Transcription
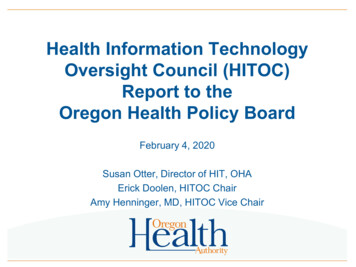
Health Information TechnologyOversight Council (HITOC)Report to theOregon Health Policy BoardFebruary 4, 2020Susan Otter, Director of HIT, OHAErick Doolen, HITOC ChairAmy Henninger, MD, HITOC Vice Chair
Items for today 2Brief background on HITOC and 2019 ProgressHITOC Strategic Plan Update ProcessHITOC Recommended 2020 WorkplanHITOC Membership Changes – Recommended SlateRequest OHPB Action
Brief Background onHITOC and 2019 Progress3
Oregon’s Health IT Strategic Plan OHA is transforming the health care system; the core ofthose efforts is the coordinated care model The coordinated care model relies on health IT tosucceed Coordinating health IT efforts at the state level isimportant because there are so many moving parts HITOC is charged with creating a statewide strategicplan for health IT in Oregon4
How does health IT support thecoordinated care model?Health IT helps Consumers/patients,their families, andtheir caregiversGet access to their own health information and participatein their careProvidersSecurely gather, store, and share patients’ clinical data sothe care team can work together to provide careProvidersTrack and report on quality measures, which supportefforts to hold the health care system accountable fordelivering high-quality careAnalyze data to identify disparities and identify patientswho need more care to allow targeted efforts to improvehealthCCOs, health plans,and providers5
OHPB’s Responsibilities Re: HITOC 6Charter HITOCSet HITOC’s prioritiesAppoint HITOC’s members and decide length of termsConsider HITOC’s recommendations and take actionwhen appropriate
HITOC’s ResponsibilitiesThe Oregon Legislature created HITOC to ensure healthsystem transformation efforts are supported by HIT.HITOC’s responsibilities under the law/charter are to: 7Explore HIT policyPlan Oregon’s HIT strategyOversee OHA’s HIT effortsAssess Oregon’s HIT landscapeReport on Oregon’s HIT progressMonitor Federal HIT law and policy
Vision/Goals for HIT-Optimized Health Care8
Policy Priorities and HITOC’s GoalsHealth System TransformationPolicy Priority*Increase access to health careEnhance care coordinationChildren’s HealthHealth IT Goal/AreaGoal 1: Share patient information across the careteamGoal 3: Patients can access their own information andengage in their careCost ContainmentPay for outcomes and valueGoal 2: Use data for system improvementMeasure progressImprove health equityShift focus upstream; Address thesocial determinants of health9Emerging area: Health IT supports social determinantsof health and health equity*From OHPB’s Action Plan for Health and workplan; italics represent 2019 OHPBPriority areas
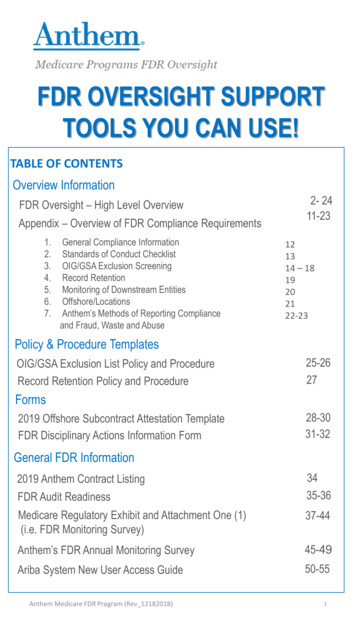
HITOC’s 2019 ProgressHITOC RoleExplore HIT PolicyAreasPlan HIT StrategyOversee OHA’s HITEfforts SDOH and health IT; HIT Commons: Community Information Exchange Health Equity Definition and health IT Health IT and patient engagement Behavioral health HIT workplan 2021 Strategic Plan Update - planningLaunched in 2019: Clinical Quality Metrics Registry HIE Onboarding Program Oregon Provider Directory CCO 2.0 HIT Roadmaps Major work in HIT Data reporting on EHR and HIE progress HIT Commons: Community Information Exchange Environmental ScanMonitor FederalPolicy Federal proposed interoperability rules; Trusted Exchange FrameworkHITOC Membership Oriented new members, who significantly increased HITOC’s consumerrepresentation and diversity Updated HITOC bylaws to allow for leadership developmentAssess HITLandscape, Reporton Progress102019 HITOC Work
Health IT Progress: Key Areas Providers are using electronic health records (EHRs orEMRs) at high rates overall Health information exchange options have grownsignificantly Health IT supports value-based payment Health IT can help address social determinants of health11
OREGON EHR ADOPTION IS VERY HIGH OVERALL,BUT DIGITAL DIVIDES EXIST.FEDERAL EHR INCENTIVEPROGRAM PARTICIPATIONRATEEHR ADOPTION RATEHospitals (n 60)100%Patient-CenteredPrimary Care Homes(n 623)Behavioral healthonly agencies(n 208)Oral health clinics 0%Unknown(n 915)100%97%59%76%13%24%Oregon Health Authority - Office of Health Information TechnologyAVERAGE FEDERALINCENTIVE AMOUNT RECEIVED 4,304,522 per hospital(range: 130k- 11.2m) 1,207,942 per org.(range: 8.5k- 27.5m) 234,821 per agency(range: 21k- 1.8m) 190,467 per organization(range: 21.3k- 1.8m)
