Transcription
OVERVIEW OFVIRGINIA MEDICAIDJENNIFER LEE, MDDIRECTOR,DEPARTMENT OF MEDICALASSISTANCE SERVICES
DMAS MissionEnsure Virginia’s Medicaid EnrolleesReceive Quality Health CareSuperior Care2Cost EffectiveContinuous Improvement
Virginians Covered by Medicaid/CHIP1 in 8 Virginians rely onMedicaidMedicaid covers 1 in 3births in VirginiaMedicaid is the primary33% of children inpayer for behavioralhealth servicesVirginia are covered byMedicaid & CHIP2 in 3 nursing facilityresidents are supported byMedicaid62% of long-term servicesand supports spending is inthe communityMedicaid plays a critical role in the lives of over 1.3 million Virginians3
Who Medicaid ServesGrowing Kids: Every baby deserves a healthy start and DMAS focuses on keeping childrenhealthy through the Medicaid and the Family Access to Medical Insurance Security (FAMIS)programs. Medicaid and FAMIS cover the medical and dental care that growing children need.Pregnant Women: Good health care during pregnancy is important for both mother and baby.The FAMIS Moms Program assists pregnant women with regular prenatal and dental care toincrease the likelihood for healthy birth outcomes.Older Adults: Medicaid is the primary payer for long term services and supports for Virginia’saging population. The use of home and community based waivers allow individuals to receive thecare and support they need in the comfort of their own home.People with Behavioral Health Conditions: Virginia Medicaid provides an array of behavioralhealth and addiction and recovery treatment services to all enrollees.Individuals in the Community: Home and Community-Based Services (HCBS), like theCommunity Living Waiver, help enrollees transition to community settings of their choice as analternative to institutionalization.4
Benefits: Covered Groups and ServicesMedicaid coverage is primarilyavailable to Virginians who meetspecific income thresholds andother eligibility criteria, including:Long TermServices &SupportsAcuteCareBehavioralHealth children pregnant women adults the aged, blind, andindividuals with disabilitiesPrimaryCareDental Eligibility is complex and not all Virginians with low income are covered5
Who Qualifies for Virginia MedicaidNot all low-income Virginians are eligible148% FPL ( 17,967)Children 0-18148% FPL ( 17,967)Pregnant Women80% FPL ( 9,712)Elderly & DisabledWorking ParentsChildless Adults52% FPL ( 6,313)Not Eligible
Medicaid ProgramsThe following specialized Medicaid benefits and programs target certain services andinterventions to designated es (ARTS)Governor’sAccess Plan(GAP)Program of AllInclusive Care forthe Elderly (PACE)7Features Launched April 1, 2017 Provides the full continuum of evidence-based addiction treatment to any of the1.3 million Medicaid and FAMIS members who need treatment Launched in January 2015 Provides primary care and behavioral health services for 15,352 uninsured, seriouslymental ill Virginians with incomes at or below 80% of the Federal Poverty Level Increases access to care, and improves physical and behavioral health outcomes. Serves dual eligibles aged 55 or older, qualifying for nursing home level of care Offers a community alternative to NH care and provides the full continuum ofmedical and social supports via a interdisciplinary care model
Medicaid Programs continuedProgramFosterCareHealth andAcute CareOralHealthDisease CaseManagement8FeaturesBenefitsMedallion 3.0 serves 82% of the 13,362 Foster Careand Adoption Assistance (FC/AA) membersFC/AA members are assigned a Foster care professionalfrom their MCOs who will work collaboratively with DMASand the Department of Social Services to address memberneedsHAP provides integrated care coordination for 9,600members enrolled in both Medallion 3.0 and a homeand community-based waiverDMAS offers Intra-Disciplinary Team (IDT) casemanagement for problem resolution with medical,pharmacy, or long-term care servicesMedallion 3.0 collaborates with DentaQuest as theDental Benefits AdministratorMedallion 3.0 connects members to oral health providers,raising awareness of oral health issues, and providingquality dental care for Medicaid and FAMIS membersEach MCO offers disease case management programsto promote active member participation in managingchronic medical or behavioral health conditionsMCOs offer members support and education to improvetheir health condition. Intervention includes diseaseprevention using tailored educational materials, nurseassessments, or intervention and home monitoring ifneeded
