Transcription
Making Healthcare Whole: IntegratingSpirituality into Patient careChristina M. Puchalski, M.D.Director, GWishProfessor, Depts of Medicine and Health SciencesThe George Washington Institute for Spiritualityand Health (GWish)The George Washington University School ofMedicine and Health SciencesWashington, D.C.
Journey with people in vulnerable times intheir lives
3
What many patients face with seriousand chronic illness Suffering due to a person’s sense of independence anddignity being threatenedLoss of meaning; loss of a sense of personhoodDespair, demoralization, hopelessnessLiving with uncertainty (“mystery”)Increased likelihood of chronic conditionsActivity limiting conditions; pain other symptomsIncreased dependence of care from othersFinancial strain (medical expenses, not working)Social isolation; strain in relationships C.Puchalski
Primary Causes of Stress ForHealthcare Professional Work Place tensionCare of the Critically Ill and Dying Patients(Vachon, 2000)Focus on technology and curing rather thansupportive care and compassion (Puchalski, 2007)When demands from the work environmentexceed the employee’s ability to cope with (orcontrol) them, stress can result C.Puchalski
Religion, Spirituality and DepressiveSymptoms in Residents (Yi et al, 2004)Depressive symptoms highly prevalent inprimary care house officers Depression associated with poorer religiouscoping, and worse spiritual well-being What about other healthcare professionalsand the role of spirituality in their lives? C.Puchalski
Illness as Triggers for Questions about Life,Meaning, spiritual issues Illness/stress can cause us to question ourmeaning and purpose in lifeHealing is more than technical Integration of these questions intopatient’s life---new understanding of selfand situation. Finding hope, meaning and purpose Acceptance of situation C.Puchalski
TOTAL PAIN"I realized that we needed not only betterpain control but better overall care. Peopleneeded the space to be themselves. I coinedthe term 'total pain,' from my understandingthat dying people have physical, spiritual,psychological, and social pain that must betreated. " Cecily Saunders, MD (Smith, The WeeklyStandard, 2006) C.Puchalski
C.Puchalski
Biopsychosocialspiritual model Integrated; e.g. pain as multifactorial Physical, emotional, social and spiritual painAll dimensions treated equallyImplies team approach--different levels ofexpertiseRecognition of the whole person--does notobscure the humanity of each individualRespect for dignity and inherent value of eachhuman being. C.Puchalski
Spirituality/Religion associated with: Better healthcare outcomes (coping, will to live,increases survival in ESRD dialysis patients, recoveryfrom surgery, depression, increased hope, less deathanxiety). Effective additive over social support.Spirituality associated with greater quality of life withpatients with advanced disease if they have meaningand purpose, fulfillment in life goals (Cohen SR,Mount BM, et al., 1995)Lower stress-associated biological markers, changes inarea of brain associated with stress/emotionsResiliencyMind-Body interventions have positive benefits onhealth C.Puchalski
Spiritual History: A Patient Need Surveys: 50-85% want physicians to address patients’ spiritual needsand incorporate into treatmentWhy?: increases trust, helps MD understand patient more, helps MDwith treatment plan, patients feel listened to and cared for, helpsencourage realistic hope and provide compassionate care.When?: dying, just diagnosed with serious illness, suffering fromchronic illness, suffering from loss, admitted to a hospital , new historyand physicalMcCord et al. Annals of Family Med 2(4):2004 C.Puchalski
Guidelines for Spiritual Care:Improving the Quality of Spiritual Care as aDimension of Palliative Care:A Consensus Conference Convened February 2009Christina Puchalski, MD, MS, FACPBetty Ferrell, PhD, MA, FAAN, FPCN, RNSupported by the Archstone Foundation, Long Beach, CA. as a part of their End-of-Life Initiative.13
Background The goal of palliative care is toprevent and relieve suffering (NCP,2009)Palliative Care supports the bestpossible quality of life for patientsand their families (NCP, 2009)Palliative care is viewed asapplying to patients from the timeof diagnosis of serious illness todeath14
Consensus Conference Design and Organization 40 national leaders representingphysicians, nurses, psychologists, socialworkers, chaplains and clergy, otherspiritual care providers, and healthcareadministratorsDevelop a consensus-driven definition ofspiritualityIdentify points of agreementMake recommendations to improvespiritual care in palliative care settingsIdentify resources to advance the quality ofspiritual care 15
A Consensus Definition of Spirituality was Developed: “Spirituality is the aspect of humanity that refers to theway individuals seek and express meaning andpurpose and the way they experience theirconnectedness to the moment, to self, to others, tonature, and to the significant or sacred.”16
Conference Recommendations I.II.III.IV.V.VI.VII.Recommendations for improving spiritual care aredivided into seven keys areas:Spiritual Care ModelsSpiritual AssessmentSpiritual Treatment/Care PlansInterprofessional TeamTraining/CertificationPersonal and Professional DevelopmentQuality Improvement17