OREGON EHR ADOPTION IS VERY HIGH OVERALL,BUT DIGITAL DIVIDES EXIST.NUMBER OF DIFFERENTEHR VENDORSHospitals (n 60)10Patient-CenteredPrimary Care Homes(n 623)26Behavioral healthonly agencies(n 208)Oral health clinics(n 915)4913TOP EHR VENDORSEHR VENDORS THAT OFFER2015 CEHRT PRODUCTEpic, 71%CPSI, 7%90%Epic, 52%Centricity, 10%85%Credible, 10%Qualifacts, 9%47%Epic, 28%Dentrix, 25%54%Oregon Health Authority - Office of Health Information Technology
OREGON HIT DATA BRIEF:HEALTH INFORMATION EXCHANGEElectronic health information sharing, or health information exchange (HIE), is central to Oregon’shealth reform objectives of high quality, coordinated care and paying for value instead of volume.Using patient data tocoordinate PHYSICAL,BEHAVIORAL,ORAL health careUsing patient data forpopulationmanagement andvalue-based paymentOregon Health Authority - Office of Health Information TechnologyUsing patient data toaddress the socialdeterminants ofhealth
IN THE PAST 5 YEARS, OREGON HAS SEEN UNPRECEDENTEDGROWTH IN HIE.20142019Emergency Department Information Exchange(EDie) implementation just beginning1Many Oregon organizations have real-time access tohospital and emergency department event notificationsfor their patients from hospitals in Oregon and itsbordering statesPrimary method for moving care summaries isDirect secure messaging or EHR-based tools2Five regional HIEs (one in development) coverabout 40% of Oregon counties; limited servicesavailableMajor hospitals, health systems, and their affiliatedprovider groups have on-demand access to caresummaries for care their patients receive outside theirsystem3Regional HIEs are available in half of Oregon’s countiesand serve an important role in their communitiesVirtually no electronic data sharing amongdifferent provider types, with fax being the primarymethod4Behavioral health and oral health providers are using HIE;they also share important patient information withphysical health providersOregon Health Authority - Office of Health Information Technology
IN THE PAST 5 YEARS, OREGON HAS SEEN UNPRECEDENTEDGROWTH IN HIE.20142019Virtually no connections among disparatenetworksAlthough Oregon’s Prescription DrugMonitoring Program (PDMP) was launchedin 2011, there was no EHR integrationHealth IT for population management is inits infancy; value-based payment is not amajor part of Oregon’s landscape567Providers use multiple HIE networks; some haveconnected to each otherProviders can access opioid prescription datamore easily; providers with health IT integrationaccess it at much higher ratesProviders use clinical data entered, stored, andshared by health IT to better managepopulations and target interventions. This alsosupports the dramatic increase in value-basedpayment arrangements.Oregon Health Authority - Office of Health Information Technology
ADOPTION OF VARIOUS HIE TOOLS IS INCREASING INOREGON.EDIE/PREMANAGEHospitals (n 60) 100%Health Systems (n 14) 100%REGIONAL HIECAREQUALITY100%100%86%72%68%PCPCHs (n 623) 47%Oral health clinics (n 915)16%All behavioral health15%licensed agencies(n 246)201730%22%Hospitals 37%Health Systems 29%PCPCHs 27%Oral health 8%Behavioral health7%20192017Health Systems 50%Hospitals 45%PCPCHs 40%37%30%29%9% Behavioral health 9%9%Oral health 8%2019Oregon Health Authority - Office of Health Information Technology201755%11%9%2019
VISITS DECREASED BY 34% IN THE 90 DAYS FOLLOWING ANINITIAL CARE GUIDELINE CREATION.2,302Total number ofvisits by HighUtilizers in the 90days before a careguideline wasimplemented.Before Care GuidelineCreation1,521Number of visits byHigh Utilizers inthe 90 days after acare guideline wasimplemented.After Care Guideline CreationOregon Health Authority - Office of Health Information Technology
