Transcription
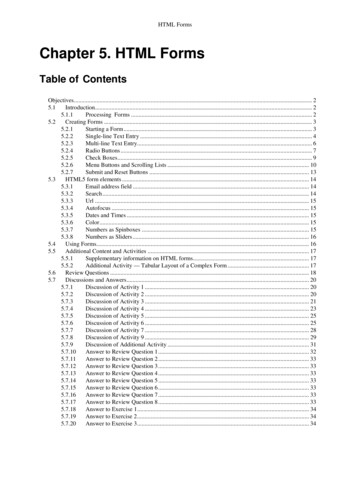
Durable Medical Equipment Provider ManualManual Updated 01/01/11FORMSNumberNameRevision DateDHHS 126Confidential Complaint06/2007DHHS 130Claim Adjustment Form 13003/2007DHHS 140Medicaid Provider Inquiry06/2007DHHS 142Request for Medicaid Forms and Publications06/2007DHHS 205Medicaid Refunds01/2008DHHS 931Health Insurance Information Referral Form01/2008Reasonable Effort Documentation06/2007Authorization Agreement for Electronic Funds Transfer01/2009Duplicate Remittance Request Form11/2010CMS-1500Sample Claim Showing Medicaid and Medicare withNPI08/2005CMS-1500Sample Claim Showing Medicaid Only with NPI08/2005CMS-1500Sample Claim Showing Medicaid and Private Pay withNPI and Medicaid Provider ID08/2005CMS-1500Sample Claim Showing Medicare, Medicaid, Private Paywith NPI and Medicaid Provider ID08/2005Sample Edit Correction Form10/2008Sample Remittance Advice06/2007DME 001Medicaid Certificate of Medical NecessityEquipment/Supplies04/2010DME 003Medicaid Certificate of Medical NecessityPower/Manual Wheelchairs and/or Accessories04/2010DME 004Medicaid Certificate of Medical NecessityOrthotics, Prosthetics, and Diabetic Shoes04/2010DME 005Medicaid Certificate of Medical NecessityEnteral Nutrition04/2010DME 006Medicaid Certificate of Medical NecessityParenteral Nutrition04/2010DME 007Medicaid Certificate of Medical NecessityOxygen04/2010DME 008Certificate of Repair and Labor Cost02/2010i
Durable Medical Equipment Provider ManualManual Updated 01/01/11FORMSNumberNameJustification for Home Uterine ActivityMonitor/Supplies (HUAM) for Subcutaneous TocolyticTherapyRevision Date06/2007MR/RD A-5 SC Dept of Disabilities and Special Needs MR/RDWaiver Authorization For Services02/2004HASCI-12-F SC Dept of Disabilities and Special Needs Head andSpinal Cord Injury Waiver Authorization for PERSServices02/2004HASCI 12-I SC Dept of Disabilities and Special Needs Head andSpinal Cord Injury Waiver Authorization for SpecializedSupplies and Adaptations02/2004219-DMEMedicaid Enrollment Data DME Supplier07/2006DHHS 214Prior Authorization04/1997Program Coordinators03/2009ii
STATE OF SOUTHCAROLINADEPARTMENT OF HEALTHAND HUMAN SERVICESSEND TO:CONFIDENTIAL COMPLAINTDIRECTOR, DIVISION OF PROGRAM INTEGRITYDEPARTMENT OF HEALTH AND HUMAN SERVICESP.O. BOX 100210, 1801 MAIN STREET, COLUMBIA, SOUTH CAROLINA 29202-3210PROGRAM INTEGRITYTHIS REPORT IS DESIGNED FOR THE REPORTING OF POSSIBLE ABUSE BY MEDICAIDPROVIDERS AND/OR RECIPIENTS. USE THE SPACE BELOW TO EXPLAIN IN DETAIL YOURCOMPLAINT. PLEASE IDENTIFY YOURSELF AND WHERE YOU CAN BE REACHED FOR FUTUREREFERENCES. UNLESS OTHERWISE INDICATED, ALL INFORMATION SHOULD BE PRINTED ORTYPED.YOUR COMPLAINT WILL REMAIN CONFIDENTIAL.SUSPECTED INDIVIDUAL OR INDIVIDUALS:NPI or MEDICAID PROVIDER ID: (if applicable)MEDICAID RECIPIENT ID NUMBER: (if applicable)ADDRESS OF SUSPECT:LOCATION OF INCIDENT:DATE OF INCIDENT:COMPLAINT:NAME OF PERSON REPORTING: (Please print)ADDRESS OF PERSON REPORTING:SIGNATURE OF PERSONREPORTING:DATE OF REPORTTELEPHONE NUMBER OF PERSON REPORTING:SIGNATURE: (SCDHHS Representative Receiving Report)SCDHHS Form 126 (revised 06/07)
