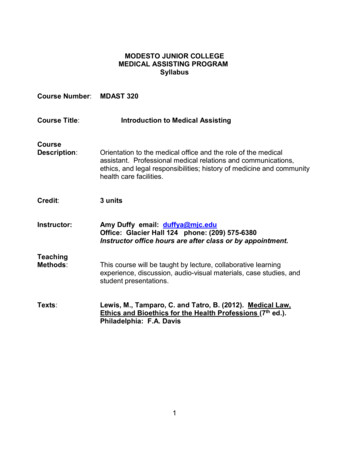
Transcription
OSCE Stationsfor Medical FinalsBook 1Adam Feather FRCPSenior Lecturer in Medical Education,St. Bartholomew’s and The London Medical School,Consultant GeriatricianNewham University Hospital NHS TrustAshling Lillis BA (Cantab) MB BS MRCP(UK)Acute Medicine Registrar,King George Hospital,EssexTony Joy MBChB MRCS(Eng) DCH‘Darzi’ Fellow in Clinical LeadershipRegistrar in Emergency MedicineNorth East Thames RotationLondonJohn S P Lumley MS FRCSEmeritus Professor of Vascular Surgery,St Bartholomew’s and the Royal LondonSchool of Medicine and Dentistry
ContentsAbout the AuthorsPrefaceAcknowledgementsHow to Use This BookIntroductory ChapterSCENARIOS1.What a wheeze2.Heartache3.Tummy pain4.Party girl5.Diarrhoea and vomiting6.Washed out and totally drained7.Breathless patient8.Cold feet9.Feeling awful10.Tingle in my fingers11.Confused young man12.Out of breath13.Funny turns14.Fallen Community leader15.Off legs16.All of a sudden17.Couldn’t get up18.Heart’s a flutter19.Don’t sweat it20.Unsteady on my feetBlank ChartsStation IndexSubject 239262286304318338353368374376v
SCENARIO 1Scenario 1:‘What a wheeze’Station 1History10-minute stationYou are the FY1 doctor on call for the Medical Team in the Emergency Department.Miss Sarah Davis has presented to the hospital with increasing shortness of breath.She is known to have asthma and has been admitted under the Respiratory Teambefore. You have been called to the ‘majors’ assessment area of the Emergency Departmentto take a history of both her present illness and her asthma history and presentyour history to the Respiratory Registrar on call.You will be assessed on the following areas, as well as the content and diagnosticreasoning of your history – take them into account in your presentation.Professionalismt t t t t Professional appearance (NHS dress code) – including general appearance, hair and jewelleryMaintains patient and personal safetyPolite introduction; identifies patient or interviewee correctly; confirms patient’s date of birth fromname band or other sourceObtains informal consent; maintains patient’s privacyDisplays empathetic and caring attitudes and behaviours throughout.Processt t t t Good organisation and structure; appropriate use of open and closed questionsAppropriate fluency/rhythm/pace to the interview – this may change depending on environmentand acute nature of the problemAppropriate time for the patient to respond/reply to questionsAppropriate acknowledgement of difficult or emotional areas of the patient’s history.Communication skillst t t t Demonstrates caring and sympathetic attitudeAsks open questionsInvites patient to ask questions and answers them appropriatelyAddresses patient’s ideas, concerns and expectations.1
W H AT A W H E E Z ESCENARIO 1Station 2Examination10-minute stationMiss Davis has an RR of 25 and O2 sats of 95% on room air. She has had one dose ofnebulised salbutamol in the Emergency Department but remains tachypnoeic. She hasbeen transferred to the resuscitation area of the Emergency Department. Please perform a focused respiratory examination of Miss Davis and present thisto your Registrar.You will be assessed on the following areas, as well as the content and skills of yourexamination – take them into account in your presentation.Professionalismt t t t t Professional appearance; maintains infection control standards, including hand cleaning andappropriate use of gloves and apronsMaintains patient and personal safetyPolite introduction; identifies patient and confirms date of birth from name band or other sourceObtains informal consent; maintains patient privacy and dignityDisplays empathetic and caring attitudes and behaviours throughout.Processt t t t Appropriate fluency/rhythm/pace to the examination – this may change depending on environmentand acute nature of the problemGood organisation and structure of examination; sensitive and empathetic approachUses appropriate clinical techniques throughoutMaintains privacy and dignity throughout.Clinical communicationt t t t 2Explains proposed examination/procedure; explains examination/procedure as it proceedsOffers information in a clear, structured and fluent manner, avoiding jargonListens to patient and responds appropriatelyDemonstrates appropriate body language.
