Transcription
Detoxification andSubstance Abuse TreatmentA TreatmentImprovementProtocolTIP45
Detoxification andSubstance AbuseTreatmentA TreatmentImprovementProtocolTIP45U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICESSubstance Abuse and Mental Health Services Administration1 Choke Cherry RoadRockville, MD 20857
AcknowledgmentsThis publication was produced under theKnowledge Application Program (KAP) contract numbers 270-99-7072 and 270-04-7049with the Substance Abuse and Mental HealthServices Administration (SAMHSA), U.S.Department of Health and Human Services(HHS). Andrea Kopstein, Ph.D., M.P.H, KarlD. White, Ed.D, and Christina Currier servedas Government Project Officers.DisclaimerThe views, opinions, and content expressedherein are those of the consensus panel and donot necessarily reflect the views, opinions, orpolicies of SAMHSA or HHS. No official support of or endorsement by SAMHSA or HHSfor these opinions or for particular instruments, software, or resources is intended orshould be inferred.Public Domain NoticeAll material appearing in this report is in thepublic domain and may be reproduced orcopied without permission from SAMHSA.Citation of the source is appreciated. However,this publication may not be reproduced or distributed for a fee without the specific, writtenauthorization of the Office of Communications,SAMHSA, HHS.iiElectronic Access and Copiesof PublicationThis publication may be ordered from or downloaded from SAMHSA’s Publications OrderingWeb page at http://store.samhsa.gov. Or, pleasecall SAMHSA at 1-877-SAMHSA-7 (1-877-7264727) (English and Español).Recommended CitationCenter for Substance Abuse Treatment.Detoxification and Substance AbuseTreatment. Treatment Improvement Protocol(TIP) Series, No. 45. HHS Publication No.(SMA) 15-4131. Rockville, MD: Center forSubstance Abuse Treatment, 2006.Originating OfficeQuality Improvement and WorkforceDevelopment Branch, Division of ServicesImprovement, Center for Substance AbuseTreatment, Substance Abuse and MentalHealth Services Administration, 1 ChokeCherry Road, Rockville, MD 20857.HHS Publication No. (SMA) 15-4131Printed 2006Revised 2008, 2012, 2013, and 2015Acknowledgments
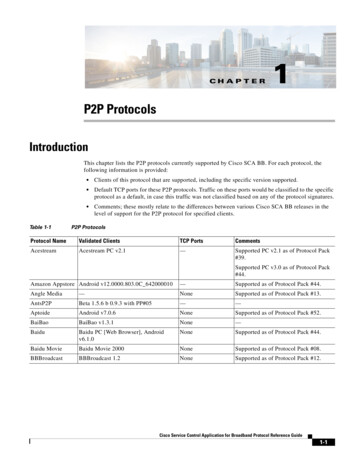
ContentsWhat Is a TIP?.viiConsensus Panel .ixKAP Expert Panel and Federal Government Participants .xiForeword .xiiiExecutive Summary .xvChapter 1—Overview, Essential Concepts, and Definitions in Detoxification.1Purpose of the TIP .1Audience .2Scope .2History of Detoxification Services.2Definitions.3Guiding Principles in Detoxification and Substance Abuse Treatment .7Challenges to Providing Effective Detoxification .8Chapter 2—Settings, Levels of Care, and Patient Placement .11Role of Various Settings in the Delivery of Services .11Other Concerns Regarding Levels of Care and Placement .20Chapter 3—An Overview of Psychosocial and Biomedical Issues During Detoxification .23Evaluating and Addressing Psychosocial and Biomedical Issues .24Strategies for Engaging and Retaining Patients in Detoxification .33Referrals and Linkages .38Chapter 4—Physical Detoxification Services for Withdrawal From Specific Substances .47Psychosocial and Biomedical Screening and Assessment .47Alcohol Intoxication and Withdrawal.52Opioids .66Benzodiazepines and Other Sedative Hypnotics rijuana and Other Drugs Containing THC .95Anabolic Steroids.96Club Drugs.97Management of Polydrug Abuse: An Integrated Approach.101Alternative Approaches .103Considerations for Specific Populations .105iii