PROVIDERS CAN ACCESS OPIOID PRESCRIPTION DATA MORE EASILY;PROVIDERS WITH HEALTH IT INTEGRATION ACCESS IT AT MUCH HIGHER RATES.PDMP enrollment is increasing among top prescribers.15,103 (87%) enrolled160001400012000100008000Prescribers and pharmacists cannow access Prescription DrugMonitoring Program (PDMP)information within their health ITLIVE WITH INTEGRATED PDMP ACCESSTotal PrescribersPrescribers – EDie10,65670060008,228 (54%)viewed reportAll Prescribers(n 17,406)3,833 (96%) enrolled2,997 (78%)viewed reportTop 4,000Prescribers40001,931 (97%) enrolled1,624 (84%)viewed reportPrescribers – EHR andHIEPharmacy Chains9,95672000Pharmacy sites0Top 2,000PrescribersOregon Health Authority - Office of Health Information Technology367
PROVIDERS CAN ACCESS OPIOID PRESCRIPTION DATA MORE EASILY;PROVIDERS WITH HEALTH IT INTEGRATION ACCESS IT AT MUCH HIGHER RATES.900,000OR Integrated867,734Due to their automation, query rates viaintegrated EHRs/HIT have increasedsignificantly.These high rates of automated queriesyield significantly higher rates of dataavailable to providers at the point ofcare.0Jan 18Jan 19Web Portal108,456EDIE 91,568Pharmacy Integrated36,392Sep 19Oregon Health Authority - Office of Health Information Technology22% of prescribers are clicking on andviewing PDMP reports when a queryreturns PDMP data for a patient beingseen. Access to PDMP data at the pointof care supports providers makinginformed prescription decisions forimproved patient outcomes.
OREGON HAS SEEN A DECREASE IN RISKY PRESCRIBING.Rates of co-prescribing and high-dose prescribing have decreased by nearly 50% since2016.1614121086420High Dose Prescribing, 90MED per 1,000 residents2016 Q32016 Q42017 Q12017 Q22017 Q32017 Q42018 Q12018 Q22018 Q32018 Q42019 Q12019 Q22019 Q3Opioid and Benzodiazepine Coprescribing per 1,000 residents2016 Q32016 Q42017 Q12017 Q22017 Q32017 Q42018 Q12018 Q22018 Q32018 Q42019 Q12019 Q22019 Q31614121086420Oregon Health Authority - Office of Health Information Technology
LOOKING AHEAD FOR BEHAVIORAL HEALTH AGENCIESBehavioral health organizations need EHRs that meet their unique information capture andmanagement needs. These EHRs must be interoperable and support behavioral health reportingrequirements, such as electronic metrics reporting.Support needsidentified in theWorkgroup report:Navigating theEHR vendorlandscapeHIT educationShared learningopportunitiesFinancialincentivesOregon Health Authority - Office of Health Information TechnologyEHR marketanalysisSupport fromlarger, betterresourcedorganizations
THE ROAD AHEADHITOC’s strategies must consider HIE gaps and the complex, fluid HIE environment. The high cost of EHRs contributes to lower EHR adoption rates for smaller organizations, so theseorganizations tend to have less access to HIE through nationwide query-based networks. Oregon providers, across the board, typically need multiple HIE tools to meet all their HIE needs. There are limited HIE options available today for complex care coordination. 42 CFR Part 2 remains a barrier to exchange, due to perceptions and the regulation itself. Major changes at the federal level will affect Oregon stakeholders over the next five years.Oregon Health Authority - Office of Health Information Technology
Progress Highlight: HIT Commons HIT Commons is a public/private partnership to govern high priority,statewide HIT Initiatives with OHA as public sponsor. Mission: to accelerate and advance Health Information Technologyadoption and use across the state. Build off Oregon’s history of successful collaboration such asEDie/PreManage. Intended to help connect existing HIT systems, support statewidesolutions. OHA is voting member of Board and provides significant funding viastate and federal funding opportunities.24
HIT CommonsA shared public/private governance partnership to accelerateand advance health information technology in OregonCo-sponsorOregon Health Leadership CouncilEDIE—Emergency Department Information ExchangePDMP – Prescription Drug Monitoring Program25Co-sponsorOregon Health AuthorityHealth Information Technology Council
HIT Commons: Community InformationExchange Oregon health system transformation to addresssocial determinants of health (SDOH):– Oregon Health Policy Board focus– CCO 2.0 SDOH requirements– HB 3076 Community Benefit (SDOH floor for hospital/clinicspend)– HIT Oversight Council’s strategic planning work Oregon health systems and communities starting toinvest in SDOH infrastructure Collaborative work could ensure that efforts are pooledand standardized to accelerate progress, reducevariation and improve effectiveness26