W H AT A W H E E Z ESCENARIO 1Please read the information below before presenting this case to theST3 Medical Registrar as if you were on a busy medical take.[NB If you have a model do not read this section]Clinical findingso Patient appears dyspnoeic at rest, and unable to complete sentenceso RR 24 breaths per minute, O2 sats 95% room air 100% on 15 O2 l/min, BP 130/75o GCS 15o PEFR 350 (65% expected)o Peripheral capillary refill time 2 s; Pulse regular in rhythm; Carotid pulsenormal in volume; JVP not elevated; Apex beat not displacedo CV examinations – heart sounds easily heard, normalo RS examination – trachea central, no chest scars, chest expansion normaland equal bilaterally, widespread expiratory wheeze throughout both lungfields, normal percussion note throughout and breath sounds audiblein all areas.Station 3Procedural skills10-minute stationProcedureYou have moved your patient to the monitored bay of the Medical Admissions Unitand while your nurse colleague is inserting an IV cannula you have been asked toadminister a nebulised dose of salbutamol. Please demonstrate how you would set up and apply the nebuliser to the patient.Equipment providedx A selection of oxygen masks and nebulisersx Oxygen supply with variable deliveryx Patient (either dummy or volunteer)x Vials of salbutamol for nebulisation3
W H AT A W H E E Z ESCENARIO 1Station 4Data interpretation10-minute stationAs a training exercise the registrar on the team has asked you to review Miss Davies’sprevious lung function tests and compare them to those of some other patients on therespiratory ward.Patient A27-year-old woman with rheumatoid arthritis now presenting with a 6-monthhistory of shortness of breath; FEV1: 3.0; O2 sats on air: 92%; FVC: 3.8; transfercoefficient: grossly reduced.Patient B69-year-old man with 2-year history of exertional dyspnoea and an episodiccough; FEV1: 2.5; O2 sats on air: 89%; FVC: 3.7; transfer coefficient: reduced.Patient C22-year-old woman with 2-month history of worsening shortness of breath andfatigue on exertion and repetitive movement; FEV1: 3.7; O2 sats on air: 95%;FVC: 6; transfer coefficient: normal.Patient D23-year-old woman with 18-month history of nocturnal cough and wheeze;FEV1: 3.0; O2 sats on air: 97%; FVC: 3.5; Transfer coefficient: normal; no increasein FEV1 with nebulised B agonist.Which of patients A, B, C, D:1 Demonstrates a restrictive lung defect?2 Demonstrates an obstructive lung defect?3 Has type I respiratory failure?4 Typically demonstrates type II respiratory failure?5 Should be treated with nebulisers?6 Is most likely to have a thymoma?7 Is most likely to have an associated primary lung cancer?8 Classically worsens their hypoxia with exertion?9 May benefit from steroid therapy?10 May derive benefit from other forms of immunosuppression?4
SCENARIO 1W H AT A W H E E Z EStation 5Prescribing skills10-minute stationYour registrar has now asked you to prescribe appropriate medications to treatMiss Davis’s asthma exacerbation.DetailsMiss Sarah Davis; DOB: 24/11/1988; No known allergies; Weight: 64 kg; Ward:MAU; Consultant: Dr BeadleBlood resultsFBC: Hb 14.4 g/dl, MCV 90 fl, WCC 13.9 109/l, neutrophils 12.4 109/l, platelets122 109/lU&Es: Na 139 mmol/l, K 3.4 mmol/l, urea 4.6 mmol/l, creatinine 73 Pmol/lRBG: 5.2 mmol/lCCa2 2.23 mol/l, PO4- 0.78 mmol/l, Mg 1.02 mmol/lCXR: no pneumothorax, no focal consolidation.ECG sinus tachycardiaManagement – prescribing taskPlease prescribe the following therapeutic interventions using the charts (page 368)and the BNF emember: DRUG DRs Don’t Forget Signing Off (page 373)Station 6Communication skills10-minute stationMiss Davis has been on inhaled therapy on the ward for 24 hours and her PEFR isnow 500 l/min (best 550). Your consultant has asked you to have a discussion with herabout her asthma control. Discuss any changes in her lifestyle that may help with hercontrol.5