STATE OF SOUTHCAROLINADEPARTMENT OF HEALTHAND HUMAN SERVICESMEDICAID PROVIDER INQUIRYTODAY’S DATE:MAIL TO:ATTENTION UNITS.C. DEPT. OF HEALTH AND HUMAN SERVICESPOST OFFICE BOX 8206COLUMBIA, SOUTH CAROLINA 29202-8206NPI or MEDICAID PROVIDER ID:TELEPHONE:PROVIDER NAME AND ADDRESS:TYPE OF PROVIDER (i.e., Dentist, Group, etc.)DATE CLAIM ----------------------------------FOLD --------------------------------PATIENT’S NAME (First, Initial, Last)MEDICAID NUMBER (10 Digits)HAS THE CLAIM APPEARED ON THE PROVIDER’S REMITTANCE ADVICE?(CHECK ONE)YESNOCLAIMS STATUS ON REMITTANCE ADVICEPAYMENT DATEDATE OF SERVICEIS MEDICARE COVERAGE INVOLVED?YESNO17-DIGIT CLAIM REFERENCE NUMBERSTATEMENT OF PROBLEM OR QUESTIONSIGNATURE OF PROVIDERRESPONSEAGENCY REPRESENTATIVESCDHHS Form 140 (revised 06/07)DATE
STATE OF SOUTH CAROLINADEPARTMENT OF HEALTHAND HUMAN SERVICESREQUEST FOR MEDICAIDFORMS AND PUBLICATIONSNPI or MEDICAID PROVIDER ID:WHEN COMPLETED PLEASE FORWARD TO:SC DEPARTMENT OF HEALTH AND HUMAN SERVICESSUPPLYPOST OFFICE BOX 8206COLUMBIA, SOUTH CAROLINA 29202-8206TYPE OF PROVIDER:TELEPHONE:-OR- FAX TO:--(803) 898-4528CONTACT NAME:NAME OF PROVIDERSTREET ADDRESS FOR UPS DELIVERY (PLEASE PRINT OR TYPE)ITEMS REQUESTEDFORM/PUBLICATION NO.SCDHHS FORM 142 (revised 06/07)TITLE OF FORM OR PUBLICATIONQUANTITY
South Carolina Department of Health and Human ServicesForm for Medicaid RefundsPurpose: This form is to be used for all refund checks made to Medicaid. This form gives the information needed toproperly account for the refund. If the form is incomplete, the provider will be contacted for the additional information.Items 1, 2 or 3, 4, 5, 6, & 7 must be completed.Attach appropriate document(s) as listed in item 8.1. Provider Name:2. Medicaid Legacy Provider # (Six Characters)OR 3. NPI#4. Person to Contact:& Taxonomy5. Telephone Number:6. Reason for Refund: [check appropriate box] Other Insurance Paid (please complete a – f below and attach insurance EOMB)a Type of Insurance: ( ) Accident/Auto Liability ( ) Health/Hospitalizationb Insurance Company Namec Policy #:d Policyholder:e Group Name/Group:fAmount Insurance Paid:Medicare( ) Full payment made by Medicare( ) Deductible not due( ) Adjustment made by Medicare Requested by DHHS (please attach a copy of the request)Other, describe in detail reason for refund:7. Patient/Service Identification:Patient NameMedicaid I.D.#(10 digits)Date(s) ofServiceAmount ofMedicaid Payment8. Attachment(s): [Check appropriate box] Medicaid Remittance Advice (required)Explanation of Benefits (EOMB) from Insurance Company (if applicable)Explanation of Benefits (EOMB) from Medicare (if applicable)Refund checkMake all checks payable to: South Carolina Department of Health and Human ServicesMail to: SC Department of Health and Human ServicesCash ReceiptsPost Office Box 8355Columbia, SC 29202-8355DHHS Form 205 (01/08)Amount ofRefund
SOUTH CAROLINA DEPARTMENT OF HEALTH AND HUMAN SERVICESMEDICAID HEALTH INSURANCE INFORMATION REFERRAL FORMProvider or Department Name: Provider ID or NPI:Contact Person: Phone #: Date:IADD INSURANCE FOR A MEDICAID BENEFICIARY WITH NO INSURANCE IN THE MEDICAIDMANAGEMENT INFORMATION SYSTEM (MMIS) – ALLOW 25 DAYSBeneficiary Name:Date Referral Completed:Medicaid ID#:Policy Number:Insurance Company Name:Group Number:Insured's Name:Insured SSN:Employer's Name/Address:IICHANGES TO AN INSURANCE RECORD THAT IS IN THE MMIS – MIVS SHALL WORK WITHIN 5 DAYSa.beneficiary has never been covered by the policy – close insurance.b.beneficiary coverage ended - terminate coverage (date)c.subscriber coverage lapsed - terminate coverage (date)d.subscriber changed plans under employer - new carrier is- new policy number ise.beneficiary to add to insurance already in MMIS for subscriber or other family member.