Transcription
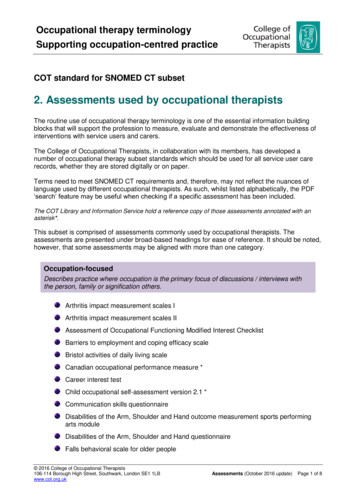
consultation with the specialistEncopresis: Assessment andManagementAlison Schonwald, MD,*Leonard Rappaport, MD, MS†Case IllustrationJake is an 8-year-old boy who has had stainson his underwear for 2 years. The historyincludes the passage of meconium withinhis first day after birth and loose stools during his toddler years despite efforts to limithis juice intake. He was toilet trained forurine at 21 2 years and for stool at 3 years; hehas passed stools regularly into the toilet from3 to 5 years of age.When he started kindergarten, Jake’sbowel habits became irregular. He began towithhold stool, so as not to defecate while atschool or to interrupt his play. Presently, Jakehas painful stools in the toilet once per week.Smears are found in his underwear mostdays, and sometimes small, hard balls of stoolare found on the floor. He hides his underwear frequently, and siblings tease him because of his odor. Jake complains of frequentstomachaches and has a poor appetite.His parents yell at him daily, tellinghim to go to the bathroom, but he says hedoesn’t “have to go.” His parents say they“don’t understand how he can walk aroundwith BMs in his pants all day” and that “itjust isn’t normal.” Jake avoids eye contact,appearing sad while his history is reviewed.Chart examination confirms that Jakewas a healthy term infant who had no medical diagnoses or surgeries. His growth parameters remain along the 75th percentilefor age. He is receiving no medications andtakes no over-the-counter or alternativetreatments. In kindergarten and firstgrade, teachers reported a high activitylevel and distractibility, and in first grade,his reading progressed slowly. Findings onphysical examination, including a detailed neurologic examination, are normal. Firm stool is palpated in his left lower*Developmental Medicine Center; Assistant inMedicine, Boston Children’s Hospital; Instructor inPediatrics, Harvard Medical School.†Director, Developmental Medicine Center; AssociateChief, Division of General Pediatrics, BostonChildren’s Hospital; Mary Deming Scott AssociateProfessor of Pediatrics, Harvard Medical School,Boston, MA.278 Pediatrics in Review Vol.25 No.8 August 2004quadrant, and bits of loose stool are notedperianally in association with stained underwear. Abdominal radiography shows alarge amount of granular stool dilating therectum and extending to the distal colon.DefinitionJake’s story is typical of a child whohas constipation and encopresis. Encopresis is defined as repeated passage of stool into inappropriateplaces by a child who is older than 4years of age chronologically and developmentally. The behavior is notdue exclusively to the direct physiologic effects of a substance (eg, laxatives) or a general medical condition,except through a mechanism involving constipation. Constipation is defined by the Academy of PediatricGastroenterologists and Nutritionists as delay or difficulty in defecationfor 2 or more weeks. The primarycare setting is the optimal place forlong-term treatment that addressesmedical and behavioral componentsof this common pediatric problem.Epidemiology andPathogenesis of EncopresisEncopresis reportedly affects 2.8% of4-year-olds, 1.9% of 6-year-olds, and1.6% of 10- to 11-year-olds. It usually presents in children younger than7 years of age. More than 90% ofencopresis is due to functional constipation where retained stool distends the rectum, resulting in stoolleaking around a stool mass (Figure).Stretch receptors in a distended rectum do not seem to signal the childto defecate until soiling is nearlycomplete. Encopresis generally is notcaused by underlying psychopathology, but it can be associated withemotional distress.Rare cases of encopresis are due to
consultation with the specialistFigure. Process and effects of encopresis. Reprinted with permission from Levine MD. Developmental and Behavioral Pediatrics.P. 419 3/e. 1999 with permission from Elsevier, Inc.damaged corticospinal pathways oranorectal dysfunction after pullthrough surgery. A small subset ofchildren who have encopresis maypass stool impulsively due to anxietyor other emotional stressors withoutunderlying constipation.Clinical Presentation andAssessmentA child who has functional constipation and consequent encopresis reports uncomfortable, often infrequent stooling into the toilet, withuncontrolled stool accidents into underwear or pull-up diapers. A detailed history and physical examination are required to rule out systemicor organic causes of constipation orincontinence, such as spinal cord dys-plasia, hypothyroidism, and meconium ileus of cystic fibrosis. For mostchildren, no further diagnostic assessment is necessary beyond thorough, directed fact finding.The history should