Transcription
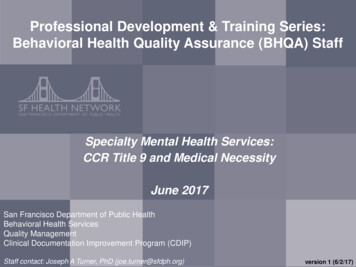
Professional Development & Training Series:Behavioral Health Quality Assurance (BHQA) StaffSpecialty Mental Health Services:CCR Title 9 and Medical NecessityJune 2017TitleSan Francisco Department of Public HealthBehavioral Health ServicesQuality ManagementClinical Documentation Improvement Program (CDIP)SubtitleStaff contact: Joseph A Turner, PhD (joe.turner@sfdph.org)1version 1 (6/2/17)
Agenda Problem: People Do Not Understand Quality assurance Let’s learn the “theory” behind the practice (30mins) Managed care Let’s learn about a public model (30mins) Medical necessity Let’s improve our skills in this area (60mins)Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/20172
Handouts Build a binder for workshop materials: Powerpoint: steal these slides for your training! CDIP CCR Title 9: a must-have reference for a true QAprofessional CDIP Medical Necessity Tool: let’s standardize thiswork Bonus Materials: know your history and profession.Read about SF managed care (circa 1995) andconceptual issues in medical necessityStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/20173
“Quality Assurance” inYour Organization Agency-Level Definition of QA: What is your job title? What are you monitoring/improving? What is the impact of your work (how does your workmake a difference)? What are you major work activities?Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/20174
“Quality Assurance” inYour OrganizationJob TitleDirector of QualityManagementTarget/Focus ofWorkMonitoring contractUoS PURQCImpact of WorkMitigate financialrisk growbusinessExample WorkActivitiesCalculate/reportmonthly UoS (forCFO) and PURQC(for program)example above is from prior jobStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/20175
Jargon Check: Quality Assurance organizedsystem to monitor& improve quality retrospectivecomparison againsta standardStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org) real-timeinvestigation ofprocesses6/2/20176
Switching Gears Different people define QA/QI/QMdifferently how does your organization see qa/qi/qm? how do managedStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)care organizations see it?6/2/20177
Managed CareINSURANCE COMPANYthey sell you the policyStep1MANAGED CARE ORG. COMPANYthey administer the benefits of the policyStep2Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/20178
Managed CareI have limited money totake care ofEVERYBODY!I can keep the savings if IMANAGE the moneywell!:\MANAGED CARE ORGANIZATION COMPANYStep3Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)they hold the risk6/2/20179
Managed CarePROVIDERthey deliver the serviceStep4PIGGYBANKtherapistMANAGED CARE ORG. COMPANYclientsthey pay provider & save (hopefully)Invoice 100 Units ofTherapy 200 Units ofTCMStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)Step56/2/201710
Managed CareHow Do Managed Care OrganizationsManage Their Risk?Gatekeepers!(no accessing specialists without permission)Utilization Management(monitoring for too much/little)Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201711
Managed CareUtilization Management(monitoring for too much/little)is the service medically necessary?Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201712
Switching Gears QA people are frequently involved in“Utilization Management” balancing the needs of a population & limited dollars how does CA do ManagedStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)Care for Medicaid?6/2/201713
California’s Managed Care MedicaidProgramInsurance Company(California State)Managed Care Org(SFDPH-BHS)Provider(you)Customer/Client(our clients)Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201714
California’s Managed Care Medicaid:Three Benefits“Medi-Cal Insurance”Physical er.PlanMental HealthMedi-CalDrug Medi-Cal(ODS)BHS(CountyMHP)BHS(CountySUDP) Physical health care SMHS Mild/Moderate MH care Moderateto SevereMH care Autism Spectrum/BHTStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org) SpecialtySUD Moderateto SevereSUD care6/2/201715
California’s Managed Care MedicaidProgramYou build a publicly funded managed careMedicaid program by following blueprints & rules!“CCR Title 9”(a regulation)Blueprint(build a County Mental Health Plan)Rules(operate a County Mental Health Plan)16