(name)ATTACH A COPY OF THE APPROPRIATE DOCUMENTATION TO THIS FORM.Submit this information to Medicaid Insurance Verification Services (MIVS).Fax:orMail:803-252-0870Post Office Box 101110Columbia, SC 29211-9804IIINEW POLICY NUMBERS FOR INSURANCE IN THE MMIS WITH THE SUBSCRIBER SSN(SCDHHS is collecting new unique policy numbers and plans to replace existing insurance records through MMISonline modification as computer resources are available.)Medicaid Beneficiary ID: SSN:Carrier Name/Code: New Unique Policy Number:Submit this information to South Carolina Department of Health and Human Services (SCDHHS).Fax:orMail:803-255-8225Post Office Box 8206, Attention TPLColumbia, SC 29202-8206DHHS 931 – Updated January 2008
SOUTH CAROLINA DEPARTMENT OF HEALTH AND HUMAN SERVICESREASONABLE EFFORT DOCUMENTATIONPROVIDERDOSNPI or MEDICAID PROVIDER IDMEDICAID BENEFICIARY NAMEMEDICAID BENEFICIARY ID#INSURANCE COMPANY NAMEPOLICYHOLDERPOLICY NUMBERORIGINAL DATE FILED TO INSURANCE COMPANYDATE OF FOLLOW UP ACTIVITYRESULT:FURTHER ACTION TAKEN:DATE OF SECOND FOLLOW UPRESULT:I HAVE EXHAUSTED ALL OPTIONS FOR OBTAINING A PAYMENT OR SUFFICIENT RESPONSEFROM THE PRIMARY INSURER.(SIGNATURE AND DATE)ATTACH A COPY OF FORM TO THE APPROPRIATE CLAIM OR ECF AND FORWARD TO YOURMEDICAID CLAIMS PROCESSING POST OFFICE BOX.Revised 05/2007
RUN DATE 05/01/2007 000001204REPORT NUMBER CLM3500ANALYST IDSIGNON IDTAXONOMY:SFL ZIP:1234PROV/XWALK RECIPIENTP AUTH TPLIDIDNUMBERABC1231111111111NPI: 1234567890SC DEPARTMENT OF HEALTH AND HUMAN SERVICESEDIT CORRECTION FORMHIC - 76 SPEC DOC IND NPRV ZIP:56789INJURY EMERG PC COORD---- DIAGNOSIS ---CODEPRIMARYSECONDARY871.3.CLAIM CONTROL #9999999999999999APAGE 1136 ECF 1136 PAGE 1 OF 1EMC YORIGINAL CCN:ADJ CCN:EDITSINSURANCE EDITSCLAIM EDITSLINE EDITS01) 71410 RECIPIENT NAME – DOE, JANE13RES14ALLOWED11 DATE OF BIRTH15DATE OFSERVICELNNO16PLACE17PROCCODE01/25/199218MOD12 SEXF1920INDIVIDUAL CHARGEPROVIDERIND21PAY23NDC.00102/01/0012V2624NPI: 1234567890TAXONOMY:2/ /NPI:TAXONOMY:3/ /NPI:TAXONOMY:4/ /NPI:TAXONOMY:5/ /NPI:TAXONOMY:6/ /NPI:TAXONOMY:7/ /NPI:TAXONOMY:8/ /NPI:TAXONOMY:242526INS CARRPOLICYINS CARRNUMBERNUMBERPAIDOLTDME00065.0027TOTAL CHARGE0128AMT REC'D INS0229BALANCE DUE0330OWN REF #******************************22**AGENCY USE ONLY**UNITS **APPROVED EDITS********REJECTED LINE !!!!!!!!!!!!!!!!!!!!!!!!! CLAIMS/LINE PAYMENT INFO !!!! EDITPAYMENT DATE 5RESOLUTION DECISIONADDITIONAL DIAG CODES:.RETURN TO:MEDICAID CLAIMS RECEIPTP. O. BOX 1412COLUMBIA, S.C. 29202-1412PROVIDER:ACME DME SUPPLIERSPO BOX 00000ANYWHEREXO.INSURANCE POLICY INFORMATION00000-0000"PLEASE NOTE: EDIT CORRECTION FORMS RETURNED TO DHHS WITH NO CORRECTIVE ACTION WILL BE DISREGARDED"* INDICATES A SPLIT CLAIM
Sample Remittance Advice (page 1)This page of the sample Remittance Advice shows a paid claim, as well as aVoid/Replacement claim for which both the Void and the Replacement processed duringthe same payment cycle.# AB0008 ACME DME SUPPLIESPO BOX 000000FLORENCESC000000000.121212121234.YPROVIDER ID.PROFESSIONAL SERVICESPAYMENT DATEPAGE -------------- DEPT OF HEALTH AND HUMAN SERVICES ------------ ---- AB00080000 REMITTANCE ADVICE 03/26/2007 1 -------------- SOUTH CAROLINA MEDICAID PROGRAM ------------ ---- --------- ----------------- ------ --------- ------ -------- -------- - ---------- ------------------- --- ------- ------- ------- PROVIDERS CLAIM SERVICE RENDERED AMOUNT TITLE 19 S RECIPIENT RECIPIENT NAME M TLE. 18 COPAY TITLE OWN REF. REFERENCE DATE(S) BILLED PAYMENT T ID. F M O ALLOWED AMT 18 NUMBER NUMBER PY IND