Transcription
Rachel Abrams, M.A.Pat Penn, Ph.D.Michael (member)La Frontera Arizona, Tucson, AZ
BackgroundCognitive-Behavioral Model of AddictionRelapse PreventionMindfulnessMindfulness & AddictionMBRP: Mindfulness-Based Relapse PreventionDefining MBRPResearch supportGoals & Central ComponentsImplementationOur MBRP studyOur experience with implementation and evaluationImplementation suggestionsMember experiences with MBRPExperiential exercisesSummary, Questions & Comments
Participants will be able to:1) Explain the theory and related goals of MBRP2) Describe MBRP and its main components3) Learn and practice two interventions from MBRP
Substance use disorders are often described as “chronic relapsingconditions,” with relapse rates over 60%.The most commonly available treatments and mutual support groups are12-step.As an alternative to 12-step programs, Relapse Prevention, and othercognitive-behavioral treatments (CBT), focus on responses to high-risksituations, combining skills-training with cognitive interventions.
Is based on the premise that maladaptive drinking and drug use arelearned behaviors.CBT provides a framework around which interventions attempt toidentify situational, social, affective, and cognitive precipitants ofpathological substance use.Once possible causes of maladaptive behavior are identified, anindividual may decide to learn to abstain from alcohol and drugs.
Does CBT really work in substance abuse treatment?You bet!Numerous studies have described the clinical and cost-effectiveness ofCBT in promotion of abstinence and in the reduction of drinkingquantity, frequency, and duration.(Carroll, 1996; Finney & Monahan, 1996; Irvin, Bowers, Dunn, & Wang, 1999; Kadden, 2001; Longabaugh & Morganstern, 1999).
As proposed by Marlatt and colleagues (Lariner, Palmer, & Marlatt, 1999; Marlatt & Gordon, Decreasedprobability ofrelapseHigh f-efficacy positiveoutcomeexperienceInitial use ofsubstanceAbstinenceviolationeffect perceivedeffects ofsubstanceIncreasedprobability ofrelapse
Summarizing this model: if an effective coping strategy is used,then the individual will likely experience an increase in selfefficacy and is less likely to consume the previously desiredsubstance.However, if an ineffective coping strategy is used, then selfefficacy may decline and/or expecting a positive outcomeincreases, leading to an increased likelihood of consumption.
Now let’s explore what Relapse Prevention is But first, what are your thoughts?
Is an intervention that attempts to describe, understand,prevent, and manage relapseFor individuals who have received, or are receiving,treatment for substance use disorders.
Begins with an assessment of triggers.Identify high-risk situations (the client’s perception of risk).A high-risk situation: any situation that poses a threat toone’s sense of perceived control (self-efficacy) and increasesthe risk of potential relapse.CBT approaches are then implemented (interpersonal &intrapersonal); self-management strategies.
Overall, the results show that although RP does not result inhigher abstinence rates following treatment,RP does significantly reduce the frequency and intensity ofrelapse episodes, helping people get “back on track” more quicklyif they do fall off the wagon.
Mindfulness and how it may be incorporated in thetreatment of substance use disorders.Your thoughts:What is mindfulness?How is mindfulness beneficial?What does it mean to be mindful?How might mindfulness be beneficial to individualssuffering from substance disorders?
“One of the most significant effects of regularmeditation practice is the development of mindfulness the capacity to observe the ongoing process ofexperience without becoming ‘attached’ oridentifying with the content of each thought,feeling, or image.”As stated in Relapse Prevention (Marlatt & Gordon, 1995).
Mindfulness, as illuminated by the quote by Viktor Frankl (1946)“Between stimulus and response, there is a space. In that spaceis our power to choose our response. In our responselies our growth and freedom.”Mindfulness practices increase awareness of this space andcreate the opportunity to respond skillfully rather than reactingautomatically and habitually.
Mindfulness has been described as “paying attention in a particularway: on purpose, in the present moment, and non-judgmentally.”Mindfulness may enhance the ability to cope with triggers byinterrupting the previous cycle of automatic substance use behavior.Mindfulness mediation provides heightened awareness and acceptanceof habitual responses without judging, analyzing, or reacting.(Bowen, Witkiewitz, Dillworth, Chawla, Simpson, Ostafin, Larimer, Blume, Parks & Marlatt, 2006; Breslin, Zack, & McMain, 2002; Davis,Flemming, Bonus & Baker, 2007; Marlatt, 2002; Roth & Creasor, 1997; Kabat-Zinn, 1994).
Neurobiological findings support the hypothesis that mediation and/ormindfulness exercises enhance awareness and the cultivation ofalternatives to compulsive behavior (Marlatt, 2002).Mindfulness may aid in the minimization of blame, guilt, and negativethinking that often increase risk of relapse.“In the context of addictions, mindfulness might mean becomingaware of triggers for craving and choosing to do something elsethat might prevent craving, therefore weakening the habitualresponse” (Groves & Farmer, p.189, 1994).