California’s Managed CareMedicaid & CCR Title 9 California LawCA GovernorCA GovernorCA Assembly California RegulationCASenateThe 29 California Codes (California’s Statutory Law)Business & Professions CodeFish & Game CodePublic Contract CodeCivil CodeFood & Agricultural CodePublic Resources CodeCode of Civil ProcedureGovernment CodePublic Utilities CodeCommercial CodeHarbors & Navigation Code Revenue & Taxation CodeCorporations CodeHealth & Safety CodeStreets & Highways CodeEducation CodeInsurance CodeUnemployment Insurance CodeElections CodeLabor CodeVehicle CodeEvidence CodeMilitary & Veterans CodeWater CodeWelfare & Institutions CodeFamily CodePenal CodeFinancial CodeProbate CodeStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)Dept of Transportation, Housing andCommunity Development, Real Estate,Aging, Social Services, Consumer Affairs,Fish & Game, Health Care ServicesThe 27 Regulatory “Titles” of the California Code of Regulations (CCR)Title 1: General ProvisionsTitle 15: Crime Prevention & CorrectionsTitle 2: AdministrationTitle 16: Professional & Vocational RegulationsTitle 3: Food & AgricultureTitle 17: Public HealthTitle 4: Business RegulationsTitle 18: Public RevenuesTitle 5: EducationTitle 19: Public SafetyTitle 7: Harbors & NavigationTitle 20: Public Utilities & EnergyTitle 8: Industrial RelationsTitle 21: Public WorksTitle 9: Rehabilitative & Developmental Services Title 22: Social SecurityTitle 10: InvestmentTitle 23: WatersTitle 11: LawTitle 24: Building Standards CodeTitle 12: Military & Veterans AffairsTitle 25: Housing & Community DevelopmentTitle 13: Motor VehiclesTitle 26: ToxicsTitle 14: Natural ResourcesTitle 27: Environmental Protection6/2/201717
California’s Managed CareMedicaid & CCR Title 9The 27 Regulatory “Titles” of the California Code of Regulations (CCR)Title 1: General ProvisionsTitle 15: Crime Prevention & CorrectionsTitle 2: AdministrationTitle 16: Professional & Vocational RegulationsTitle 3: Food & AgricultureTitle 17: Public HealthTitle 4: Business RegulationsTitle 18: Public RevenuesTitle 5: EducationTitle 19: Public SafetyTitle 7: Harbors & NavigationTitle 20: Public Utilities & EnergyTitle 8: Industrial RelationsTitle 21: Public WorksTitle 9: Rehabilitative & Developmental ServicesTitle 22: Social SecurityTitle 10: InvestmentTitle 23: WatersTitle 11: LawTitle 24: Building Standards CodeTitle 12: Military & Veterans AffairsTitle 25: Housing & Community DevelopmentTitle 13: Motor VehiclesTitle 26: ToxicsTitle 14: Natural ResourcesTitle 27: Environmental ProtectionStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)Regulations BLUEPRINTS &RULES6/2/201718
California’s Managed CareMedicaid & CCR Title 9 California Code of Regulations (blueprints rules):Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201719
California’s Managed CareMedicaid & CCR Title 9 CCR Title 9 Rehabilitative & Developmental Services Division 1 Department of Mental Health Chapter 11 Medi-Cal Specialty Mental Health Services Subchapter 3 Specialty Mental Health Services Other thanPsychiatric Inpatient Hospital ServicesRegulations BLUEPRINTS &RULESStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201720
California’s Managed CareMedicaid & CCR Title 9DomainDetailDocumentReferenceMedicalNecessity (NonHospital) Medi-Cal criteria (diagnosis, impairments, interventions)EPSDT criteria§1830.205 &§1830.210(p75)Definitions ofServices Definition of assessment, plan development, etc.§1810.204(p4-)NonReimbursableServices Academic educational servicesVocational services with actual work/training as thepurposeRecreationSocialization without systematic individualized feedbackBoard/care costs of Adult Residential, Crisis Residential,etc.Services provided in an IMD (21yo-64)Subchapter 4,Article 3 (ps92-93) Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201721
California’s Managed CareMedicaid & CCR Title 9DomainDetailDocument ReferenceManaged CareDuties ACCESS: County must have 24/7 accessibility to servicesCULTURE/LANUGAGE: County must have cultural competence plan andoffer services in threshold languagesPROVIDERS: County must have organizational, group and individualproviders in their networkSubchapter 1, Article 4(ps44-47) QualityManagement QM Director reports to Director of Mental Health PlanQM Program involves providers and consumersQM monitors grievances, appeals and clinical recordsMaintains Utilization Management programEnsures documentation/medical records are complete (signed byclient/provider)Subchapter 1, Article 4(ps55-57)FederalFinancialParticipation “Claiming” is the process by which MHPs obtain FFP.“Reimbursement” means a payment of FFPSubchapter 4, Article 1 (ps85-86)Claiming &Lockouts Claiming for services by minutes, hours, daysService Lockouts (by service)Subchapter 4, Article 3 (ps94-108)Certification ofClaims by MHP Assessment is complete/correctTPOC is complete/correctClient was eligible to receive servicesThe client actually received the servicesMedical necessity for every service was metSubchapter 4, Article 1 (ps87-88)Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201722