MMDDYY PROC. MEDICAID S NUMBER I I LAST NAME D CHARGES PAYMENT --------- ----------------- ------ --------- ------ -------- -------- - ---------- ------------------- --- ------- ------- ------- ABB222222 0406001089000400A 1192.00 243.71 P 1112233333 MCLARK 0.00 01 021507 V2624 800.00 117.71 P 0HH 0.00 02 021507 V2623 392.00 126.00 P 0HH 0.00 VOID OF ORIGINAL CCN 0404711253670430A PAID 02/28/04 ABB222222 0406001089000400U 1412.00- 273.71- 1112233333 MCLARK 01 012107 V2624 1112.00- 143.71- 0HH 02 012107 V2623 300.00- 130.00- OHH REPLACEMENT OF ORIGINAL CCN 0404711253670430A PAID 02/28/04 ABB222222 0407701389002500A 1001.50 42.75 P 1112233333 MCLARK 0.00 01 012107 V2624 142.50 42.75 P 0HH 0.00 02 012107 V2623 859.00 0.00 R 0HH 0.00 TOTALS 2 2193.50 286.46 0.00 0.00 --------- ----------------- ------ --------- ------ -------- -------- - - -------- ------------------- --- ------- ------- ------- 286.46 ------------ ------------ STATUS CODES:PROVIDER NAME AND ADDRESSFOR AN EXPLANATION OF THECERT. PG TOTMEDICAID PG TOT --------------------------------- ERROR CODES LISTED ON THIS ------------- ------------- P PAYMENT MADE ACME DME SUPPLIES FORM REFER TO: "MEDICAID 0.00 286.46 R REJECTED PROVIDER MANUAL". ------------- ------------- S IN PROCESS PO BOX 000000 CERTIFIED AMTMEDICAID TOTALE ENCOUNTER FLORENCESC 00000-0000 IF YOU STILL HAVE QUESTIONS ------------- ------------- ------------- --------- PHONE THE D.H.H.S. NUMBER 0.00 0.00 0.00 --------------------------------- SPECIFIED FOR INQUIRY OF ------------- ------------- ------------- --------- CLAIMS IN THAT MANUAL.FEDERAL RELIEFMAXIMUS AMTCHECK TOTALCHECK NUMBER
Sample Remittance Advice (page 2)This page of the sample Remittance Advice shows a claim-level Void without a corresponding Replacement claim.PROVIDER ID. -------------- AB11110000 -------------- ---------------- PAYMENT DATEPAGE CLAIM ------------ ---- ADJUSTMENTS 03/26/2007 2 SOUTH CAROLINA MEDICAID PROGRAM ---- ---------------- ------------ --------- ----------------- --- --------- ------ -------- -------- - - - ---------- ---------- --- ------ ------------------------ PROVIDERS CLAIM SERVICE RENDERED AMOUNT TITLE 19 S RECIPIENT RECIPIENT NAME M ORG OWN REF. REFERENCE PY DATE(S) BILLED PAYMENT T ID. F M O CHECK ORIGINAL CCN NUMBER NUMBER IND MMDDYY PROC. MEDICAID S NUMBER LAST NAME I I D DATE --------- ----------------- --- --------- ------ -------- -------- - ---------- -------------- --- ---- ------------------------ ABB222222 0406001089000400U 513.00- 197.71- 1112233333 CLARKM 022807 0404711253670430A 01 012107 V2624 453.00 160.71- P 0HH 02 012107 V2623 60.00 33.00- P OHH TOTALS 1 513.00- 193.71- --------- ----------------- ------------- ------ -------- -------- - ---------- -------------- --- ------ ------------------------ MEDICAID TOTALCERTIFIED AMTFEDERAL RELIEFTO BE REFUNDEDDEBIT BALANCE ------------- ------------- ------------- IN THE FUTUREPRIOR TO THIS 243.71 0.00 0.00 ---------- REMITTANCE ------------- ------------- ------------- 0.00 ------------- ---------- 0.00 ADJUSTMENTSMAXIMUS AMT ------------- ------------- ------------- PROVIDER NAME AND ADDRESS 193.71- --------------------------------- YOUR CURRENT ------------- ------------- ACME DME SUPPLIES DEBIT BALANCECHECK TOTALCHECK NUMBER ------------- ------------- --------- PO BOX 000000 0.00 50.00 4197304 FLORENCESC 00000-0000 ------------- ------------- --------- --------------------------------- DEPT OF HEALTH AND HUMAN SERVICES