Mindfulness can provide a “skillful means” of copingwith urges and cravings that involves observing themwith kindness and flexibility, thus preventing beingconsumed by them.
Please get in a comfortable sitting position“Sitting Meditation”
Now, let’s at look at MBRP specifically - Research, Goals & Central Components
Until his death in 2011, he was the director ofthe Addictive Behaviors Research Center andProfessional of Psychology at the Universityof Washington.“By moving from aversion to acceptance as a means of coping withcraving, recovery is facilitated on the basis of a new compassionateapproach, which is what we hope to offer in the MPRP program”(G. Alan Marlatt).
Integrating over 2 decades of research with CBT based RP with existingmindfulness-based techniques, Marlatt and colleagues developed a“new” cognitive-behavioral intervention for substance use disorders,called mindfulness-based relapse prevention (MBRP).The goal of this relapse prevention:to develop awareness and acceptance of thoughts, feelings, andsensations through practicing mindfulness.to utilize mindfulness skills as an effective coping strategy in the faceof high-risk situations.
Populations tested:Adults in outpatient treatment for substance abuseAdults with substance use disorders who recentlycompleted intensive inpatient or outpatient treatmentIncarcerated adults with a history of substance abuseIndividuals with substance use disorders of various agesand ethnicities after intensive stabilizationUndergraduate smokers
Teach mindfulness awareness to clients suffering from addiction.Foster increased awareness of triggers and habitual responses.Cultivate the ability to pause and observe the present moment, in orderto make more skillful decisions.Ultimately, working toward freedom from deeply engrained and oftencatastrophic habitual patterns of thought and behavior.
When faced with a trigger for substance use, one can makea mindful choice that decreases the likelihood of relapse.Seeing the “big picture” provides a greater sense of freedomand choice.A mindful approach helps reduce the tendency of the mindto increase negative emotional states by lowering thestigma, shame, blame, and guilt commonly experienced bypeople who struggle with addiction.
The identification of high-risk situations for relapse isa central component of the treatment.Client’s are taught to observe pleasant and unpleasantsensations, thoughts or feelings, and they are encouragedto accept them without judgment.
A major element of the mindfulness training involvesteaching people to direct their attention to the breathin order to calm and focus the mind.
Challenging “positive outcome expectancies” andeducating about the “abstinence violation effect” are amajor focus of the treatment.Maintain focus and awareness on the present moment.Not living toward, or making decisions based on, futureevents (i.e. euphoria, numbing).
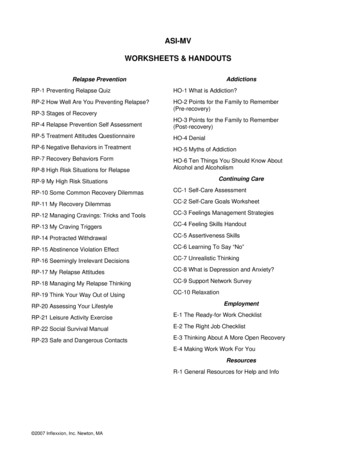
IntroductionPart I. Conducting MBRPPart II. Facilitator’s GuideSession 1: Automatic Pilot & RelapseSession 2: Awareness of Triggers & CravingsSession 3: Mindfulness in Daily LifeSession 4: Mindfulness in High-Risk SituationSession 5: Acceptance & Skillful ActionSession 6: Seeing Thoughts as ThoughtsSession 7: Self-Care & Lifestyle BalanceSession 8: Social Support & ContinuingPractice
Style & Structure:Session agendas including practices, worksheets, and handouts.Because investigation and trust of one’s own experience isencouraged, the core principles of MBRP:are elicited from participants whenever possibleare explored through experiential practices and inquiry
Inquiry:Sessions begin with experiential exercises, followed by a briefdiscussion or “inquiry.”Discussions centered on the clients’ present experience.Ensure that the inquiry sessions are redirected to involve discussionaround describing the immediate experience in the present moment(i.e. sensations in the body, thoughts, or emotions) versus theinterpretation, analysis, or story about the experience.
The observation of direct experience is the primaryintentionParticipants learn to recognize when they are caught instoriesThey realize that they have the choice to pause andreturn to present experience.
Home Practice:Is assigned each weekEach session includes a review of the previous week’s practices.Encourage, but be careful not to provoke self-blame orjudgment.Discuss struggles with lightness, compassion, and curiosity.
Michael’s ExperienceWith MBRP
Adapted MBRP to one of our settingsUsed evaluation methods and instrumentsQuestion: Why bother with Evaluation?