Home and Community-Based Services WaiversThe Medicaid home and community based waivers offer individuals who require assistancewith activities of daily living and/or supportive services the opportunity to receive care in thecommunity rather than in a facility settingWaiverAlzheimer’sAssisted LivingWaiverCommunity LivingWaiverFamily andIndividual ovides assistance with activities of daily living, housekeeping, and supervision; medication administration;nursing evaluations and weekly activity program based on needs and interests.Provides 24/7 services and supports for adults and some children with exceptional medical and/or behavioralsupport needs. This includes residential supports and a full array of medical, behavioral, and non-medical supports.Provides supports for children and adults living with their families, friends, or in their own homes, includingsupports for those with some medical or behavioral needs.Provides supports for adults able to live independently in the community with housing subsidies and/or othertypes of support. The supports available in this waiver will be periodic or provided on a regular basis as needed.Elderly or Disabledwith ConsumerDirection WaiverProvides supports for elderly and disabled individuals including adult day health care; medication monitoring,personal care services; respite care; personal emergency response systems, transition coordination and services.TechnologyAssisted WaiverProvides supports for children and adults who are chronically ill or severely impaired and require both a medicaldevice and substantial and ongoing skilled nursing care to avert further disability or to sustain their lives9
Funding Medicaid Coverage State ReceivesFederal Match(50% Match Rate)StateAppropriatesGeneralFundsDMAS10% ofMedicaidMembers90% ofDMAS Pays for MemberHealth Care ServicesFee-For-Service (FFS)Providers PaidDirectly10MedicaidMembersManaged Care: MCOCoordinates Care and Contractswith Providers to DeliverServices
Virginia Medicaid: Enrollment & ExpendituresEnrollment vs. Expenditure SFY 2017100%24%80%12%20%Children in LowIncome Families60%48%40%20%0%Parents,Caregivers &PregnantWomen48%20%8%Enrollment28% of the Medicaid population20%Individuals withDisabilitiesOlder AdultsExpendituresDrives68% oftotal expendituresExpenditures are disproportionate to the population where services for older adults andindividuals with disabilities drive a significant portion of Medicaid costs11
Medicaid BudgetOnly 2.2% of the total DMAS budget is for administrative expensesTotal FY17 BudgetMedicalServices97.5%97.5% of the DMASbudget funds medicalexpenses*Note: Health IT Incentive Payments are funded by 100% federal funds.12Admin2.2%Health ITIncentivePayments0.3%*
Major Initiatives of Virginia Medicaid1Launched Commonwealth CoordinatedCare Plus for ABDs in August 20172Launch updated managed care programfor pregnant women & children(Medallion 4.0) in 20183Procure many technology changes(Medicaid Enterprise System) 2017-184Launched Substance Use Services(ARTS) in 2017 90% of Virginia Medicaid enrollees are in managed care13
Strategic Transition to Managed CareTwo managed care programsCCC Plus14Medallion 4.0 Serving older adults and disabled Includes Medicaid-Medicareeligible 216,000 individuals Serving infants, children,pregnant women, parents 760,000 individuals Long-term services and supports inthe community and facility-based,acute care, pharmacy Incorporating community mentalhealth Births, vaccinations, well visits, sickvisits, acute care, pharmacy Incorporating community mentalhealth Implementation started Aug 2017 Implement statewide byJan 2018 New procurement 2017 Implementation August 2018 Building on two decades ofmanaged care experience Approximately 30B over 5 years Estimated 10B - 15B over 5 years