Switching Gears QA people have a role to play inCalifornia’s Managed Care MedicaidProgram CCR Title 9, Chapter 11 is your friend! let’s teach providers MedicalStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)Necessity!6/2/201723
Specialty Mental Health Services (SMHS)Medical Necessity QUESTIONS: Do you understand medical necessity as outlined inTitle 9? Do your clinic staff understand medical necessity asoutlined in Title 9? Is it possible to have a common understanding ofmedical necessity? Who would benefit if we had a commonunderstanding of medical necessity?Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)24
Specialty Mental Health Services (SMHS)Medical NecessityCCR Title 9 Definition of Medical Necessity:§1830.205. Medical Necessity Criteria for MHP Reimbursement of Specialty Mental Health Services.(a) The following medical necessity criteria determine Medi-Cal reimbursement for specialty mental health services that are the responsibility of the MHP under this Subchapter, except asspecifically provided. (b) The beneficiary must meet criteria outlined in Subsections (1)-(3) below to be eligible for services: (1) Have one of the following diagnoses in the Diagnostic andStatistical Manual of Mental Disorders, DSM-IV , Fourth Edition (1994), published by the American Psychiatric Association:(A) Pervasive Developmental Disorders, except Autistic Disorders; (B) Disruptive Behavior and Attention Deficit Disorders; (C) Feeding and Eating Disorders of Infancy and EarlyChildhood; (D) Elimination Disorders; (E) Other Disorders of Infancy, Childhood, or Adolescence; (F) Schizophrenia and other Psychotic Disorders, except Psychotic Disorders due to aGeneral Medical Condition; (G) Mood Disorders, except Mood Disorders due to a General Medical Condition; (H) Anxiety Disorders, except Anxiety Disorders due to a General MedicalCondition; (I) Somatoform Disorders; (J) Factitious Disorders; (K) Dissociative Disorders; (L) Paraphilias; (M) Gender Identity Disorder; (N) Eating Disorders; (O) Impulse Control DisordersNot Elsewhere Classified; (P) Adjustment Disorders; (Q) Personality Disorders, excluding Antisocial Personality Disorder; (R) Medication-Induced Movement Disorders related to otherincluded diagnoses.(2) Have at least one of the following impairments as a result of the mental disorder(s) listed in Subsection (b)(1) above: (A) A significant impairment in an importantarea of life functioning. (B) A reasonable probability of significant deterioration in an important area of life functioning. (C) Except as provided in Section 1830.210, a reasonable probabilitya child will not progress developmentally as individually appropriate. For the purpose of this Section, a child is a person under the age of 21 years. (3) Meet each of the intervention criterialisted below: (A) The focus of the proposed intervention is to address the condition identified in Subsection (b)(2) above. (B) The expectation is that the proposed intervention will: 1.Significantly diminish the impairment, or 2. Prevent significant deterioration in an important area of life functioning, or 3. Except as provided in Section 1830.210, allow the child to progressdevelopmentally as individually appropriate. 4. For a child who meets the criteria of Section 1830.210(1), meet the criteria of Section 1830.210(b) and (c). (C) The condition would not beresponsive to physical health care based treatment. (c) When the requirements of this Section or Section 1830.210 are met, beneficiaries shall receive specialty mental health services fora diagnosis included in Subsection (b)(1) even if a diagnosis that is not included in Subsection (b)(1) is also present.