Sample Remittance Advice (page 3)This page of the sample Remittance Advice shows four gross-level adjustments.Gross-level adjustments always appear on the final page of the Remittance Advice.PROVIDER ID.PAGEPAYMENT DATE ------------ ---- ADJUSTMENTS 03/26/2007 3 SOUTH CAROLINA MEDICAID PROGRAM ---- ---------------- ------------ --------- ----------------- ------------- ----------- ---------- -------------- ------ ---------- --------- ----------- ---------- PROVIDERS CLAIM SERVICE PROC / DRUG RECIPIENT RECIPIENT NAME ORIG. ORIGINAL DEBIT / EXCESS OWN REF. REFERENCE DATE(S) ID. F M CHECK PAYMENT ACTION CREDIT NUMBER NUMBER MMDDYY CODE NUMBER LAST NAME I I DATE AMOUNT REFUND --------- ----------------- ------------- ----------- ---------- -------------- ------ ---------- --------- ----------- ---------- TPL 2 0408600003700000U DEBIT -2389.05 TPL 4 0408600004700000U DEBIT -1949.90 TPL 5 0408600005700000U DEBIT -477.25 TPL 6 0408600006700000U DEBIT -477.25 PAGE TOTAL: 5293.45 0.00 --------- ----------------- ------------- ----------- ---------- -------------- ------ ---------- --------- ----------- ---------- MEDICAID TOTALCERTIFIED AMTFEDERAL RELIEFTO BE REFUNDEDDEBIT BALANCE ------------- ------------- ------------- IN THE FUTUREPRIOR TO THIS 0.00 0.00 0.00 ---------- REMITTANCE ------------- ------------- ------------- 0.00 ------------- ---------- 0.00 ADJUSTMENTSMAXIMUS AMT ------------- ------------- ------------- PROVIDER NAME AND ADDRESS 0.00 0.00 --------------------------------- YOUR CURRENT ------------- ------------- ACME DME SUPPLIES DEBIT BALANCECHECK TOTALCHECK NUMBER PO BOX 000000 ------------- ------------- --------- FLORENCESC 00000-0000 5293.45 0.00 ------------- ------------- --------- --------------------------------- -------------- AB11110000 -------------- --------------- DEPT OF HEALTH AND HUMAN SERVICES
SOUTH CAROLINA DEPARTMENT OF HEALTH AND HUMAN SERVICESMEDICAID CERTIFICATE OF MEDICAL NECESSITY FORMFOR EQUIPMENT/SUPPLIESSECTION A: MUST BE COMPLETED BY DME PROVIDER:(1) Recipient’s name: Medicaid # (10 digits):(2) DOB: / / : Sex: HT: (in); WT: Date of Service: / /(3) Provider’s name: Provider’s DME # NPI#(4) Street address: City: State: Zip: Local telephone #:(5) Provider’s signature: Date:(6) LIST ALL PROCEDURE CODES THAT ARE ORDERED BY THE TREATING/ORDERING PHYSICIAN FOR EQUIPMENT/SUPPLIES:NOTE: FOR ALL PROCEDURE CODES THAT ARE COVERED, BUT DO NOT HAVE AN ESTABLISHED PRICE, YOU MUST INCLUDEMANUFACTURER PRICE LIST.SECTION B: ALL FIELDS IF APPLICABLE MUST BE COMPLETED BY TREATING/ORDERING PHYSICIAN:(7) Diagnosis codes (ICD-9) Description(s):(8) Indicate patient’s ambulatory status while performing activities of daily living: Non-ambulatory Ambulatory, without assistanceAmbulatory with the aid of a walker or cane, Ambulatory, with other assistance as describedDoes the patient have decubitus ulcers? Yes No.If yes, circle stage(s): I, II, III, or IV. Indicate the wound size(s):Please describe how this equipment / supply is medically necessary, the benefits to the recipient and how long will it take for the benefit to beevident:(9) For supplies, please indicate the dressing change required per day, week, month, etc.Is additional information attached on separate sheet? Yes No (If “yes,” enter recipient’s name & I.D. Medicaid number onattachment(10) Please indicate the date that the patient was seen for the equipment/supplies prescribed:(11) Please indicate the prescription date:(12) Duration of need (maximum of 12 months):(Please indicate