Transcription
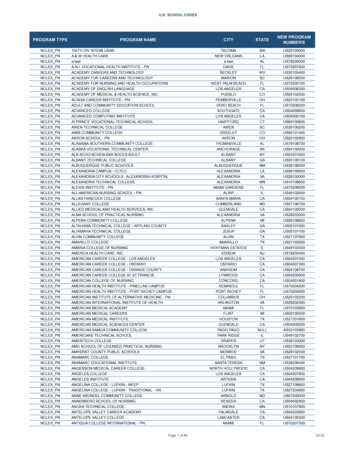
Training programcosting exampleMarcia Weaver, PhDResearch Associate ProfessorInstitute for Health Metrics and Evaluation (IHME)October 13, 2016
Learning objectivesFollowing this session, participants will:1. Correctly explain how five principles of costanalysis can be applied to a training program2. Interpret results of the cost-effectivenessanalysis for the Integrated Infectious DiseaseCapacity-Building Evaluation (IDCAP)
1. PerspectivePerspective is the point of view from which the costs arecalculated. It addresses the issue of which inputs orresources to include. Training program budget for your organization Donor, which includes other partners they support Societal, which includes opportunity costs
Training program budgetCost perunitTrainerOn-site[.]Trainingprogrambudget 100 perday 1,000per site5-day computerbased training plus3-day workshopUnitsCost3 3000 7,35010-day training pluson-site visitsUnitsCost10 1,0005 5,000 12,250
Donor perspectiveCost 5-day computerbased training plus3-day workshopUnitsCost10-day training pluson-site visitsUnitsCost 7,350 225 perday3 675 8,025 12,25010 2,250 15,000
Societal perspectiveCost5-day computer – 10-day trainingper unit based training plus plus on-site visits3-day workshopUnitsCostUnits CostTraining program budgetContract withvenueTrainees’ timeTotal cost 7,350 225per day 20 perday 12,2503 67510 2,250200 4,000275 5,500 12,025 20,000
Societal perspectiveCost5-day computer – 10-day trainingper unit based training plus plus on-site visits3-day workshopUnitsCostUnits CostTraining program budgetContract withvenueTrainees’ timeTotal costCost/trainee 7,350 225per day 20 perday 12,2503 67510 2,250200 4,000275 5,50025 12,025 48125 20,000 800
2. Financial vs. economic costFinancial cost – For goods and services that aretraded on a competitive market, the opportunitycost is simply the pricewhere opportunity cost is the value of the mostbeneficial alternative use of the resources.Economic cost – Value of goods and services thatare not purchased such as volunteer time or forwhich the price is distorted
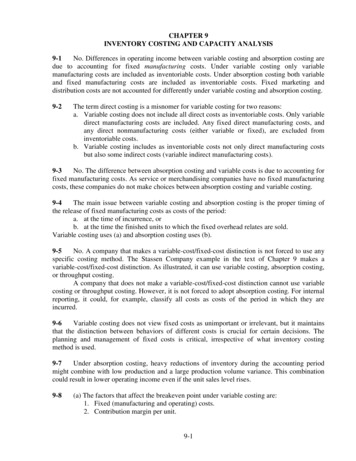
3. Output vs. outcome1. The cost per unit of output is valid when thetwo programs being compared are equallyeffective.2. A cost per unit of outcome can addressdifferences in effectiveness across programs.3. The scope of the analysis is determined by thedenominator. Only programs with a commondenominator can be compared.
Cost per unit of output5-day computerbased training plus3-day workshop10-day trainingplus on-siteTraining 12,025 20,000Supervision 8,000 2,000Total cost 20,025 22,000Cost of transfer of learning
Cost per unit of output5-day computerbased training plus3-day workshop10-day trainingplus on-siteTraining 12,025 20,000Supervision 8,000 2,000Total cost 20,025 22,000Cost per trainee 20,025/25 801 22,000/25 880Cost of transfer of learning
Cost per unit of intermediate outcome5-day computer10-day training plusbased training plus 3- on-siteday workshopCost of transfer of learningTraining 12,025 20,000Supervision8,000 2,000Total cost20,025 22,000Trainees who meet standard1522Cost per trainee who metstandard 20,025/15 1,335 22,000/22 1,000
Cost analysis: Compares the cost per unit ofoutput when to programs are equally effectiveCost-effectiveness analysis (CEA): Comparescost to effectiveness, e.g. Clinician who meets standard /life years saved from intervention
4. Incremental analysisIncremental cost effectiveness ratio (ICER)Δ Change in health care costΔ Change in health outcomes
ICER is a slopeHealthoutcomesHealthBenefitsHealth Care Cost
PMTCT Cost/HIV infection avertedPre-trainingPost-trainingProgram costRemuneration 80,000 84,000Supplies15,00018,000Capital5,00010,000 100,000 112,000Total CostNumber of mother-infant pairs1,0001,200Base case-vertical transmission25%25%Number of HIV infections averted1,000*.25*.63 1581,200*.25*.63 189Incremental cost 112,000 - 100,000 12,000Incremental effectiveness189 – 158 31ICER 12,000/31 381
4. Incremental analysisEffects:HIVinfectionsaverted189ICER158 100,000 112,000Health Care Cost
5. Sensitivity analysis Calculation of alternative cost-effectiveness resultswhen there is uncertainty about one or moreparameters. It shows the extent to which uncertainty about aparameter would substantially affect the estimate.