§1830.210. Medical Necessity Criteria for MHP Reimbursement for Specialty Mental Health Services for Eligible Beneficiaries under 21 Years of Age. (a) For beneficiaries under 21 yearsof age who are eligible for EPSDT supplemental specialty mental health services, and who do not meet the medical necessity requirements of Section 1830.205(b)(2)-(3), medicalnecessity criteria for specialty mental health services covered by this Subchapter shall be met when all of the following exist: (1) The beneficiary meets the diagnosis criteria in Section1830.205(b)(1), (2) The beneficiary has a condition that would not be responsive to physical health care based treatment, and (3) The requirements of Title 22, Section 51340(e)(3)(A) aremet with respect to the mental disorder; or, for targeted case management services, the service to which access is to be gained through case management is medically necessary for thebeneficiary under Section 1830.205 or under Title 22, Section 51340(e)(3)(A) with respect to the mental disorder and the requirements of Title 22, Section 51340(f) are met. (b) The MHPshall not approve a request for an EPSDT supplemental specialty mental health service under this Section or Section 1830.205 if the MHP determines that the service to be provided isaccessible and available in an appropriate and timely manner as another specialty mental health service covered by this Subchapter and the MHP provides or arranges and pays for sucha specialty mental health service. (c) The MHP shall not approve a request for specialty mental health services under this Section in home and community based settings if the MHPdetermines that the total cost incurred by the Medi-Cal program for providing such services to the beneficiary is greater than the total cost to the Medi-Cal program in providing medicallyequivalent services at the beneficiary’s otherwise appropriate institutional level of care, where medically equivalent services at the appropriate level are available in a timely manner, andthe MHP provides or arranges and pays for the institutional level of care if the institutional level of care is covered by the MHP under Section 1810.345, or arranges for the institutionallevel of care, if the institutional level of care is not covered by the MHP under Section 1810.345. For the purpose of this Subsection, the determination of the availability of an appropriateinstitutional level of care shall be made in accordance with the stipulated settlement in T.L. v. Belshé.Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)25
Specialty Mental Health Services (SMHS)Medical NecessityCDIP View of Medical Necessity:.Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)26
Teaching SMHS Medical Necessity Easy-Peasy: Included Diagnosis Standard interpretation: if it appears on the listpublished by DHCS, it’s included Source document: DHCS MHSUD (Mental Health &Substance Use Disorder Services) Information Notice#15-030 (initial ICD10 crosswalk) and #16-106(corrected and updated including no diagnosis(Z03.89) and diagnosis deferred (R63)Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201727
Teaching SMHS Medical Necessity Easy-Peasy: Included Diagnosis Standard Charting: State the client meets DSM criteriaFully describe symptoms/behaviors that qualify (onset,frequency, duration, severity, impact)Describe the mechanism by which symptoms impair theclient’s functioningAll information needed to justify diagnosis is contained in the“Presentation” and “Impact on Functioning” sections of assmtStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201728
Teaching SMHS Medical Necessity Easy-Peasy: Included Diagnosis CCR Title 9 §1830.205: does not identify specificdiagnoses! Only gives the general categories ofdiagnoses from DSM-IV.“ Have one of the following diagnoses in the Diagnostic andStatistical Manual of Mental Disorders, DSM-IVE, Fourth Edition(1994), published by the American Psychiatric Association ”Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201729
Teaching SMHS Medical Necessity Easy-Peasy: Condition not Responsive toPhysical Health Care Based Treatment Standard interpretation: “Condition” functional impairment (citation DHCSMHSUDS Information Notice 16-061)“Not Responsive” not improving“Physical Health Care Based Treatment” general healthcare services focused on physical conditions/diseasesStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201730
Teaching SMHS Medical Necessity Tougher: Pathway #2/Current SignificantImpairment-Important Area of LifeFunctioning STANDARDIZING interpretation/charting: Current past 30 days [citation BHS Memo: Using the CBHSelectronic health record (Avatar) to track and maintain Assessment andTreatment Plan of Care (TPOC) timeliness.] “Impairment” the disability caused by thesymptoms/behaviors of the diagnosis (citation MHSUD InfoNotice 16-061)Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201731