W H AT A W H E E Z ESCENARIO 1AnswersStation 1 – HistoryPatient scriptYou are 23 years old and have been asthmatic since the age of 14. Your asthma isnot well controlled and have had at least one to two admissions a year since then.The last admission was 3 months ago, when you were ventilated in intensive care.You have been previously ventilated three times. You are a current smoker of fiveto ten cigarettes a day and have to use inhalers three to four times a day. Yourcurrent medication is beclometasone and salbutamol inhalers. You have had sixcourses of steroids in the last 12 months.You take inhalers when you are wheezy rather than every morning and night. Yournormal PEFR when well is 550 l/min. You regularly wake up coughing during thenight and have often missed days at work because you are very wheezy; you gaveup your job in a supermarket after your last admission.The present illness started 5 days ago with a slight head cold followed by a coughproductive of green sputum and you are short of breath and wheezy, particularlyat night. You feel exhausted, like before you were ventilated the last time. You havehad a fever but have not noticed any blood in your sputum or chest pain.You have no pets and do not know of anything specifically that exacerbates yourasthma. You did not have hay fever or eczema as a child and you don’t know anyother family members who have eczema, asthma or hay fever. You live in a flatwith your four siblings and your parents.You are worried because you do not want to be admitted and would rather gohome. You are very scared of being ventilated again.6
A B C D EA B C D EA B C D O 1W H AT A W H E E Z EA B C D EIdentifies key informationt Presence of wheeze, increased shortness of breath and decreased exercise tolerancet Presence of infective symptoms – fever, coryza, thick green sputumIdentifies key information from rest of historyHistory of chronic asthmat Time of diagnosist Current treatment regime – inhaled steroid and PRN ß2-agonistt Peak flow at bestt Current control – any interference with sleep, frequency of exacerbationst Previous admissions to hospital; exacerbation requiring high dependency or intensivecare – intubated 3 months agoIncludes important negatives including systemic enquiryt Absence of chest pain and haemoptysisRelevant factors from employment, housing, social supportt Unable to work due to poor control, lives in a small flat with a number of family memberst No environmental triggers identifiedPrevious medical historyt Atopy history – no eczema, no hay fever or allergic rhinitisSocial and occupational historyt Smoker, 5–10 per dayt No petsDrug and allergic historyt Inhalers (as above), no allergiesNo relevant family historyt No family history of asthma or eczemaSummarises important areas of the history back to the patientInvites patient to ask questions and deals with them appropriatelyEstablishes patient’s ideas, concerns and expectationst Identifies that patient is concerned about being admitted to hospital and is worried thatshe may be admitted to intensive care once againAppropriately explains to patient that she is likely to be admitted to the hospital andreassures her that treatment of her exacerbation is the priority7
W H AT A W H E E Z ESCENARIO 1DIAGNOSTIC REASONINGA B C D EPlease present your historyCandidate offers a logical, well-structured account of the history What is your diagnosis?t Candidate offers the correct diagnosis and appropriate differentialst Diagnosis: this an exacerbation of asthma with a probable infective trigger, as thepatient’s symptoms include a cough productive of green sputum and fever. How would you describe her current control of her chronic asthma?t This patient obviously has very poor control of her asthma with frequent severeexacerbations. Previous admission to intensive care requiring intubation and ventilationis a key point to elicit from the history, as this will guide you to treat and monitor thispatient very closely. What are the key aspects to obtain in any chronic disease history?t Time of diagnosist Current treatment regime and contact with specialist servicest Frequency of admissions and severity of exacerbationst Functional ability at best and at worstt Interference with activities of daily living (and sleep in the case of asthma, as nocturnalcough can be extremely disruptive)t Patient’s understanding of her diagnosis.GLOBAL HISTORY MARKA B C D E8