Traditional MBRPAftercare program2-2.5 hour group 1x weeklyIdeal group size 6 to 12.Closed groupHome practice essentialHome practice with CDsAssessment battery given at baseline,immediately following the 8-weekintervention period, and 2 & 4 monthspost-intervention.Assessments: The Timeline Followback(TLFB), The Penn Alcohol Craving Scale(PACS), Alcohol & Drug UseConsequences/Short Inventory ofProblems (SIP-AD), The Five FactorMindfulness Questionnaire (FFMQ).Our Study6mo residential drug/alcohol tx1 hour group 1x weeklyGroup size ranged 9 to 11Rolling enrollment groupHome practice encouraged, but unableto monitorClients did not have opportunity/meansto listen to CDs in room.Assessment battery given at baseline,immediately following interventionweeks 4 and 8.Assessments: FFMQ, PACS, and theDrug Avoidance Self-Efficacy Scale(DASES).
FFMQ: Five Facet Mindfulness QuestionnaireA reliable and valid comprehensive instrument for assessingdifferent aspects of mindfulness in community and studentsamples.Subscales (39 items total):ObservingDescribingActing with AwarenessNon-judgingNon-reacting
Please rate each of the following statements using the scale provided. Write thenumber in the blank that best describes your own opinion of what is generallytrue for you.12Never truerarely true3sometimes true4often true5very often or always true1. When I’m walking, I deliberately notice the sensations of my bodymoving.2. I’m good at finding words to describe my feelings.3. I criticize myself for having irrational or inappropriate emotions.4. I perceive my feelings and emotions without having to react to them.5. When I do things, my mind wanders off and I’m easily distracted.
PACS: Penn Alcohol Craving ScaleA five-item self-report measure with questions about:the frequency, intensity, and duration of cravingthe ability to resist drinkingan overall rating of craving for alcohol for the previousweekQuestions scaled from 0 to 6Flannery, B.A., Volpicelli, J.R. & Pettinati, H.M. (1999). Psychometric properties of the Penn Alcohol Craving Scale.
DASES: Drug & Alcohol Self-Efficacy ScaleA 16-item self-report questionnaireClients are asked to imagine themselves in a particularsituation and to rate their level of confidence (selfefficacy) to resist drug use in that situation.Each of the items represents a different situation inwhich a drug abuser might be tempted to use.Responses are rated on a 7-point scale ranging from"certainly yes" to "certainly no" which corresponds to ameasure of "strength" of self-efficacy.
Assessment times:(1) pre treatment/beginning of session 1(2) end of week 4(3) post treatment - at the conclusion of session 8The graphs on the following slides are as follows:PENNDASESFFMQ Total Scores
Cravings353030Total Score2529HS23MH20JJAD1511119106551102012 Assessments350DBCBTB
Self-Efficacy6664646362Degree of H5150ADDB48CB46TB4444424012Assessments3
Total ScoreFFMQ 24MH12Assessments3
Open groupInability to accurately monitor and/or utilize home practiceassignments (i.e. CDs)SettingNot every participant had a desire to learn/utilize the methodGroup limited to one hourVarying length of sobriety (i.e. time in treatment)Incomplete FFMQ’s: lesson learned!We would use the measures again – relevant and feasible
Group time: 1.5 hours for community treatmentClient choice to participateClosed groupCheck completed assessmentsFacilitators: be trained and confident with mindfulnesstechniquesFacilitators need to ensure that the “inquiry” process staysfocused on present experienceEnsure non-judgment of such experience (i.e. compassionate andgentle approach)Evaluate your adaptations!
“Jane’s” ExperienceWith MBRP
Please again get in a comfortable sitting positionThese two short mindfulness mediations are two of the keymediations that participants learn to utilize in MBRP.a) SOBER Breathing Spaceb) Urge Surfing
1) Develop awareness of personal triggers and habitual reactions,and learn ways find the space in this automatic process.2) Change relationship to discomfort through learning how torecognize challenging emotions and physical experiences, andrespond to them in skillful ways.3) Foster a nonjudgmental and compassionate approach towardourselves and our experiences.4) Build a lifestyle that supports both mindfulness practice andrecovery.
www.mindfulrp.comResearch summariesTrainingsMBRP tapes: Feel free to download these MP3s of practices usedin MBRP for your personal use or to share with clients.Body ScanSOBER SpaceUrge SurfingSitting Meditation (female voice)Sitting Meditation (male voice)Longer Sitting MeditationMindful Movement
Thank you for your time!Questions?Comments?
mindfulness-based techniques, Marlatt and colleagues developed a “new”cognitive-behavioral intervention for substance use disorders, called mindfulness-based relapse prevention (MBRP). yThe goal of this relapse prevention: yto develop awareness and acceptance of thoughts, feelings, and se