Chapter 5—Co Occurring Medical and Psychiatric Conditions.121General Principles of Care for Patients With Co Occurring Medical Conditions .122Treatment of Co Occurring Psychiatric Conditions.136Standard of Care for Co Occurring Psychiatric Conditions .138Chapter 6—Financing and Organizational Issues .145Preparing and Developing a Program.145Working in Today’s Managed Care Environment.157Preparing for the Future.168Appendix A—Bibliography .169Appendix B—Common Drug Intoxication Signs and Withdrawal Symptoms .223Appendix C—Screening and Assessment Instruments .225Section I: Screening and Assessment for Alcohol Abuse .225Section II: Screening and Assessment for Alcohol and Other Drug Abuse .228Appendix D—Resource Panel.231Appendix E—Field Reviewers.233Index .237SAMHSA TIPs and Publications .243FiguresFigure 1 1 DSM IV TR Definitions of Terms .6Figure 1 2 Guiding Principles Recognized by the Consensus Panel .7Figure 2 1 Issues To Consider in Determining Whether Inpatient or OutpatientDetoxification Is Preferred .21Figure 3 1 Initial Biomedical and Psychosocial Evaluation Domains.25Figure 3 2 Symptoms and Signs of Conditions That Require Immediate Medical Attention.26Figure 3 3 Strategies for De escalating Aggressive Behaviors .28Figure 3 4 Questions To Guide Practitioners To Better Understand the Patient’s CulturalFramework .32Figure 3 5 The Transtheoretical Model (Stages of Change) .36Figure 3 6 Clinician’s Characteristics Most Important to the Therapeutic Alliance.38Figure 3 7 Recommended Areas for Assessment To Determine AppropriateRehabilitation Plans.40Figure 3 8 Strategies To Promote Initiation of Treatment and Maintenance Activities .42Figure 4 1 Assessment Instruments for Dependence and Withdrawal From Alcohol andSpecific Illicit Drugs.49Figure 4 2 Symptoms of Alcohol Intoxication .53Figure 4 3 Potential Contraindications To Using Benzodiazepines To Treat Alcohol Withdrawal .61Figure 4 4 Signs and Symptoms of Opioid Intoxication and Withdrawal .67Figure 4 5 Benzodiazepines and Their Phenobarbital Withdrawal Equivalents .77ivContents
Figure 4 6 Other Sedative Hypnotics and Their Phenobarbital Withdrawal Equivalents .78Figure 4 7 Stimulant Withdrawal Symptoms.79Figure 4 8 Commonly Abused Inhalants/Solvents.83Figure 4 9 DSM IV TR on Nicotine Withdrawal .86Figure 4 10 Items and Scoring for the Fagerstrom Test for Nicotine Dependence .87Figure 4 11 The Glover Nilsson Smoking Behavioral Questionnaire (GN SBQ) .88Figure 4 12 Some Examples of Nicotine Withdrawal Symptoms That Can Be Confused WithOther Psychiatric Conditions .89Figure 4 13 Effects of Abstinence From Smoking on Blood Levels of Psychiatric Medications .90Figure 4 14 The “5 A’s” for Brief Intervention .91Figure 4 15 Some Definitions Regarding Disabilities .111Figure 4 16 Impairment and Disability Chart .112Figure 4 17 Locating Expert Assistance.114Figure 6 1 Financial Arrangements for Providers.162Contentsv
What Is a TIP?Treatment Improvement Protocols (TIPs) are developed by the Center forSubstance Abuse Treatment (CSAT), part of the Substance Abuse andMental Health Services Administration (SAMHSA) within the U.S.Department of Health and Human Services (HHS). Each TIP involves thedevelopment of topic-specific best-practice guidelines for the preventionand treatment of substance use and mental disorders. TIPs draw on theexperience and knowledge of clinical, research, and administrative expertsof various forms of treatment and prevention. TIPs are distributed tofacilities and individuals across the country. Published TIPs can beaccessed via the Internet at http://store.samhsa.gov.Although each consensus-based TIP strives to include an evidence base forthe practices it recommends, SAMHSA recognizes that behavioral health iscontinually evolving, and research frequently lags behind the innovationspioneered in the field. A major goal of each TIP is to convey "front-line"information quickly but responsibly. If research supports a particularapproach, citations are provided. When no citation is provided, the information is based on the collective clinical knowledge and experience of theconsensus panel.vii