SCENARIO 1W H AT A W H E E Z EStation 2 – ExaminationPatient scriptIf you are an actor/patient, read the patient history and physical signs fully – whenthe candidate comes to an abnormal site in their examination, act-out tendernessand/or volunteer the relevant physical sign.A B C D EA B C D EA B C D EPROFESSIONALISMPROCESSCOMMUNICATIONCONTENTA B C D EExposes and positions patient correctly and maintains comfortt Exposes chest and ensures monitoring and oxygen are appliedComments on wellbeing of patientt Patient appears short of breath at restt Only able to complete short sentencest Not using accessory muscle of respirationAsks for appropriate relevant clinical observationst Tachypneoic at 24 breaths per minute, O2 sats 95% room air 100% on 15 l/min O2t BP 130/75, capillary refill 2 s, GCS 15Focused examinationt Inspection – no scars on chestt Palpation – chest expansion normal and equal bilaterally; trachea centralt Percussion – normal percussion note in all zonest Auscultation – polyphonic expiratory wheeze throughout both lung fieldsCompletes examination by identifying relevant additional clinical signsCompletes examination by assessing PEFR: 350 (65% best)Thanks patient, offers assistance, maintains patient’s dignity and privacy until they aredressed9
W H AT A W H E E Z ESCENARIO 1DIAGNOSTIC REASONINGA B C D EIdentifies correct physical signs, including important negative findings; does not identifysigns that are not present.Demonstrates a safe and sensible management plan.t Place patient in an area where they can be monitored closelyt Apply oxygen via a reservoir mask at 15 l oxygen per minutet Give nebulised B-agonist (salbutamol)t Establish IV access.GLOBAL EXAMINATION MARKA B C D EStation 3 – Procedural skillsNEBULISER ADMINISTRATIONExposes and positions patient correctly and maintains comfortt Patient sat up at 45 degrees to optimised inhaled therapyWashes hands before giving medicationPerforms the procedure correctlyt Selects correct mask and nebuliser chambert Selects correct dose of salbutamol (2.5 or 5 mg), checks dose, medication and date of expirywith colleaguet Removes lid from nebuliser chambert Pours liquid into bottom of chambert Reassembles chamber and attaches to oxygen maskt Attaches to oxygen tubingt Places facemask over patient’s nose and mouth and securest Starts oxygen at 4–6 l/mint Documents administration in drug chartt Advises patient that it will take 5–7 min to complete nebuliser.Addresses relevant post-procedure follow-up and safety issuesGLOBAL PROCEDURAL MARKA B C D E10
SCENARIO 1W H AT A W H E E Z EStation 4– Data interpretationDATA INTERPRETATION12345678910AB and CAB and CB and DCBAB, C and DA and CPatient (A) – demonstrates a restrictive lung defect with resting hypoxia and reduced transfercoefficient. In view of the history of rheumatoid arthritis, this picture would fit with fibrosingalveolitis. These patients have type I respiratory failure and classically the hypoxia worsenswith exercise.Patient (B) – the history and lung function tests suggest underlying obstructive airwaysdisease. The reduced transfer coefficient suggests probable emphysema and excludes lateonset asthma. The data do not indicate whether there is any reversibility. This is demonstratedby repeating the FEV1 and FVC tests pre- and post-nebuliser. Demonstration of reversibility isimportant, as it indicates whether inhaled steroid therapy may be useful.Patient (C) – this history is suggestive of myasthenia gravis. These patients get an obstructivelung defect, as they are unable to move their chest wall due to the neuromuscular defect. Thetransfer coefficient is normal, as there is no alveolar problem.Patient (D) – this is the history and lung function test for Miss Davis. This shows a normal lungfunction test with symptoms suggestive of intermittent wheeze. Young patients with asthmausually have normal spirometry between exacerbations. If asthma control remains poor, thensome element of chronic obstruction may develop.GLOBAL DATA INTERPRETATION MARKA B C D E11