Working Definition:Oregon Community Information Exchange (CIE) A CIE connects health care, humanand social services partners toimprove the health and well-being ofcommunities and address healthdisparities and health equityA bi-directional CIE TechnologyPlatform could provide manyfunctions, including statewide socialservices directory, shared riskassessment capabilities, real-timeclosed loop referral management,collaborative care coordination, andstandardized metrics, and dataanalysis.Bi-DirectionalInformation ExchangeSocial NeedsScreeningRiskAssessment,Analytics,and MetricsCommunityInformation ExchangeResourceDirectoryCollaborative CarePlansNote: this is a working definition in a rapidly evolving space.27ReferralManagement
Environmental Scan Reveals MultiplePlayers Active in IE-Environmental-Scan-August-31-2019.pdf28
Aligning CIE Streams of Work HIT Commons: Oregon CIE Advisory Group– Developing a Statewide CIE Roadmap by end of 2020 Oregon Health Leadership Council (OHLC)– Working in partnership with early adopters to develop acoordinated CIE implementation with Unite Us (vendor) OHA’s Office of Health IT– Convening an internal OHA/Dept of Human Services CIEworkgroup HITOC– Strategic Plan Update – stakeholder input29
CIE Advisory Group: Key TopicsSocial needs screeners/assessmentsResource directoriesCommunity & Community Based Organization (CBO)engagement strategiesPrivacy & legal agreement structure or best practicesMetrics, reporting, evaluationWorkflows & learning collaboratives30
Recommended HITOC Prioritiesfor 2020 and Strategic Plan UpdateProcess31
Proposed 2020 Major HITOC Priorities Strategic Plan Update, Stakeholder Engagement– Health information exchange, system improvement/value-basedpayment, patient engagement– Emerging area: social determinants of health and CommunityInformation Exchange– Emerging area: health IT and health equity Landscape/policy work– Exploratory work with Public Health and health IT– CCO 2.0 Health IT Roadmaps, EHR/HIE data Federal rule/policy changes and sustainability Oversight work: partnerships and programs– Behavioral health HIT Workplan32
Exploring Social Determinants of Healthand HIT HIT is critical to OHA’s SDOH work––––To assess an individual’s SDOH needsTo coordinate care between providers and SDOH organizationsTo manage referrals for addressing SDOHTo use SDOH data for risk modeling, population management 2020 HITOC work:– Support for HIT Commons Community Information Exchangeefforts– Stakeholder input and Strategic Plan work33
Exploring Health Equity and HIT HITOC’s work includes:––––Input and reflection on Health equity definitionCoordination with Health Equity CommitteeUnderstanding how EHRs standards match to REAL-DClinical Quality Metrics Registry future capacity to track patientlevel data– Oregon Provider Directory captures demographic information– Further exploration of connection between health IT and healthequity34
Strategic Plan Update: HIT to supportHealth System TransformationHealth System TransformationPolicy Priority*Increase access to health careEnhance care coordinationChildren’s HealthHealth IT Goal/AreaGoal 1: Share patient information across the careteamGoal 3: Patients can access their own information andengage in their careCost ContainmentPay for outcomes and valueGoal 2: Use data for system improvementMeasure progressImprove health equityShift focus upstream; Address thesocial determinants of healthEmerging area: Health IT supports social determinantsof health and health equity*From OHPB’s Action Plan for Health and workplan; italics represent 2019 OHPBPriority areas35
Strategic Plan Update: Centered on GoalsHealth IT Goal/AreaDescriptionGoal 1: Share Patient Information Oregonians have their core health information availableAcross the Care Teamwhere needed so their care team can deliver personcentered, coordinated care.Goal 2: Use Data for SystemImprovementClinical and administrative data are efficiently collectedand used to support quality improvement and populationhealth management, and incentivize improved healthoutcomes. Aggregated data and metrics are also used bypolicymakers and others to monitor performance andinform policy development.Goal 3: Patients Can Access Their Individuals and their families access, use and contributeOwn Health Information andtheir clinical information to understand and improve theirCollaborate in Their Carehealth and collaborate with their providersEmerging Area: Health ITsupports social determinants ofhealth and health equity36