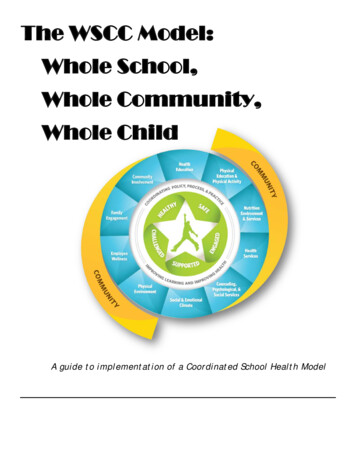
I. Spiritual Care ModelsRecommendations Integral to any patient-centered health caresystem Based on honoring dignity Spiritual distress treated the same as any othermedical problem Spirituality should be considered a “vital sign” Interdisciplinary18
Inpatient Spiritual Care Implementation Model19
II. Spiritual Assessment of Patients and Families RecommendationsSpiritual screening, historyAssessment toolsAll staff members should be trained to recognizespiritual distressHCP’s should incorporate spiritual screening andhistory as a part of routine history/evaluationFormal assessment by Board Certified ChaplainDocumentation of spiritual issues in chartFollow-up as with any other issue20
Spiritual History ComprehensiveDone in context of intake exam or during aparticular visit such as breaking bad news, end oflife issues, crisisDone by the clinician who is primarily responsiblefor providing direct care or referrals to specialistssuch as professional chaplains.Can be used to follow up on spiritual themes thatcome up in conversation with patients C.Puchalski21
Spiritual History F Do you have a spiritual belief? Faith? Do youhave spiritual beliefs that help you cope withstress/what you are going through/ in hardtimes? What gives your life meaning? I C Are you part of a spiritual or religiousAre these beliefs important to you? How dothey influence you in how you care for yourself?community? A How would you like your healthcare providerto address these issues with you? C.Puchalski22
A Consensus Definition of Spirituality was Developed: “Spirituality is the aspect of humanity that refers tothe way individuals seek and express meaning andpurpose and the way they experience theirconnectedness to the moment, to self, to others, tonature, and to the significant or sacred.” F: meaning, purpose, transcendence (sacred, God,significant, others, moment) .Inner LifeI: how this affects one's life, healthcare decisions,copingC: connectedness to others within a sacred, orsignificant context23
Validation (COH) Inter-item correlation between FICA quantitativeand COH spirituality domain of QOL instrument: ReligionActivitiesChange over timePurposeHopespiritual
Faith/Belief/Meaning Theme (n 73) Appreciation of life and familyLife activities work, purpose)Faith/Hope in healingRelationship with GodAppreciation for lifeReading BibleAgnosticPositive state of mindReligious affiliationPrayerFate in God’s HandsNature4731181275554444
Spiritual Diagnosis Decision Pathways26
Spiritual Assessment ExamplesDiagnoses (Primary)Key feature from historyExample StatementsExistentialLack of meaning / questions meaning about one’s ownexistence / Concern about afterlife / Questions themeaning of suffering / Seeks spiritual assistance“My life is meaningless”“I feel useless”Abandonment God or othersLack of love, loneliness / Not being remembered / NoSense of Relatedness“God has abandoned me”“No one comes by anymore”Anger at God or othersDisplaces anger toward religious representatives /Inability to ForgiveConcerns about relationship withDeityCloseness to God, deepening relationshipConflicted or challenged beliefsystemsVerbalizes inner conflicts or questions about beliefs orfaith Conflicts between religious beliefs andrecommended treatments / Questions moral or ethicalimplications of therapeutic regimen / Express concernwith life/death and/or belief systemDespair / HopelessnessHopelessness about future health, lifeDespair as absolute hopelessness, no hope for value in lifeGrief/lossGrief is the feeling and process associated with a loss ofperson, health, etcGuilt/shameGuilt is feeling that the person has done something wrongor evil; shame is a feeling that the person is bad or evil“I do not deserve to die pain-free”ReconciliationNeed for forgiveness and/or reconciliation of self orothersI need to be forgiven for what I didI would like my wife to forgive meIsolationFrom religious community or otherReligious specificRitual needs / Unable to practice in usual religiouspractices“I just can’t pray anymore”Religious / Spiritual StruggleLoss of faith and/or meaning / Religious or spiritualbeliefs and/or community not helping with coping“What if all that I believe is not true”“Why would God take my child its not fair”“I want to have a deeper relationship with God”“I am not sure if God is with me anymore”“Life is being cut short”“There is nothing left for me to live for”“I miss my loved one so much”“I wish I could run again”“Since moving to the assisted living I am not ableto go to my church anymore”
Action/address:Intervention – HCP / Pt. Communication Compassionate presenceReflective listening/query aboutimportant life eventsSupport patient sources ofspiritual strengthOpen ended questionsInquiry about spiritual beliefs,values and practicesLife review, listening to thepatient’s storyContinued presence and follow up28
Intervention – Simple Spiritual Therapy Referral to spiritual careprovider as indicated (BCC,pastoral counselor, spiritualdirector, culturally basedhealerSpiritual GoalsGuided visualizationProgressive relaxationBreath practice orcontemplationMeaning-oriented-therapyNarrative MedicineDignity-conserving therapy29