W H AT A W H E E Z ESCENARIO 1Station 5– Prescribing skillsCheck: DRUG DRs Don’t Forget Signing Off (page 373)Patient details/addressographAllergies, sensitivities and adverse drug reactionsInitialsNo known allergiesDateNot possible to ascertainMedicine/substanceReaction & SeverityMIA 224Gender M / F13/01Weight (kg)64Initials & DateSurname:HeightDAVISFirst name:SARAHDate of birth:24.01.881.60mSurface area (m2)Alerts624011NHS/ Hospital No:DateIN-PATIENT MEDICATION PRESCRIPTIONAND ADMINISTRATION RECORDConsultantTrainee Dr. Name and Bleep no.BEADLEDate of admissionMIAH 224Date chart reboardedEstimated date of discharge13.01.12This chart is no.Transcribing Check by Pharmacy11. of .WardSign . Date .MAU1. . 2. .Supplementary Medication charts in use: Other (please specify): 1 . 2 .Epidural/PCASyringe driverTPNChemotherapyInsulin sliding scaleOnce only medications – loading doses, pre-medication, PGDs or surgical antibiotic propylaxisDateTime tobe givenMedicine (approved ARITHROMYCINRoute30mg PO2.5mg NEB500mcg NEB500mg PO500mg POSignature andbleep no.PharmacyTimegivenGiven byChecked byMIA 224MIA 224MIA 224MIA 224MIA 224As required nSignatureMIA 22412AllergiesCheckedMaxDose/24hrsDose1gRoutePO6 DateTimeDoseRouteDateTimeDoseRoute
W H AT A W H E E Z outeDose1gMaxDose/24hrsIndicationTimeSCENARIO 1As required prescriptionsRoutePO6 HRPharmacySignatureStart13.01 IF FURTHER NEEDED PLEASE CALL DOCTORMIA 224Thromboprophylaxis please prescribe treatment regimens in the regular medications sectionChoice of mechanical prophylaxis and leg(s) to be applied toGraduated elasticcompressionIntermittend pneumaticcompression devicestockings(IPC)13.01LeftStartEndSignatureand BleepDate:Date:No.StartEndSignatureand BleepDate:Date:No.MedicationDoseCLEXANE40mgPlease ensureyou havecompleted theVTE risk assess-Date13.01.12SCSignatureRightEnter details belowEnterTimeEnter details belowBothDose ChangeRouteEnterTimeLegMIA 224InstructionsPharmacyment formBleep no.OxygenTarget Saturation88-92%94/98%*Device: N nasal cannula, SM simple face mask, V venturi,H humidified, RM reservoir mask, OTHER other eg.NCPAP/NIPPVOther specify)Target Saturation not applicableDate StartedIf oxygen saturation falls below target range on prescribed oxygen, patient needs urgent clinical review.If oxygen saturation is above targent range on prescribed oxygen, ask for review.Date ChangedDate ChangedEnterTimePharmacyEnter details below13.01* Device% or L/min(Specify a rangeeg 1-12 L/min)Signature andBleep No.VENTURI40%MIA 224Infusion prescriptions continuedDate&timeRoute13/0113/01Infusion FluidMedicationApproved name withexpiry / unit numberDurationRateName &strengthVolumeDoseIV0.9% SALINEExp:Batch/unit no:1LITRE8hrIV0.9% SALINEExp:Batch/unit no:1 20mmol KclLITRE8hrPrescriber’ssignature &bleep no.DategivenSC subcutaneousIVC intravenous centralIVP intravenous peripheralGiven by/ AddedbyStarttimeCheckbyFinishtimePharmacy13
W H AT A W H E E Z ERegular prescriptions continuedSCENARIO 1Anti-infectives prescriptionFor 5 DaysDate13/01RouteTimesDose06500mgprescribe long term prophylaxis and anti-tuberculosis medications in regular medications sectionDate1314151617MedicationIndicationSignature and bleep no.AMOXYCILLINLRTIMIA 224Pharmacy0912500mg1822500mg24Regular prescriptions continuedAnti-infectives prescriptionFor 5 DaysDate13/01RoutePOTimesDoseprescribe long term prophylaxis and anti-tuberculosis medications in regular medications sectionDate1314151617MedicationIndicationSignature and bleep no.CLARITHROMYCINLRTIMIA 224Pharmacy0609500mg121822500mg24Regular prescriptions continuedRegular InstructionsSignature and bleep no.RoutePOPREDNISOLONE5/7 ONLYMIA 224SignatureMIAPharmacy060930mg12182224Regular prescriptions continuedRegular .5mg222.5mg022.5mgInstructionsSignature and bleep no.MIA 224Pharmacy
W H AT A W H E E Z ESCENARIO 1Regular prescriptions continuedRegular re and bleep no.PharmacyMIA 2240610500mcg14500mcg18500mcg22500mcg24GLOBAL PRESCRIBING MARKA B C D E15