Strategic Plan Update: Process Join a listening session in person or by phone. Register atgo.usa.gov/xpzy2. Submit a written comment (Feb. 1 – Apr. 30) atgo.usa.gov/xpzVt Stay up to date at our website go.usa.gov/xpeQc37
Strategic Plan Update: 2020 StakeholderListening sessionsFebruary: Technology Partner Listening Session Tribal/OHA Monthly Meeting Oral Health Listening SessionMarch: CCO Listening Session Consumer Listening Session HIT Commons Governance Board Meeting Community Information Exchange Advisory Group MeetingApril: Behavioral Health Listening Session General Listening Session38
OHPB ACTION: 2020 HITOC PrioritiesAction: Are these the right priorities for HITOC in 2020? Strategic Plan Update, Stakeholder Engagement– Health information exchange, system improvement/value-basedpayment, patient engagement– Emerging area: social determinants of health and CommunityInformation Exchange– Emerging area: health IT and health equity Landscape/policy work– Exploratory work with Public Health and health IT– CCO 2.0 Health IT Roadmaps, EHR/HIE data Federal rule/policy changes and sustainability Oversight work: partnerships and programs– Behavioral health HIT Workplan39
HITOC Membership – ProposedChanges40
Learn more about Oregon’s HIT/HIE developments andSubscribe to our email a/HPA/OHIT-HITOCSusan OtterDirector of Health Information TechnologySusan.Otter@state.or.us41
Health Information Technology Oversight CouncilSupplemental Materials for Report to Oregon HealthPolicy Board, February 4, 2020Supplemental Materials 2020 Health Information Technology Oversight Council (HITOC) Draft Work Plan (p. 2) HITOC Key Strategies Summary: 2017, 2019, 2021 (p.3-4) 2021 HITOC Strategic Plan Update – 2020 process and Current Goals/Strategies (p.5-8) HITOC Membership – Proposed Changes (separate attachment)Reference materials: 2019 HITOC Data Report, HIE Overview, HIE in Oregon: Tale of Two 2019HITReport HIEOverview TwoWorlds Combined.pdf HIT Commons: Community Information Exchange – Environmental Scan and CIE AdvisoryGroup: mmunity-informationexchange-ocie/Other background materials: Oregon HIT Programs and Partnerships OC/Documents/101 Office of Health IT.pdf HITOC Overview: https://bit.ly/2Wfxeh2 HIT Roles: HITOC, HIT Commons, OHA, OHPB: /Health IT Roles OHBP-OHA-HITOC-HITCommons.pdf HITOC Behavioral Health HIT Workgroup Report and Scan (Resources section of webpage):https://bit.ly/2DuRyUl Oregon’s Strategic Plan for Health Information Technology (HIT) and Health InformationExchange (2017-2020): https://bit.ly/2CsrDerGet involved with Oregon Health ITOffice of Health Information Technology: HealthIT.Oregon.govJoin the listserve: bit.ly/2VYgoDBHITOC Report to OHPB: Supplemental Materials (January 2020)Page 1 of 8
Health Information Technology Oversight CouncilSupplemental Materials for Report to Oregon HealthPolicy Board, February 4, 2020HITOC 2020 Draft Work Plan AreasStrategic work: 2021 Strategic Plan Update and stakeholder/partner engagementNext steps for Health equity and health ITNext steps for Patient engagement through health ITEvolution of Health Information Exchange: Networks of networks effortsPotential OHPB Priority Topics (e.g., Cost Growth Target)Exploratory and Policy Context Exploratory work: Public health and health ITImpacts of the new federal interoperability rules, Trusted Exchange Framework and CommonAgreement (TEFCA)Changing health IT funding: Sustainability for HIT workLandscape assessment: CCO 2.0 Health IT Roadmaps and EHR/HIE DataOversight Continued oversight of current health IT programs/partnerships and Behavioral Health HITworkplan*Full HITOC 2020 Draft Workplan: s/2020HITOCWorkPlan Draft.pdfHITOC 2019 Major Bodies of Work Exploratory work in social determinants of health and Community Information Exchangeconcept Preliminary work in health equity (definition and the role of health IT) Exploratory work in patient engagement and health