PMTCT CEA with uncertaintyPre-trainingTotal CostPost-training 100,000 112,000Number of mother-infant pairs1,0001,200Base case-vertical transmission25%25%Lower bound19%19%Upper bound30%30%Incremental cost 112,000 - 100,000 12,000ICER – base case 12,000/31 381Lower bound 12,000/24 501Upper bound 12,000/38 317
Summary – 5 principles1. Perspective2. Financial vs. economic cost3. Output vs. outcome4. Incremental analysis5. Sensitivity analysis
Aim: Create & evaluate an innovative capacity-buildingprogram Develop an IntegratedManagement of InfectiousDisease (IMID) curriculum formidlevel practitioners Complement the trainingprogram with On-Site Support(OSS) Measure their effect on thequality of care and healthoutcomes Estimate the costeffectiveness of theinterventionsPhoto by Charles Steinberg, MD
Integrated Management of Infectious Disease (IMID) WHO curricula such as IMCI,ETAT, and IMAI Advances in health professionaleducation (Miceli, et al. IJID2012) HIV, TB, malaria, andpneumonia
On-Site Support (OSS) Mobile Team Medical officer Clinical Officer LaboratoryTechnologist Districtcontactperson/nurseofficer
Mixed Design With Pre/Post and ClusterRandomized Trial ComponentsTime 0ARM ATime 1IMIDOSSARM BTime 2Bi-monthly OSSIMIDOSS
23 Facility performance indicators spanned seven areas Emergency triage, assessment and treatment(ETAT) Case management of fever HIV prevention HIV Care ART Respiratory illness TB/HIV
Example of results: Percentage of outpatients triagedTime 0: Arm ATime 0: Arm B
OSS significantly increased the % of outpatients triaged% of Outpatients TriagedRR (CI)Arm ATime 1 – Time 0Arm BTime 1 – Time 0Arm A vs. Arm B: Time 1 – Time02.03 (1.13, 3.64)*1.29 (1.01, 1.64)*1.58 (0.82, 3.01)
Analysis for 23 indicators showed impact on 6 indicators Outpatients triaged Emergency & priority patients admitted, detained or referred Malaria suspects received appropriate treatment Smear negative malaria suspects treated w/ anti-malarials U5 pneumonia suspects assessed for pneumonia HIV infected patients enrolled in care
Cost AnalysisIntervention Curriculum Development IMID On-site SupportTreatment Drugs
Preliminary cost analysis in USIMID OSS(Arm A)GrantCurriculumIMID0SSTotalMOH SalariesIMIDOSSTotalMalaria drug savingsNet costIMID Incremental(Arm B) cost of OSS 16,99422,04749,230 88,271 12,61022,047 464533 997(523) 88,745 34,656456 456(77) 35,036 53,709
Integrated Epidemiological Model
Malaria & Pneumonia Model
IMID OSSNet costLives saved /LifeDALYs Saved /DALYIMIDIncre-mental 88,745 35,035 53,71023158 3,875 2,336 6,799729484245 122 72 219
Summary - IDCAP Integrated epidemiological model combines mostindicators to provide one aggregate measure of theeffect IMID and OSS across three age groups. Uganda’s GDP in 2011 was roughly US 487 per capita,suggesting IMID and OSS were highly cost-effectiveinterventions both individually and in combination byWHO standards.
Thank you!
5-day computer– based trainingplus 3-day workshop 10-day training plus on-site visits Units Cost Units Cost Training pro - gram budget 7,350 12,250 Contract with venue 225 per day 3 675 10 2,250 Trainees’ time 20 per day 200 4,000 275 5,500 Total cost 12,025 20,000 Societal perspective