duration by months, not to exceed 12).I certify that I am the treating/ordering physician identified in Section B of this form. Any statement attached hereto has been reviewed and signed by me. I certifythat the medical necessity information is true, accurate and complete, to the best of my knowledge, and I understand that any falsification, omission or concealmentof material fact may subject me to civil or criminal liability. Additionally, I certify that the requested equipment/supplies are appropriate for the patient.(13) PHYSICIAN’S NAME :PHYSICIAN’S NPI # :PHYSICIAN’S SIGNATURE DATE / / (SIGNATURE AND DATE STAMPS ARE NOT ACCEPTABLE)PLEASE REFER TO THE MEDICAID CMN POLICY IN THE DME MEDICAID PROVIDER MANUAL.DME 001 - Dated 01/01/11
INSTRUCTIONS FOR COMPLETING THE MEDICAID CERTIFICATE OF MEDICAL NECESSITY FOR EQUIPMENT/SUPPLIESSECTION A: MUST BE COMPLETED BY DME PROVIDERRECIPIENT’S NAME ANDMEDICAID #:Indicate the patient’s name and his/her Medicaid # (10 digits).PATIENT DOB, SEX, HEIGHT, WEIGHT:Indicate patient’s date of birth (MM/DD/YY) and sex (male or female); height in inches and weight inpounds.DATE OF SERVICE:Indicate the date of service (DOS). The date of service must be the same as the delivery date.PROVIDER‘S NAME, DME #AND NPI#:Indicate the name of the DME company (Provider name), Provider’s DME# and NPI#.PROVIDER’S PHYSICAL ADDRESSAND TELEPHONE NUMBER:Indicate the provider’s physical address (provider’s location) and telephone number.PROVIDER SIGNATURE AND DATE:Signature of DME provider representative and date.HCPCS CODES:List all HCPCS procedure codes for items ordered by the treating/ordering physician.Note: For all procedure codes that are covered, but do not have an established price, you must includemanufacturer price list.SECTION B: MUST BE COMPLETED BY TREATING/ORDERING PHYSICIAN:DIAGNOSIS CODES:In the first field, list the ICD-9 diagnosis code(s) that represent(s) the primary reason(s) for orderingthis item. In the second field, list the description(s) for each ICD-9 diagnosis code(s).QUESTION SECTION:These fields are used to gather clinical information to help Medicaid determine the medical necessityfor the item(s) being ordered. Answer each question which applies to the items ordered.DATE PATIENT WAS SEEN FOREQUIPMENT/SUPPLIES PRESCRIBED:Indicate the date patient was seen by the treating/ordering physician, nurse practitioner or physicianassistant for the equipment/supplies prescribed. The treating/ordering physician, nurse practitioneror physician assistant must examine the beneficiary within 60 days before prescribing equipmentand/or supplies.PRESCRIPTION DATE:Indicate the prescription date. The prescription date must be within 60 days of the date oftreating/ordering physician’s signature and the date the beneficiary was seen by the physician, nursepractitioner, or physician assistant. All MCMNs that are not signed within this time frame will bereturned (if submitted with a PA) or rejected (if attached to a claim) and the MCMN will be deemedinvalid.EST. LENGTH OF NEED:Indicate the estimated length of need (the length of time the physician expects the patient to requireuse of the order item) by filling in the appropriate number of months, up to 12 months. An MCMNcan be valid up to a maximum of 12 months from the date the patient was seen for theequipment/supplies prescribed.PHYSICIAN ATTESTATION:The physician signature certifies (1) the CMN which he/she is reviewing includes Sections A and B;(2) answers in Section B are correct and the self-identifying information in Section A is correct.PHYSICIAN SIGNATURE ANDDATE:DME 001 – Dated 01/01/11After completion and/or review by the physician of Sections A and B the physician’s must sign anddate the CMN in Section B, verifying the Attestation appearing in this Section. The physician’ssignature also certifies the item(s) order is medically necessary for this patient.