W H AT A W H E E Z ESCENARIO 1Station 6 – Communication skillsPatient scriptYou are a 23-year-old woman with asthma who was diagnosed at age 14 afterhaving increasing wheeze, especially on exertion. You have been admitted tohospital at least six times, including an admission to the intensive care unit 3months ago. You use both of your inhalers at least three or four times a day.You have had to leave your university course because of frequent absences and youhave become frustrated with your asthma preventing you from having a normallife. You smoke five to ten cigarettes a day and know this doesn’t help your asthma,but it helps when you feel ‘stressed’.You do not know anyone with asthma and feel that no one understands howdifficult it is for you. You do not visit your GP, as he just ‘lectures’ you about takingyour inhalers. You have never had an asthma action plan and feel hopeless toprevent further exacerbations, so there is no point taking regular inhalers. You arenot keen on your steroid inhalers, as you know that steroids make you fat.A B C D EA B C D EA B C D EDIAGNOSTICPROFESSIONALISMPROCESSCONTENTA B C D EReviews patient’s current understanding of clinical situation and summarises what hashappened so fart Establishes current control of asthmat Establishes events of this admissiont Identifies current issues regarding controlt Smoking, irregular use of inhalers, frequent admissionsEstablishes patient’s ideas, concerns and expectationst Establishes patients beliefs that she is unable to control asthmat Understanding of stepwise treatmentExplains the key important information; invites patient to ask questions and is able to dealwith them appropriatelyt Addresses importance of smoking cessationt Explains escalation of stepwise therapy (and de-escalation when control is adequate)t Explains asthma action plan and areas of supportt Deals with concern regarding inhaled steroids16
W H AT A W H E E Z ESCENARIO 1Summarises important areas of the consultation back to the patientFormally ends the consultation and ensures appropriate follow-up has been discussedGLOBAL COMMUNICATION MARKA B C D EScenario 1: Reflection and consolidationHistoryMiss Davis is a 23-year-old patient with chronic asthma since the age of 14. Her control is very poor, she hasbeen ventilated in ICU three times. The last time was 3 months ago. She uses her reliever on a daily basis.She is prescribed regular inhaled steroids but does not take them regularly. She sleeps poorly and has hadmultiple admissions and courses of oral steroids. She is a current smoker. She has not been able to workbecause of her frequent exacerbations.Her current illness started 5 days ago. She has had a cough productive of green sputum and a fever. Shehas been increasingly wheezy and it is not responsive to her inhaled ß2-agonist. She has no chest pain orhaemoptysis. She came to hospital as she feels exhausted and is very worried that she may need ventilationonce again.ExaminationMiss Davis is a young lady who, on examination, is short of breath at rest and only able to complete shortsentences. She has oxygen sats of 95% in room air. She is tachypnoeic at 24 resps per minute. She istachycardic at rest with a pulse of 102 and BP 130/75. On examination of the chest she has no evidence ofpneumothorax but has widespread expiratory polyphonic wheeze.The purpose of the examination of any patient with an acute exacerbation of asthma is to assess the severityof the exacerbation in order to ensure that appropriate treatment and escalation is provided in a timely way.Every junior doctor should be able to perform this clinical examination and stratify an exacerbation.The assessment is based on:t Ability to speak in full/short sentences or not at allt RR and respiratory effortt Oxygen saturationst PEFR as a percentage of either best (if known) or expectedt A normal or rising pCO2 (a sign of tiring of respiratory effort).The exacerbation is then classified as mild, moderate, severe or life-threatening.17