CCC Plus PopulationsApproximately 210,000 individuals, including: Individuals age 65 and older Adults and children living with disabilities Individuals living in Nursing Facilities (NFs) Individuals in the CCC Plus Waiver (formerly the Tech Assisted Waiver andEDCD Waiver) Individuals in the 3 waivers serving the DD populations for their acute andprimary services *CCC and Medallion 3 ABD populations transitioned to CCC Plus on 1/1/201815
6 Health Plans Contracted Statewide Aetna Better Health of Virginia Anthem HealthKeepers Plus Magellan Complete Care ofVirginia Optima Health United Healthcare Virginia Premier Health PlanA list of CCC Plus regions by locality is available at: http://www.dmas.virginia.gov/Content pgs/mltss-proinfo.aspx16
Current CCC Plus Enrollment by RegionCCC Plus EnrollmentAs of Week eghanySouthwestNorthern 142,1793,0892,2427,01223,378VA er
Care Coordinator ExpectationsVirginia continues to take a collaborative, hands-on approach with MCOs toestablish clear expectations for care coordinatorsDMAS Tech Waiver SMEs communicate with ALL health plans Customized Training On-Site for Continued Training and Education Clinical Case Reviews and Necessary Follow Up Joint Home Visits as necessaryTimely Information Sharing, Communication, & Training Weekly Training Calls on services, success stories, case reviews and scope of CareCoordinator role – Average over 300 participants on each call Coffee Talk Tuesdays dedicated to Live Q&A - Call limit reached weekly with 150callers Specialized training based on identified learning needs i.e. EPSDT, DD Waivers, etc.Questions Answered Directly from Care Coordinators Dedicated Email box for their questions,, concerns and requests for training Direct communication with DMAS Care Management Staff Email notices to growing group of registered Care Coordinators – currently over500Direct Issue Resolution Process with Care Coordinator Management and ClinicalLeads18
MEDALLION 4.0will cover 737,146 Medicaid and FAMIS* memberseffective August 1, 2018*depending upon re-authorization19
MEDALLION 4.0Program Themes & Focus Maternal child health partnerships Behavioral health models Expansive networks Strong compliance and reporting Provider and member engagement Innovation Quality, data, and outcome focus20
MEDALLION 4.0 PROGRAM DESIGN Medallion 4.0 1915 (b) waiver covers pregnant women, infants, children,and parents/care caregivers New carved in populations and services: Early Intervention Services Third Party Liability (TPL) – “other insurance” Community Mental Health and Rehabilitation Services (CMHRS) Our focus is on each covered population Will serve as the platform for access to health care forthose enrolled under the Medicaid expansion along withCCC Plus Members have a choice of six plans in each of the sixregions21
MEDALLION 4.0Six Regions22
M4.0 HEALTH PLANSMagellan23COMPLETE CARE OF VIRGINIA
ADDING NEW INNOVATIONSwhile KEEPING THE BEST OF MEDALLION 3.0 andALIGNING WITH CCC PLUS 24Program Statewide and regions High program acceptance Quality program HEDIS NCQA Accredited Expansive Networks Adequate Rates Compliance and TechnicalManual Managed Care SystemPartnerships ARTS (April 2017) Performance Incentive Award(PIA) Innovation Enhanced Services Common Core Formulary Telehealth Program Integrity CMS managed care regulations ED Care Coordination Data integrity and encounters Social Determinants of Health Value Based Payments
INFANTS 0-325 Increase Immunizations Increase Well Visits Early Assessments Safe Sleep Neonatal Abstinence Syndrome (NAS)Babies Reduction in Infant Death (ThreeBranch Workgroup) Early Detection, Screening, andIntervention Zero to Three Workgroup
MATERNITY26 Early Prenatal Care Increase Case Management Increase Post Partum Care includingdepression screenings Less Early Elective Deliveries Lower C-Section Rate Breast Feeding Increase Family Planning Utilization Increase HEDIS scores Addiction and Recovery Treatment Services(ARTS) More Outreach and Education Use of Social Media Possible Value-Based Purchasing Possible Kick Payment