IT Next steps for statewide health information sharing efforts, including review of proposedfederal policy Wrap up planning for behavioral health and HIT work – adopted BH HIT Workplan Launched several efforts: Clinical Quality Metrics Registry, Oregon Provider Directory, HIEOnboarding Program, CCO 2.0 HIT Roadmaps Major work on 2019 HITOC Data Report on EHR and HIE progress Prepare for HITOC Strategic Plan Update HITOC membership – orientation to new members, updated bylaws re: leadership developmentNote: Ongoing priorities include continued oversight work on partnerships/programsHITOC Report to OHPB: Supplemental Materials (January 2020)Page 2 of 8
Health Information Technology Oversight CouncilSupplemental Materials for Report to Oregon HealthPolicy Board, February 4, 2020Status of HITOC Key Strategies: 2017, 2019, 2021ConceptPlanningOperationalSuspendedStatus in 2017Status: end of 2019Support for Electronic Health Record (EHR) Adoption/UseMedicaid EHR IncentiveOperationalOperationalProgram (MEHRIP)since 2011Oregon MedicaidOperationalEnded May 2019 asMeaningful Use Technicalsince 2016plannedAssistance Program(OMMUTAP)Promote EHR ComparisonConcept – engage OregonTool from Office of thestakeholders in input toNational Coordinator forONCHITImplement Core HIT InfrastructureOregon CommonPlanningSuspended - 2018Credentialing Program(OCCP)Oregon Provider DirectoryPlanningSoft-Launch - Fall 2019(OPD)HIT Commons: adoption& spread support: OPDFlat File Directory forDirect secure messagingaddressesClinical Quality MetricsRegistry (CQMR)ConceptOperationalsince 2014PlanningSpread Health Information Exchange (HIE)CareAccordOperationalsince 2011HIE Onboarding ProgramPlanningOHA’s PreManage Medicaid Launched 2016SubscriptionNetwork of Networks forConceptStatewide HIESupporting OPD softlaunch - 2019-2020OperationalInitial launch for MEHRIP Jan. 2019, Launch for CCOincentives - late 2019EndedStatus by end of 2021Ends 2021 as plannedEngage Oregonstakeholders in planning –2020/2021Promote launch - 2022Ongoing operations,expanded functionality tosupport statewide useOngoing support TBDTransition to OPD - 2020Ongoing operations,expanded functionality(e.g., using enrollmentdata for multi-payer uses)Ended mid-2017Launched - Jan 2019OperationalEnds 2021 as plannedOngoing operationsPlanningHITOC Report to OHPB: Supplemental Materials (January 2020)Page 3 of 8
Health Information Technology Oversight CouncilSupplemental Materials for Report to Oregon HealthPolicy Board, February 4, 2020Status in 2017Expanding Interoperability - Federal 2-yearONC CooperativeHIE grant,Agreement (subrecipient:ended July 2017Reliance)as plannedBehavioral HealthConceptInformation Sharing Toolkit(42 CFR Part 2)Shared Governance and High Value DataHIT CommonsPlanningEmergency Department OperationalInformation Exchangesince 2015(EDie)/PreManagePrescription DrugPlanningMonitoring Program(PDMP) IntegrationinitiativeOregon CommunityInformation Exchange(CIE)Other: Policy and Data workCCO 2.0: HIT RoadmapsCCO 2.0: HIT Data onEHR/HIE use by clinicConceptHITOC Data reporting, data“dashboards”Behavioral Health HIT workPlanningBehavioralHealth HITEnvironmentalScanStatus: end of 2019(on hold awaiting federalTEFCA and rulemaking)Status by end of 2021Finalized - late 2019Ongoing updatesOperational since 2018Operational (under HITCommons since 2018)Ongoing operationsOngoing operationsOperational since 2018Ongoing operationsConceptCIE Roadmap - 2020Implementation of CIERoadmap - 2021Planning - 2018Draft CCO HIT Roadmapssubmitted with RFA – April2019Most CCO 2020 HITRoadmaps approved –Dec. 2019PlanningAll 2020 HIT Roadmapsapproved - spring 2020;Annual Update - spring2021Baseline HIT datareported - fall 2020,Annual Update - spring20212019 HITOC Data report on Ongoing data reportingEHR/HIEBH HIT Workgroup reportOngoing work and BH HIT– 2018,workgroupOHA BH HIT Workplan 2019HITOC Report to OHPB: Supplemental Materials (January 2020)Page 4 of 8