Teaching SMHS Medical Necessity Tougher: Pathway #2/Current SignificantImpairment-Important Area of LifeFunctioning STANDARDIZING interpretation/charting: “Significant” Important and real (genuine, palpable,practical, noticeable) in its impact to the person“Significantly diminish”: (a) diminish: to make or becomeless; to decrease in size, extent, or range; (b) significant couldbe objective measures (e.g., 2 1 on the ANSA;clinical nonclinical status on CBCL)Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201732
Teaching SMHS Medical Necessity Tougher: Pathway #2/Current Significant ImpairmentImportant Area of Life Functioning Standard interpretation: “Important Area of Life Functioning” IS SQUISHYHow can we try to understand?Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201733
Teaching SMHS Medical Necessity Sources of Info & Models: Important Area of LifeFunctioning1. General Community MH/Systems of Care Logic:a) Home Functioningb) School/Work Functioningc) Community Functioninga SAFE strategy!Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201734
Teaching SMHS Medical Necessity Sources of Info & Models: Important Area of LifeFunctioning2. BHS AVATAR Prompts on Screen-Assessment:a) CYF: Describe impact of the mental health problem on selfcare, home, pre-school and communityb) A/OA: impact on life/behavior leading to the client to seekservices;Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201735
Teaching SMHS Medical Necessity Sources of Info & Models: Important Area of LifeFunctioning3. BHS CANS/ANSA Items:a) CYF 0-4: Motor, Sensory, Developmental/Intellectual,Communication, Physical/Medical, Familyb) CYF 5-18: Family, Living Situation, Recreational,Developmental, Legal, Physical/Medical, Sexuality, SchoolBehavior, School Achievement, School Attendancec) A/OA: Physical/Medical, Family, Recreational, Living Skills,Employment, Transportation, Sexuality, Residential Stability,Legal, Self-Care, Social Functioning, IntellectualStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201736
Teaching SMHS Medical Necessity Sources of Info & Models: Important Area of LifeFunctioning4. 1994 Manual (Rehab Option & Targeted Case Mgmt):a. Community Functioning: (next page)ORb. Psychiatric Symptoms: the person exhibits repeated presenceof psychotic symptoms OR suicidal ideation or acts OR violentideation or acts to persons or property.ORc. Psychiatric History: the person has a psychiatric history ofrecurring substantial functional impairment or symptoms. Theperson's history demonstrates that without mental health service,there is a high risk of recurrence to a level of functionalimpairment/symptoms listed above.Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201737
Teaching SMHS Medical Necessity Sources of Info & Models: Important Area of LifeFunctioning [1994 Manual (Rehab Option & Targeted Case Mgmt)]:Community Functioning: reflects the degree in which a mental health illness disrupts or interfereswith community living to the extent that without treatment and/or services, the person would be unable tofunction:(a) Living arrangements: the person lives in the community in a setting of his/her choice; for children, they livein the home and comply with community rules(b) Daily Activities: the person is involved in a productive daily activities (may include involvement in householdchores, scheduled programs, education and training, and employment; for children, they are involved in ageappropriate daily activities (may include involvement in household chores, scheduled programs, education andtraining, and employment)(c) Social Relationships: the person demonstrates the ability to establish and maintain relationships and socialsupport systems; for children, they demonstrate the ability to establish and maintain relationships and socialsupport systems; for children, they demonstrate the ability to establish and maintain age appropriate social andfamily relationships(d) Health: individual demonstrates the ability to maintain physical and mental hygiene and manage ownmedications; for children, they experience maximum physical and mental well being, with symptoms minimized6/2/201738and good access to health care services.