begin withevents since birth, with specifics surrounding bowel function and anytreatments used. Past medical andsurgical history may identify systemicdiseases or medical causes of constipation that indicate treatments otherthan laxatives and maintenance of stoolregularity. For example, Hirschsprungdisease usually presents with difficultyin evacuation from birth, recurrent abdominal distension, or emesis. Failureto thrive and enterocolitis often occurin infancy. Encopresis is rare, and therectal examination findings include atight aganglionic bowel around the examining finger.It is essential to distinguish delayed toilet training, where the childnever consolidated the ability tostool independently into the toilet,from encopresis. Treatment varies,depending on whether constipationunderlies the stooling accidents,rather than toilet refusal, althoughtoilet refusal often is associated withconstipation. Developmental historyfocuses on details of toilet training,when and which methods were used,and any successes or failures. Mostchildren are toilet trained by 3 yearsof age in the United States. Childrenwho are not toilet trained until after4 years are outliers in this developmental trajectory.Pediatrics in Review Vol.25 No.8 August 2004 279
consultation with the specialistPoints to review include details ofpresent urinary and bowel patterns,such as frequency of stool evacuationinto the toilet, stool accidents, stoolconsistency, and the urge to defecate.More severe, prolonged constipationgenerally requires more aggressivetreatment. Any history of abuse orother trauma also should be sought.Children who have been abused maybecome incontinent in times of stressor as part of regressive behavior and areless suitable candidates for rectal suppositories or enemas.Urinary patterns, diurnal and nocturnal enuresis, and symptoms of urinary infection must be elicited andmay indicate neurologic abnormalities or consequent urine contamination. Constipation and encopresismay be associated with urine infections, especially in females, due topoor hygiene. Even without infection, enuresis can be caused by a dilated rectum pushing on and irritating the bladder, thus causing spasm.History may reveal that increasingstool backup is associated with urineaccidents. Charting calendars mayclarify such details.History taking provides an essential opportunity to communicatewith the child. The child must be aparticipant for treatment to be effective, and often affected children areoverwhelmed and embarrassed whenencopresis is discussed. Developing asense of the child’s perspective cancreate a connection between caregiver and patient and may be gainedwith questions about present schooland family functioning.The physical examination of thechild who has encopresis includes determination of growth parameters,attention to signs of systemic disease,careful neurologic assessment, andexamination of the anal opening.Anal fissures cause ongoing pain withdefecation, tags may reflect inflammatory bowel disease, and an absent280 Pediatrics in Review Vol.25 No.8 August 2004anal wink may indicate neurologicabnormality. An anteriorly placedanus may be associated with lifelongconstipation and deserves referral toa surgeon. Rectal examination can beuseful in assessing for Hirschsprungdisease and may indicate the degreeof rectal impaction, which can guidetreatment. Low anal pressure may reflect external or internal sphincterdisease. For most children, a rectalexamination performed with thechild lying on his or her back in amodified lithotomy position canminimize trauma.A rectal examination may not beappropriate for the first visit, particularly in a child who has a history ofsexual abuse or who is overwhelmedwith the discussion of this privateproblem. However, a digital examination should be performed at leastonce to rule out organic causes ofconstipation and to prescribe adequate treatment.Laboratory investigation is indicated only as history or physical examination suggests; rarely, laboratory studies may include thyroidfunction tests and measurement ofelectrolytes, calcium, and magnesium. An abdominal radiograph maybe useful when the history is vague orthe child is uncooperative with theexamination. Lumbosacral spinefilms or magnetic resonance imagingare indicated when results of thelower extremity neurologic examination are abnormal or sacral abnormalities are seen.quires treatment with lubrication before constipation can be addressed.A Cochrane Database SystematicReview in July 2001 found 16 randomized or quasi-randomized trialsof behavior or cognitive interventions (with or without other treatments) for the management of defecation disorders in children. A totalof 843 children were included in thetrials. Overall conclusions suggestedthat behavioral