CHILDREN 3-18 27Increase Obesity Oral Health Asthma Vision Blood Lead Screening Well Visits Adolescent FocusEarly and PeriodicScreening, Diagnosis, andTreatment (EPSDT)
CHILDREN 3-18 28Special Needs ChildrenTrauma Informed Care and ResiliencyCommunity Mental Health and Rehabilitation Services (CMHRS)Improve Coordination Department of Education (DOE) Department of Social Services (DSS) Virginia Department of Health (VDH) Department of Behavioral Health and Developmental Services (DBHDS)
ADULTS Wellness Behavioral Health and CMHRS Chronic Diseases Family Planning/Long Acting Diabetes Hypertension Heart Disease Obesity Specialty Programs29Reversible Contraceptive (LARC) Social Determinants of Health Emergency Department Use Base for Medicaid Expansion
HEALTH SYSTEM IMPACTAll 13 Major Health SystemsContract With M3 Health PlansInova Health SystemVCUSentaraWellmontBon SecoursCarilionCentra30HCAINOVALifePointMountain States UVARiversideValleySentaraVCUWellmont
ROBUST NETWORKS Currently, over 100,000 providers serving members at more than300,000 sites across the Commonwealth Provider network and management staff that DMAS does not have Ability to recruit, credential providers and manage networks Plan specific provider agreements and payments Target provider enrollment based on population characteristics Ability to create individual out of network provider agreements forcases where a member has special needs, requests orcircumstances Supports new models: integrating behavioral health medicalhomes, pilots Ability to leverage commercial and health system relationships31
TIMELINE Request for Proposal (RFP): Spring 2017 Selection for negotiations: November 2017 Draft contract and rates: November 2017 Notice of intent to award: December 2017 Contract signed: April 2018 Regional implementations: 2018 August, September, October, November, December Concurrent operation of Medallion 3.0 and MEDALLION 4.032
REGIONS AND EFFECTIVE ENROLLMENT DATESRegionsProposed Effective DatesTidewaterAugust 1, ernRoanoke/AlleghanySouthwest33September 1, 2018October 1, 2018November 1, 2018December 1, 2018December 1, 2018
ARTS Program: Transforming the Delivery Systemof Medicaid SUD gementARTS4/1/17PeerRecoverySupportsEffective July 1, 2017Magellan will continue tocover community-basedsubstance use disordertreatment services for feefor-service membersAll ARTS Servicesare Covered byManaged CarePlansA fully integratedPhysical andBehavioral HealthContinuum of Care
Increases in Addiction Providers Due to ARTSOver 350 new Addiction Treatment Provider Organizations in MedicaidAddiction Provider TypeInpatient Detox (ASAM4.0)Residential Treatment(ASAM 3.1, 3.3, 3.5, 3.7)Partial HospitalizationProgram (ASAM 2.5)Intensive OutpatientProgram (ASAM 2.1)3# of Providersbefore ARTS# of Providersafter ARTS% Increase inProvidersUnknown103NEW478 1850%013NEW4972 47%Opioid Treatment Program629 383%Office-Based OpioidTreatment Provider079NEW
Highlights From the First Nine Months of ARTSIncrease in total number of Substance Use Disorder Outpatient ProvidersBefore ARTS(Apr-Dec 2016)(Apr-Dec 2017)9502,544Physicians2231359NP16155Counselors and SW267350Other444680Total number ofSUD OutpatientProvidersBy Provider TypeAfter ARTSSource: Independent Evaluation by Virginia Commonwealth University36% Change 168% 509% 869% 31% 53%
Highlights From the First Nine Months of ARTSMore members are receiving treatment for all Substance UseDisorders (SUD) and Opioid Use Disorder (OUD)Before ARTS(Apr-Dec 2016)Members withSUD receivingtreatmentMembers withOUD receivingtreatmentAfter ARTS(Apr-Dec 2017) 64%10,10216,570 51%6,98910,522Source: Independent Evaluation by Virginia Commonwealth University37% Change
Highlights From the First Nine Months of ARTSFewer Emergency Department (ED) visits and decreased costs relatedto Opioid Use Disorder (OUD)Before ARTS(Apr-Dec 2016)After ARTS(Apr-Dec 2017)ED Visits relatedto OUD 31%4,4843,101Total Spendingon ED Visits 27% 7,950,0195,776,221Source: Independent Evaluation by Virginia Commonwealth University38% Change