Teaching SMHS Medical Necessity Tougher: Pathway #3/Probability of SignificantDeterioration in Life Functioning STANDARDIZING interpretation/charting: “Probability” The extent to which something is probable;the relative likelihood of an event happening or being thecase;“Deterioration” The process of becoming progressivelyworse; to make worse; a reduction in ability to perform up tothe anticipated standardStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201739
Teaching SMHS Medical Necessity Tougher: Pathway #3/Probability of SignificantDeterioration in Life Functioning STANDARDIZING interpretation/charting: “Significant Deterioration” An important and “real”(genuine, palpable, practical, noticeable) worsening/reductionthat impacts ability to perform up to the anticipated standard“Prevent” to keep from happening or arising; stop frombeing in a certain state; to deter or hinderStaff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)6/2/201740
Skills Development:Can You Teach Medical Necessity? Teaching Medical Necessity for SMHS: You are SPECIAL (“specialist vs. generalist”) LAWYERS wrote Title 9 (“flip into pictures & words”) FOUR special components (“not just any old ”) FOUR ways to qualify (“CA’s program is generous”)Staff Contact: Joseph A Turner, PhD (joe.turner@sfdph.org)41
Skills Development:Can You Teach Medical Necessity? Teaching Device #1: “Did you know you arespecial?” Goals: teach people the technical name for ourservices highlight the intense nature of our services Script:1. did you know you are special tell us what makes you special2. did you know you are special in our system3. you are special in our system because you provide specialtymental health services42
Skills Development:Can You Teach Medical Necessity? Teaching Device #1: Special One way to help people learn is “compare andcontrast” The opposite of “specialist” is “generalist” “General” health care services are provided in healthclinics—these are critically important services/staff, butthey are generalist services (e.g., diabetes meds) “General” mental health services are provided toclients whose impairments are mild/moderate43
Skills Development:Can You Teach Medical Necessity? Teaching Device #1: Special Another way to help people learn is to play on theirinterests (e.g., social justice; advocacy) “SMHS are special because they are funded withtaxpayer dollars and taxpayer dollars are veryspecial dollars—they are highly regulated andscrutinized (e.g., you cannot take taxpayer dollars andthen discriminate against people)”44
Skills Development:Can You Teach Medical Necessity? Teaching Device #2: “Lawyers wrote Title 9 Iflipped it into pictures and words” Goals: show Title 9 is a regulation and validatedifficulty understanding medical necessity, but that youhave done the heavy lifting for them. Script:1. I’m going to orient you to a document that teaches medicalnecessity. After I orient you to the document, I’ll explain it to you2. Page 1 just shows you the definition from Title 9. Page 2 takesthose words and represents them as pictures. Page 3 takes thosesame words and represents them as a table3. Some people learn better from pictures vs. words45
Skills Development:Can You Teach Medical Necessity? Teaching Device #2: Pictures & Words The pictorial representation helps us understand therelationship between impairments/interventions If client has “current/significant impairments,” theninterventions must “significantly reduce impairments” The tabular representation helps us understand thecommon elements Every pathway, including EPSDT, requires an includeddiagnosis!46