SOUTH CAROLINA DEPARTMENT OF HEALTH AND HUMAN SERVICESMEDICAID CERTIFICATE OF MEDICAL NECESSITY FORMFOR POWER/MANUAL WHEELCHAIRS AND/OR ACCESSORIESSECTION A: MUST BE COMPLETED BY DME PROVIDER:(1) Recipient's name: Medicaid # (10 digits)(2) DOB / / ; Sex: HT: (in); WT: Date of Service:(3) Provider’s name: Provider’s DME # NPI#:(4) Street address: City: State: Zip: Local telephone #:(5) Provider's signature: Date:(6) LIST ALL PROCEDURE CODES THAT ARE ORDERED BY THE TREATING/ORDERING PHYSICIAN ON:PLEASE NOTE: FOR ALL PROCEDURE CODES THAT ARE COVERED, BUT DO NOT HAVE AN ESTABLISHED PRICE, YOU MUST INCLUDEMANUFACTURER PRICE LIST.I ATTEST THAT THE PT/OT THERAPIST AND/OR THE TREATING /ORDERING PHYSICIAN HAS NO FINANCIAL RELATIONSHIP WITH MYCOMPANY.SECTION B: ALL FIELDS IF APPLICABLE MUST BE COMPLETED BY TREATING/ORDERINGPHYSICIAN:(7) Diagnosis codes (ICD-9): Diagnosis(s):(8) Indicate the patient’s mobility limitation & explain how it interferes with the performance of activities of daily living (ADLs): Explain why a cane or walker is not sufficient to meet the patient’s mobility needs in the home: Explain why a manual wheelchair is not sufficient to meet the patient’s mobility needs in the home: How long has the condition been present and what is the patient’s clinical progression: Indicate any related diagnosis and all other interventions tried and the results: Has the patient ever used a walker, manual or power wheelchair and what were the results?(9) Please indicate the date that the patient was seen for the equipment/supplies prescribed:(10) Prescription Date:(11) Duration of need (Maximum of 12 months):I certify that I am the treating/ordering physician identified in Section B of this form. Any statement attached hereto has been reviewed and signed by me. I certifythat the medical necessity information is true, accurate and complete, to the best of my knowledge, and I understand that any falsification, omission, or concealment ofmaterial fact may subject me to civil or criminal liability. Additionally, I certify that the requested equipment/supplies are appropriate for the patient.(12) PRINT PHYSICIAN’S NAME: NPI #PHYSICIAN’S SIGNATURE: DATE / / (SIGNATURE AND DATE STAMPS ARE NOT ACCEPTABLE)PLEASE REFER TO THE MEDICAID CMN POLICY IN THE DME MEDICAID PROVIDER MANUAL.DME 003 – Dated 01/01/11
INSTRUCTIONS FOR COMPLETING THE MEDICAID CERTIFICATE OF MEDICAL NECESSITY FOR POWER/MANUALWHEELCHAIRS AND/OR ACCESSORIESSECTION A: MUST BE COMPLETED BY DME PROVIDERRECIPIENT’S NAME ANDMEDICAID #:Indicate the patient’s name and his/her Medicaid # (10 digits).PATIENT DOB, SEX, HEIGHT, WEIGHT:Indicate patient’s date of birth (MM/DD/YY) and sex (male or female); height in inches and weight inpounds.DATE OF SERVICE:Indicate the date of service (DOS). The date of service must be the same as the delivery date.PROVIDER‘S NAME, DME #AND NPI#:Indicate the name of the DME company (Provider name), Provider’s DME# and NPI#.PROVIDER’S PHYSICAL ADDRESSAND TELEPHONE NUMBER:Indicate the provider’s physical address (provider’s location) and telephone