W H AT A W H E E Z ESCENARIO 1InvestigationsThe diagnosis of chronic asthma is based on history and a clinical probability of more than one of thefollowing symptoms:t wheezet breathlessnesst chest tightnesst coughparticularly if:t symptoms worse at night and in the early morningt symptoms occur in response to exercise, allergen exposure, cold air and after taking aspirin or betablockers.If the diagnosis of chronic asthma is most likely, a trial of inhaled ß2-agonist should be started.The ability to instruct in the technique and subsequently obtain accurate PEFR in all patients presenting withwheeze and dyspnoea is a core skill for all foundation year doctors.ManagementThe management of any chronic condition can be extremely challenging to both the patient and juniordoctor. The key is to control symptoms with a stepwise escalation of therapy. Good control is that whichenables patients with asthma to complete ADLs without interruption and to require rescue therapy only upto once per week.Liaison with primary care and asthma specialist nurses and personalised asthma action plans facilitatepatient-led therapy.Further reading and web linksBTS/SIGN guidelines for both diagnosis, acute and chronic management of guidelines.aspx18
SCENARIO 2Scenario 2:‘Heartache’Station 1History10-minute stationYou are the FY1 attached to a GP surgery. The next patient is Mr James Wright, whohas made an urgent appointment to see the doctor. He has agreed to see you beforeseeing the GP. Please take a focused history from the patient with a view to presenting the historyand likely diagnosis to the GP.You will be assessed on the following areas, as well as the content and diagnosticreasoning of your history – take them into account in your presentation.Professionalismt t t t Professional appearance (NHS dress code) – including general appearance, hair and jewellery;maintains patient and personal safetyPolite introduction; identifies patient or interviewee correctly; confirms patient’s date of birth fromname band or other sourceObtains informal consent; maintains patient’s privacyDisplays empathetic and caring attitudes and behaviours throughout.Processt t t t Good organisation and structure; appropriate use of open and closed questionsAppropriate fluency/rhythm/pace to the interview – this may change depending on environmentand acute nature of the problemAppropriate time for the patient to respond/reply to questionsAppropriate acknowledgement of difficult or emotional areas of the patient’s history.Communication skillst t t t Demonstrates caring and sympathetic attitudeAsks open questionsInvites patient to ask questions and answers them appropriatelyAddresses patient’s ideas, concerns and expectations.19
H E A R TAC H EStation 2Examination10-minute stationS CENARIO 2After completing and presenting the history, the GP asks you to perform a focused/appropriate examination of the patient. Mr Wright was also seen this morning by thePractice Nurse, who performed a series of clinical observations and tests on him. Youmay ask for these during your assessment. You should present the relevant findings (given within the station) to the GP in anappropriate manner for a busy GP surgery.You will be assessed on the following areas, as well as the content and skills of yourexamination – take them into account in your presentation.Professionalismt t t t t Professional appearance; maintains infection control standards, including hand cleaning andappropriate use of gloves and apronsMaintains patient and personal safetyPolite introduction; identifies patient and confirms date of birth from name band or other sourceObtains informal consent; maintains patient privacy and dignityDisplays empathetic and caring attitudes and behaviours throughout.Processt t t t Appropriate fluency/rhythm/pace to the examination – this may change depending on environmentand acute nature of problemGood organisation and structure of examination; sensitive and empathetic approachUses appropriate clinical techniques throughoutMaintains privacy and dignity throughout.Clinical communicati
ST3 Medical Registrar as if you were on a busy medical take. [NB If you have a model do not read this section] Clinical findings o Patient appears dyspnoeic at rest, and unable to complete sentences o RR 24 breaths per minute, O 2 sats 95% room air 100% on 1