Skills Development:Can You Teach Medical Necessity? Teaching Device #3: “Four special elements inevery chart” Goals: emphasis on all charts will have fourelements and encourage staff to look for those.47
Skills Development:Can You Teach Medical Necessity? Teaching Device #3: FOUR SPECIALS Script:1.2.3.4.5.If you tell me your chart meets medical necessity, then I know I’mgoing to see 4 special things—follow along on Page 2 of thehandout and look at the 4 vertical blue bubblesThe first ‘special’ for medical necessity is a special diagnosis notany old diagnosis, but a special diagnosisThe second ‘special’ is a special impairment in functioning notany old impairment, but a special impairment in functioningThe third ‘special’ is the need for special interventions not any oldinterventions, but special interventions.The fourth ‘special’ is the need to be served in a specialtysetting not any old physical health care setting48
Skills Development:Can You Teach Medical Necessity? Teaching Device #3: FOUR SPECIALS One way to help people learn is the use of repetition Use rhythm, rhyme and inflection to help peopleremember (“ not any old diagnosis, but a ”)49
Skills Development:Can You Teach Medical Necessity? Teaching Device #4: “Four Ways to Qualify” Goals: teach people that there are multiple ways for aclient to meet medical necessity; show thatmaintenance is a valid pathway Script:1. Now that we know the 4 common elements, let’s walk though the 4different ways a client can qualify for medical necessity2. Look at page 2 of the handout (the picture) and follow along50
Skills Development:Can You Teach Medical Necessity? Teaching Device #4: “Four Ways to Qualify” Script (continued):3. Pathway 1 is “current significant impairment in functioning.” This is like your intake client who presents with a crisis/problem Usually clients come to services in some type of acute state. You know an acute client need a service today because they arehaving problems. I’m going to refer to this pathway as CURRENT/SIGNIFICANT,ACUTE/INTAKE, and TODAY.51
Skills Development:Can You Teach Medical Necessity? Teaching Device #4: “Four Ways to Qualify” Script (continued): If you argue that your client qualifies through the“current/significant/acute/today” thenyourprogress notes must show that yourinterventions are significantlyreducing the significantimpairment!52
Skills Development:Can You Teach Medical Necessity? Teaching Device #4: “Four Ways to Qualify” Script:4. Pathway 2 is “risk of significant deterioration.” This is like the client you’ve been seeing for a year who is morestableSpecialty mental health services have been to stabilize/improvethe client’s functioning, but yet you know they cannot maintainthose gainsWe can think about this as your maintenance client—you are tryingto help the client maintain their functioning.I will refer to this as “risk of decline,” maintenance and “tomorrow”(i.e., your client is doing ok today, but if you stop providing aservice, their functioning will decline TOMORROW.53
Skills Development:Can You Teach Medical Necessity? Teaching Device #4: “Four Ways to Qualify” Script (continued): If you argue that your client qualifies through the “risk of significantdecline/maintenance/tomorrow” thenyourprogress notes must show that yourinterventions are preventingsignificant decline!54
Skills Development:Can You Teach Medical Necessity? Teaching Device #4: “Four Ways to Qualify” Script:4. Pathway 3 is confusing and I’ve never seen it in p
CDIP CCR Title 9: a must-have reference for a true QA . Title 11: Law Title 24: Building Standards Code Title 12: Military & Veterans Affairs Title 25: Housing & Community Development Title 13: Motor Vehicles Title 26: Toxics Title 14: Natural Resources Title 27: Environmental Protection