intervention plus laxative therapy, rather than either alone,improves fecal continence in childrenwho have encopresis. Biofeedback wasnot found to be effective.These findings support the efficacy of the treatment methods wehave employed for 25 years in theDevelopmental Medicine Center atBoston’s Children’s Hospital (Table1). There are several variations of themedications chosen and the order inwhich they are employed. The firsttwo steps occur at the initial visit; thethird step occurs after the clean-outstage.Mineral oil often is difficult to tolerate. We recommend keeping theoil cold and mixing it in a 1:1 ratiowith a fat-based substance that thechild enjoys, such as pudding, yogurt, or chocolate syrup. Mineral oilshould be avoided in children at riskfor aspiration. Some prescribe a multivitamin to prevent malabsorption offat-soluble vitamins, although the literature is inconsistent in supportingthis widespread practice.Management of EncopresisEncopresis WithoutConstipationA limited body of evidence-baseddata addresses the treatment of childhood encopresis. Management includes intensive medication and behavioral interventions and is adjustedto the child’s developmental stageand degree of constipation. Retention caused by painful fissures re-Treatment of encopresis that occurswithout constipation requires similarbehavioral approaches, but withoutconcomitant laxative therapy. Inthese cases, the index of suspicion fororganic pathology or abuse is considerably higher.
consultation with the specialistDevelopmental Medicine CenterProgram at Boston’s Children’s HospitalSchedule ofClean-outStep One: PsychoeducationDay 1: Bisacodyl pillDay 2: Bisacodyl suppositoryDate 3: Fleet姞 enemaRepeat three additional times over12 daysTable 1.Demystify the shame and blame around stool accidents Use the child’s abdominal radiograph or an illustrated explanation (or both)to review the process of retained stool that leads to a distended gut,allowing stool to “sneak out” without warning. Discuss that retained stool has to be cleaned out with medication (somechildren fear we mean surgery unless specified) and that there likely will bea lot of stool to clean out! Empathize with the stress and frustration and emphasize the need to breakthe cycle of impatience that may have developed. Clarify that now the childtruly cannot control the stool leaking out and cannot be blamed.Step Two: The Initial Clean-out of Retained StoolThe clean-out method depends on the age of the child, previous treatments,and history of trauma Children 7 years of age and older who have no history of trauma may optfor the fastest and most direct choice: a 14-day cycle of alternatingbisacodyl pills, bisacodyl suppository, and Fleet姞 enema (Table 2). Younger children ( 7 y) or those who cannot tolerate suppositories orenemas may require polyethylene glycol without electrolytes, starting at 1cap in 6 oz of fluid per day. Impaction that is present for many months mayrequire higher dosing or the addition of a stimulant such as senna orbisacodyl. During the initial clean-out, the child and family should expect a largeamount of stool output and should be reminded of the radiographdocumenting the bowel full of stool.Step Three: Establishing Regular Bowel PatternsMedication and a behavior plan We often use mineral oil titrated to efficacy, from 2 Tbsp per day to 6 Tbsptwice per day. Polyethylene glycol without electrolytes also is usedfrequently, particularly for children who do not tolerate the taste of mineraloil or who experience oil leakage. The maintenance dose of polyethyleneglycol without electrolytes generally ranges from 1/2 cap every day to 1 captwice per day. The dose is adjusted to maintain soft, regular stools. Because the child may not develop the urge to defecate for 6 to 9 monthsafter constipation is treated, a regular sitting time is necessary. The goal isto pass stool into the toilet before stool leaks. Sitting after breakfast anddinner takes advantage of the body’s gastrocolic reflex and often can beincorporated easily into the daily routine. We suggest sitting for 5 to10 minutes, depending on the child’s age and attention span. The family must work to eliminate any negative associations aroundtoileting that may have developed. Limiting conversation about toileting canbe helpful, as can rewarding the child for sitting or taking care of his or herown bodily needs. Older children may benefit from having games oractivitie
useful in assessing for Hirschsprung disease and may indicate the degree of rectal impaction, which can guide treatment. Low anal pressure may re-flect external or internal sphincter disease. For most children, a rectal examination performed with the child lying on his or her back in a modified lithotomy position can minimize trauma.