumor Board. A data extraction tool did notcapture clinical data reliably. Improvements in data collection systems are essential toevaluate the outcomes of multi-disciplinary programs. A quality improvement projectis underway.Use of a validated survey instrument to assessfunctional outcomes of rectal cancer treatment in acommunity hospital settingK. Cole1, K. Lehmann1, D. DiCesare2Portland Surgical Associates, 2 Tufts University School of Medicine1Background: Patients undergoing rectal cancer treatment may develop bowel, urinary,and sexual functional difficulties weeks to months after treatment; screening for theseissues can be challenging in the absence of a centralized, multi-disciplinary clinic. Weused a validated survey tool to help identify these patients.Methods: Surveys were offered postoperatively to all patients undergoing rectalresection with pelvic dissection between February 2012 and July 2017. The survey wasmodified from the EORTC (QLQ-CR29) validated questionnaire. A response of 3 (“quitea bit”) or more on any survey item prompted consideration for interventionResults: During the study period, 32 patients were surveyed. 21 patients returned atleast one survey (66%); 29 out of 51 total surveys (57%) were returned. 12 of the 29surveys (41%) were completed during a follow-up visit, while 17 (59%) were returnedby mail. During the study period, 9 out of 21 patients (43%) assigned a score of 3 atleast once for a bowel function item; 4 out of 21 patients (19%) for a urinary functionitem; and 7 out of 21 (33%) for a sexual function item. A total of 12 out of 21 patientsto return a survey (57%) were offered interventions and 5 out of 12 accepted (42%)Conclusions: Use of an existing survey instrument allowed us to identify and treat patientswith functional problems related to rectal cancer treatment independent of scheduledfollow-up, improving the quality of survivorship care in our community hospital.Relapse of follicular lymphoma: a bevy of buttock cellsC. Del Prete, J. H. Feng, F. Lansigan, E. Bengtson, R. KubicaDartmouth-Hitchcock Medical CenterBackground: Follicular lymphoma (FL) is considered an indolent non-Hodgkinlymphoma, rarely associated with a leukemic phase. We report a 58-year-old malewith history of FL, diagnosed two years prior with extensive adenopathy and treatedwith bendamustine and rituximab. Therapy was discontinued after two cycles due13
to intolerance. He achieved partial remission and was followed prospectively. Hepresented with debilitating lower extremity swelling. Dopplers were negative for DVTthough extensive pelvic adenopathy was detected. Labs showed a critical white countand tumor lysis. He was admitted to the hematology service.Methods: Case reportResults: Labs revealed WBC 463K (9K two months previously), Hgb 7.3, Plt 63K andLDH 740 (110-220 u/L). The differential diagnosis at this time included histologictransformation to more aggressive lymphoma such as diffuse large B-cell vs CLL/SLL. Aperipheral smear revealed leukocytosis with 91% atypical lymphocytes, described as“buttock cells”, consistent with leukemic phase of FL. Flow cytometry demonstrateda monoclonal lambda-restricted CD10 CD20 B-cell population. A PET-CT showedextensive FDG avid bulky adenopathy in the neck, chest, abdomen, and pelvis alongwith massive splenomegaly. A lymph node biopsy revealed FL with Ki67 of 10-20% anda bone marrow biopsy showed 95% involvement with FL. The patient was treated withCOPE (cyclophosphamide, vincristine, prednisone, and etoposide) and rituximab wasadded once WBC 50K. Therapy is ongoing with dramatic response to date.Conclusions: Our patient was admitted with suspicion of transformation to highgrade lymphoma; however, subsequent work-up revealed leukemic phase of follicularlymphoma, a rarely reported entity associated with a poor prognosis.Is Brain MRI necessary in the pretreatmentevaluation of early stage NSCLC?C. Del Prete, G. Wasp, J. Farrell, K. Dragnev, G. Russo, G. Atkins, G. BrooksDartmouth-Hitchcock Medical CenterBackground: At present, there is limited evidence and conflicting guidelines on whento include brain MRI in the pretreatment evaluation of NSCLC.Methods: We retrospectively reviewed data from eligible patients who underwentwork-up for newly diagnosed NSCLC from January 1 to December 31, 2015. Weidentified all records of pretreatment neuroimaging within 12 weeks of diagnosis,inclusive of CT head (CR) or brain MRI (MRI). The indication for neuroimaging,presence of neurologic symptoms, cancer stage (excluding neuroimaging), and thepresence of brain metastases were abstracted.Results: 157 of 216 patients (72.7%) underwent neuroimaging (144 MRIs, 13 CTs).Only 41 patients (26%) underwent imaging for neurologic symptoms while theremainder were asymptomatic (74%). Of those, 28 (68%) were found to have abrain metastasis. Among asymptomatic patients, 19 were stage I and 16 were stageII prior to neuroimaging. No brain metastases were discovered. For more advancedNSCLC (also asymptomatic), 37 patients had stage III and 44 stage IV disease: brainmetastases were found in 4 (11%) and
Moderator - Nicole Messier RN, BSN, OCN,ONN-CG -University of Vermont Medical Center Panelists Katie Hall, BSN, RN-BC, OCN - Lahey at Parkland Charlene Forcier, RN, MS, CHPN, ONN-CG - Dartmouth-Hitchcock Patti-Ann Douglas, RN, OCN - Stephen's Memorial Hospital 10:20 - 10:50 AM EXHIBITS / REFRESHMENTS / NETWORKING Atrium / Collins Reception