Highlights From the First Nine Months of ARTSEffect of ARTS on the Number of ED Visits for MedicaidMembers with an Opioid Use Disorder1.41.21.00.80.60.40.20.02016 Q12016 Q22016 Q3OUD2016 Q4Non-SUD2017 Q1OUD without ARTSSource: Independent Evaluation by Virginia Commonwealth University2017 Q22017 Q3
Highlights From the First Nine Months of ARTSDecrease in total number of prescriptions and members withprescriptions for Opioid pain medicationsBefore ARTS(Apr-Dec 2016)Total number ofprescriptions foropioid painmedicationNumber ofmembers withprescriptions forOpioid painmedicationsAfter ARTS(Apr-Dec 2017) 29%420,883299,598 16%116,28697,529Source: Independent Evaluation by Virginia Commonwealth University40% Change
Coming Soon: Medicaid Expansion! Starting early 2019 400,000 more adults living in Virginia will have access toquality, low cost health coverage41
Who is EligibleCover Virginia will provide low and no-cost health care coverage to expansion eligible individuals Adults ages 19 – 64, not Medicare eligible Income from 0% to 138% Federal Poverty Level Not already eligible for a mandatory coverage group42
Cover Virginia Proposed Alternative Benefit PlanThe Cover Virginia alternative benefit plan (ABP) would includes all State Plan services andadditional adult preventive services from the benchmark planCovered Benefits Doctor, hospital, and emergency services Prescription drugs Laboratory and x-ray services Maternity and newborn care Behavioral health services including addiction andrecovery treatment services Rehabilitative and habilitative services includingphysical, occupational, and speech therapies andequipment Family planning services Transportation to medical appointments when nototherwise available Home health services Durable medical equipment (DME) and supplies Long term care and support services (NF, PACE, andHCBS) Preventive and wellness services and diseasemanagement services1ABP43follows existing Medicaid cost sharing provisions until Track 2 Reforms are implementedDelivery SystemsManaged Care and Fee-For-Service CCC Plus – Medically Frail Medallion 4.0 - Not Medically Frail Fee-For-Service - Awaiting managedcare enrollment
Medicaid Reforms: Dual Track Process as Outlined inThe 2018 Appropriations ActThe 2018 Appropriations Act directs DMAS to:1.Amend the State Plan for Medical Assistance, and any waivers thereof, toimplement coverage for newly eligible individuals under the ACA (Track 1)2.Begin the process of implementing a § 1115 demonstration project to transformthe Medicaid program for newly eligible individuals and eligible individualsenrolled in the existing Medicaid program (Track 2)Track 1: Implemented via contracts and/or other policy changesTrack 2: 1115 Demonstration WaiverCoverage fornewly eligible individualsRequired reforms that transform the Medicaidprogram for eligible individualsDMAS would work in parallel to begin the process of applying for a 1115 waiver at the sametime as submission of the State Plan Amendments to CMS44
Medicaid Expansion: Phase 1To be implemented through contracts and/or other policy changes Referrals to job training, education, and job placement assistance forall unemployed, able-bodied adults Health and Wellness Accounts Appropriate Utilization of ED Services Healthy Behavior Incentives Enhanced Fraud Prevention Efforts45
Medicaid Expansion: Phase 2Reforms Required with Track 2 – § 1115 Waiver 46Population earning 100-138% Federal Poverty Level Monthly Premiums, copayments and deductibles Waiting period prior to re-enrollment if premium not paid Cost-sharing to promote healthy behaviors and appropriate ED use Cost-sharing reductions for compliance with healthy behaviorsTraining, Enrollment, Education, Employment and Opportunity Program (TEEOP) Gradually escalating participation in community engagement increases to at least80 hours per month Community engagement includes employment, job skills training, job searchactivities, education, volunteering, and caregiving Exemptions – medically frail, children 18 y/o, individuals 55 y/o, primarycaregivers with a dependent child 18 y/o, etc.