Intervention – Patient Self-Care Reconciliation with self and/or othersJoin spiritual support groupsMeditationReligious or sacred spiritual readingsor ritualsBooksYoga, Tai ChiExerciseEngage in the arts (music, art, danceincluding therapy, classes etc)JournalingReflective practices30
III. Formulation of a Spiritual Treatment Care Plan RecommendationsScreen & AccessAll HCPs should do spiritual screeningClinicians who refer should do spiritual histories anddevelop appropriate treatment plans working withBoard Certified Chaplain if possibleDiagnostic labels/codesTreatment plansSupport/encourage in expression of needs and beliefs31
III. Formulation of a Spiritual Treatment Plan (cont’d) Spiritual care referral (BCC, pastoral counselor, spiritual director, clergy asappropriate) Documentation of spiritual support resources Follow up evaluations Treatment algorithms Discharge plans of care Bereavement care Establish procedure32
Narrative: Hopelessness Ronda is a 52 yo female with end-stageovarian cancer. Seven-and-a-half yearsafter the multiple surgeries andchemotherapy, with good outcomes, she isnow faced with advanced disease forwhich there is no longer any treatment.Her hope has always been for a cure. Nowshe faces a deep sense of hopelessness. C.Puchalski33
Spiritual History F: Raised Jewish culturally; meaning hasalways been in nature and not religionI: Spirituality is important, nature calmsher,worried about how she can do thatnowC: Friends and family are her supportA: now that she is dying she would like toknow how Judaism views dying andwhat rituals might help her C.Puchalski34
Narrative example: Biopsychosocial-Spiritual ModelAssessment and PlanRonda is a 52 yo with end stage ovarian ca . Assessment reveals:PhysicalPain is well controlled; continue with current medication regimen.Nausea; still has episodes of nausea and vomiting, likely secondary topartial sm bowel obstruction (SBO). Add octreotide to current regimenEmotionalGrief rxn that “fight is over”.Tearful, difficulty sleepingSocialRonda concerned abot how to tell them she is dying.Supportive counseling, presence.Work with social work to arrange family meetingSpiritualHopelessness, main source of meaning in “winning the fight”, active in ovcancer alliance and seen as inspiration. Not religious but now wants tolearn how “Jewish Patients die?”Dream List, legacy building, encourage talking with Ov Cancer Alliance,referral to chaplain and to Rabbi
Interventions by the Team Help patient create a dream listTalk about all relationships in theperson’s life, including God if that isimportant. Any conflicts?What are her sources of hope?What has she learned of hope from herreligion? From other things? C.Puchalski36
Ronda’s Spiritual Assessment with Chaplain What was her upbringing from a Jewishperspective?What is her experience of ritual?Why did she leave her Jewish practice?What does it mean to her to be a “goodJew”What is her belief in an afterlife? C.Puchalski37
Conclusion Spiritual care is essential to improving qualitycare Studies have indicated the strong desire ofpatients to have spirituality included in their careand have suggested positive health outcomes38
Conclusion (cont’d) Interprofessional care should include board-certified chaplainson the care team Regular ongoing screening and assessment of patients’spiritual issues Integration of patient spirituality into the treatment plan withappropriate follow-up with ongoing quality improvement Professional education and development of programs Adoption of these recommendations into clinical site policieswith accountability measures39
SPRITUAL CAREDEMONSTRATION PROJECTS(OCT 2010-SEPT 2012) 9 Competitively Selected Southern California HospitalsFour Target AreasConference calls (1x/month)Convening meeting (2x/year)MentoringExternal evaluationDocument models and advance best care practices
California Hospital Sites Cedars SinaiCity of HopeKeck LAC USC Medical CenterPalomar PomeradoScripps MemorialSt Joseph’s Hospital, Orange CountySt John’s Regional Medical CenterUCLA Santa MonicaVeteran’s Hospital West LA
Four Target AreasFour Target Areas for Projects Spiritual Care Models Spiritual Assessment of Patients and Families Spiritual Treatment Plan Quality Improvement
Evaluation and Metrics Process evaluation (#patients receivingspiritual history, screening, assessment)Chart review of spirituality integrated intotreatment plan# chaplain referralsPatient satisfaction with care, spiritualneeds met
SummaryOur hope is that these demonstration projectswill serve as a model for others to improvespiritual care for patients.
GWish: www.gwish.org Education resources (SOERCE, National Competenciesetc)Interprofessional Initiative In Spirituality Education(nursing, medicine, social work, pharm, psychology)Retreats in for Healthcare Professionals (Assisi, US) August 2009, 2010 Assisi, ItalyTime for Listening and Caring: Oxford University PressMaking Healthcare Whole, Templeton PressFICA Assessment tool--- online DVDSummer Institute in spirituality and health at GWU.June 2011InspirChristina Puchalski, MD 202-994-6220 hcscmp@gwumc.edu cpuchalski
purpose and the way they experience their connectedness to the moment, to self, to others, to nature, and to the significant or sacred." F: meaning, purpose, transcendence (sacred, God, significant, others, moment) .Inner Life I: how this affects one's life, healthcare decisions, coping C: connectedness to others within a sacred, or