The Oregon Health Authority and Health IT:Strategic Plan 2021 UpdateWhat is Oregon’s strategic plan for health IT?OHA is transforming the health care system, and the core of those efforts is the coordinated care model. Thecoordinated care model relies on health IT to succeed. Coordinating health IT efforts at the state level isimportant because there are so many moving parts. Therefore, the Oregon legislature charged HITOC withcreating a statewide strategic plan for health IT for everyone in Oregon.Health IT helps Consumers/patients, their families, and their caregivers: Access their own health information andparticipate in their careProviders: Securely gather, store, and share patients’ clinical data so the care team can work together toprovide care; track and report on quality measures, which supports efforts to hold the health care systemaccountable for delivering high-quality careCCOs, health plans, and providers: Analyze data to identify disparities and find patients who need morecare to allow targeted efforts to improve healthOregon and Health IT: Quick OrientationProviders are using EHRs/EMRs at high rates overall. Electronic health records or electronic medicalrecords (EHR/EMR) support patient care and patient access to their own information (via patient portals); thedata they gather supports care coordination, value-based payment, and population management.Status: Overall EHR adoption rate is higher than the national average, number of providers using more advancedEHRs is growing, “digital divides” remainHealth information exchange options have grown significantly. HIE securely moves health informationbetween organizations, supporting care coordination, value-based payment, and population management.Status: EDie/PreManage (Collective platform) have been a standout success, national networks provide accessto care summaries, regional HIEs and other efforts support CCOs and communities, no single tool can meet allneeds, “digital divides” remainHealth IT supports value-based payment. CCOs and providers need health IT tools and processes to managevalue-based payment arrangements.Status: CCOs have developed Health IT Roadmaps that include plans for health IT and value-based paymentwhich will support major growth in value-based payment arrangements under CCO 2.0; most CCOs, health plans,and providers will need to develop new health IT capacity to manage value-based paymentHealth IT can help address social determinants of health. Health IT tools can support social needsassessments, risk scoring, and connect health care with social services.Status: Providers are exploring using health IT to assess social needs; work is underway to explore options forcommunity information exchange, connecting health care providers with social services; this area raises newchallenges with technology, privacy, and care coordinationStrategic Plan 2021 Update, last updated January 2020Page 5 of 8
Gathering your input: health IT goals and question promptsHITOC wants to hear your input on what strategies are going well and where Oregon needs to change course.Please look at the health IT goals below and reflect on how things are going. The optional questionprompts below can help you organize your input, but you are not required to use them.Goal 1: Share patient information across the care team. Oregonians have their core healthinformation available where needed, so their care team can deliver person-centered, coordinated care.Goal 2: Use data for system improvement. Clinical and administrative data are efficiently collectedand used to support quality improvement and population health management, incentivize improvedhealth outcomes. Aggregated data and metrics are also used by policymakers and others to monitorperformance and inform policy development.Goal 3: Patients can access their own information and engage in their care. Individuals and theirfamilies access, use, and contribute their clinical information to understand and improve their healthand collaborate with their providers.Emerging area: Health IT supports social determinants of health and health equity.Optional question prompts (all questions can be applied to all goals)1. How is this going for you today?5. Where are the biggest challenges/barr
EHR VENDORS. EHR VENDORS THAT OFFER TOP EHR VENDORS 2015 CEHRT PRODUCT. Epic, 71% CPSI, 7%. Epic, 52% Centricity, 10% Credible, 10% Qualifacts, 9% Epic, 28% Dentrix, 25% Hospitals (n 60) Patient-Centered Primary Care Homes (n 623) Behavioral health-only agencies