number.PROVIDER SIGNATURE AND DATE:Signature of DME provider representative and date.HCPCS CODES:List all HCPCS procedure codes for items ordered by the treating/ordering physician.Note: For all procedure codes that are covered, but do not have an established price, you mustinclude manufacturer price list.SECTION B: MUST BE COMPLETED BY TREATING/ORDERING PHYSICIAN:DIAGNOSIS CODES:In the first field, list the ICD-9 diagnosis code(s) that represent(s) the primary reason(s) for orderingthis item. In the second field, list the description(s) for each ICD-9 diagnosis code(s).QUESTION SECTION:This information is used to gather clinical information to help Medicaid determine the medicalnecessity for the item(s) being ordered. Answer each question which applies to the items ordered.DATE PATIENT WAS SEEN FOREQUIPMENT/SUPPLIES PRESCRIBED:Indicate the date patient was seen by the treating/ordering physician, nurse practitioner or physicianassistant for the equipment/supplies prescribed. The treating/ordering physician, nurse practitioneror physician assistant must examine the beneficiary within 60 days before prescribing equipmentand/or supplies.PRESCRIPTION DATE:Indicate the prescription date. The prescription date must be within 60 days of the date oftreating/ordering physician’s signature and the date the beneficiary was seen by the physician, nursepractitioner, or physician assistant. All MCMNs that are not signed within this time frame will bereturned (if submitted with a PA) or rejected (if attached to a claim) and the MCMN will be deemedinvalid.EST. LENGTH OF NEED:Indicate the estimated length of need (the length of time the physician expects the patient to requireuse of the order item) by filling in the appropriate number of months, up to 12 months. An MCMNcan be valid up to a maximum of 12 months from the date the patient was seen for theequipment/supplies prescribed.PHYSICIAN ATTESTATION:The physician signature certifies (1) the CMN which he/she is reviewing includes Sections A and B;(2) answers in Section B are correct and the self-identifying information in Section A is correct.PHYSICIAN SIGNATURE ANDDATE:DME 003 – Dated 01/01/11After completion and/or review by the physician of Sections A and B the physician’s must sign anddate the CMN in Section B, verifying the Attestation appearing in this Section. The physician’ssignature also certifies the item(s) order is medically necessary for this patient.
SOUTH CAROLINA DEPARTMENT OF HEALTH AND HUMAN SERVICES MEDICAID CERTIFICATE OFMEDICAL NECESSITY FORM FOR ORTHOTICS, PROSTHETICS AND DIABETIC SHOESSECTION A: MUST BE COMPLETED BY DME PROVIDER:(1) Recipient's name: Medicaid # (10 digits):(2) DOB: / / ; Sex: HT: (in); WT: Date of Service:(3) Provider’s name: Provider’s DME # NPI#(4) Street address: City: State: Zip: Local telephone #:(5) Provider's signature: Date:(6) LIST ALL PROCEDURE CODES THAT ARE ORDERED BY THE TREATING/ORDERING PHYSICIAN FOR ORTHOTICS, PROSTHETICS, AND/ORDIABETIC SHOES.PLEASE NOTE: FOR ALL PROCEDURE CODES THAT ARE COVERED BUT DO NOT HAVE AN ESTABLISHED PRICE, YOU MUST INCLUDEMANUFACTURER PRICE
SC Dept of Disabilities and Special Needs Head and Spinal Cord Injury Waiver Authorization for PERS Services : 02/2004 . HASCI 12-I : SC Dept of Disabilities and Special Needs Head and Spinal Cord Injury Waiver Authorization for Specialized Supplies and Adaptations 02/2004 . 219-DME . Medicaid Enrollment

![[MS-OFBA]: Office Forms Based Authentication Protocol](/img/3/ms-ofba.jpg)