Provider Assessments Two types of provider assessments: Coverage Assessment Payment Rate Assessment Most private hospitals required to pay assessments Exempted hospitals include: Public hospitals Freestanding psychiatric or rehabilitation hospital Children’s hospital Long-stay hospital Long-term care hospital Critical access hospital47
Coverage Assessments Hospitals pay for state’s share of the cost of coverage for theexpansion population Federal government pays 93% of cost through 2019, then 90% in2020 Assessment percentage set by DMAS Approximately 0.5% in FY19 and 1.4% in FY20 Funds generated from assessment deposited in a non-reverting fundat the State Treasury fund Funds can only be used to fund cost of non-federal share ofMedicaid expansion Funds left over at end of year will reduce amount of funds to becollected the following year Virginia hospitals expected to receive approximately 36% of the newspending on expansion48
Payment Rate Assessments Hospitals pay the state share of the cost of increasing reimbursementrates up to the “upper payment limit” and to fill the “MCO hospital gap” Upper payment limit: Applies to FFS claims and is the maximum Medicaid can pay for services (equal towhat Medicare pays for services) MCO hospital gap: Applies to MCO payments and is the difference between what MCOs pay and themaximum Medicaid could have paid for the service under FFS This payment rate assessment will result in hospitals receiving paymentsthat bring up their net reimbursement to approximately the same levels aspaid by Medicare (88% of cost) These funds can only be used to fund costs of the non-federal share ofsupplemental payment rate increase Funds left over at end of year will reduce amount of funds needed to becollected the following year49
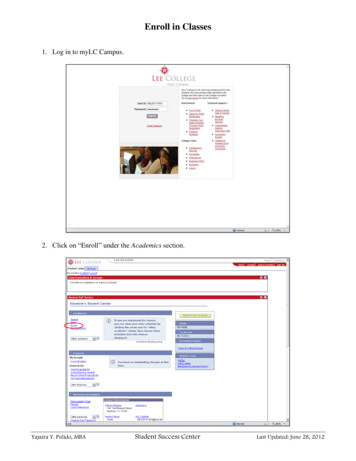
Next Steps – After Budget signing 50Program Authorities – SPAs, WaiverSystems ChangesStreamlined Enrollment StrategiesContract Modifications and RatesCommunications and OutreachEducation and TrainingTesting and ReadinessImplementation
Regular Updates About Medicaid ExpansionThe CoverVA.org website will soon have additional information on: Who is eligible Household income Other qualifications Frequently asked questionsNew information will be added often so check back frequently forupdates51
Partner with us on ExpansionHospitals and health systems can help support Medicaid expansion Assist with intensive marketing and outreach to educate and informnewly eligible individuals, providers, and other stakeholders Support enrollment efforts and access to services for newly eligibleindividuals, including presumptive eligibility determinations Share the Cover Virginia banner and link on your website and socialmedia pages52
Medallion 3.0 collaborates with DentaQuest as the Dental Benefits Administrator . Medallion 3.0 connects members to oral health providers, raising awareness of oral health issues, and providing . 90% of Virginia Medicaid enrollees are in managed care. Launch updated managed care program for pregnant women & children (Medallion 4.0 ) in 2018. 2.