Consensus PanelNote: The information given indicates each participant's affiliation during the time the panel wasconvened and may no longer reflect the individual's current affiliation.ChairNorman S. Miller, M.D., FASAMProfessor and Director of Addiction MedicineDepartment of PsychiatryMichigan State UniversityEast Lansing, MichiganCo-ChairSteven S. Kipnis, M.D., FACPMedical DirectorRussell E. Blaisdell Addiction TreatmentCenterNew York State Office of Alcoholism andSubstance Abuse ServicesOrangeburg, New YorkWorkgroup Managers andCo-ManagersAnne M. Herron, M.S.DirectorDivision of State and Community AssistanceCenter for Substance Abuse TreatmentSubstance Abuse and Mental Health ServicesAdministrationRockville, MarylandRonald J. Hunsicker, D.Min., FACATAPresident/Chief Executive OfficerNational Association of Addiction TreatmentProvidersLancaster, PennsylvaniaRobert J. Malcolm, Jr., M.D.Professor of Psychiatry, Family Medicine,and PediatricsAssociate Dean for Continuing MedicalEducationCenter for Drug and Alcohol ProgramsInstitute of PsychiatryMedical University of South CarolinaCharleston, South CarolinaAnthony Radcliffe, M.D., FASAMChief of Addiction MedicineKaiser PermanenteSouthern California Permanente MedicalGroupFontana, CaliforniaCarl Rollynn Sullivan, III, M.D.ProfessorDirector of Addiction ProgramDepartment of Behavioral Medicine andPsychiatrySchool of MedicineWest Virginia UniversityMorgantown, West VirginiaNancy R. VanDeMark, M.S.W.Director of Colorado Social ResearchAssociatesArapahoe House, Inc.Thornton, ColoradoPanelistsLouis E. Baxter, Sr., M.D., FASAMExecutive DirectorPhysicians Health ProgramMedical Society of New JerseyLawrenceville, New JerseyKenneth O. Carter, M.D., M.P.H., Dipl.Ac.PsychiatristAcupuncture Detoxification SpecialistCarolinas Medical CenterCharlotte, North CarolinaJean Lau Chin, M.A., Ed.D., ABPPPresidentCEO ServicesAlameda, Californiaix
Charles A. Dackis, M.D.Assistant ProfessorDepartment of PsychiatryUniversity of Pennsylvania School of MedicinePhiladelphia, PennsylvaniaSylvia J. Dennison, M.D.Chief/Medical DirectorDivision of Addiction ServicesDepartment of PsychiatryUniversity of IllinoisChicago, IllinoisPatricia L. Mabry, Ph.D.Health Scientist Administrator/BehavioralScientistOffice of Behavioral and Social SciencesResearchOffice of the DirectorNational Institutes of HealthBethesda, MarylandxHendree E. Jones, M.A., Ph.D.Assistant ProfessorCAP Research DirectorDepartment of Psychiatry and BehavioralSciencesJohns Hopkins University CenterBaltimore, MarylandFrances J. Joy, R.N., CD, CASACManagerAlcohol and Drug Abuse UnitState of Missouri Department of Mental HealthFulton State HospitalFulton, MissouriConsensus Panel
KAP Expert Panel and FederalGovernment ParticipantsNote: The information given indicates each participant's affiliation during the time the panel wasconvened and may no longer reflect the individual's current affiliation.Barry S. Brown, Ph.D.Adjunct ProfessorUniversity of North Carolina at WilmingtonCarolina Beach, North CarolinaJacqueline Butler, M.S.W., LISW, LPCC,CCDC III, CJSProfessor of Clinical PsychiatryCollege of MedicineUniversity of CincinnatiCincinnati, OhioDeion CashExecutive DirectorCommunity Treatment & CorrectionCenter, Inc.Canton, OhioDebra A. Claymore, M.Ed.Adm.Owner/Chief Executive OfficerWC Consulting, LLCLoveland, ColoradoMichael Galer, D.B.A., M.B.A., M.F.A.Independent ConsultantWestminster, MassachusettsRenata J. Henry, M.Ed.DirectorDivision of Substance Abuse andMental HealthDelaware Health and Social ServicesNew Castle, DelawareJoel Hochberg, M.A.PresidentAsher & PartnersLos Angeles, CaliforniaJack Hollis, Ph.D.Associate DirectorCenter for Health ResearchKaiser PermanentePortland, OregonCarlo C. DiClemente, Ph.D.ChairDepartment of PsychologyUniversity of Maryland Baltimore CountyBaltimore, MarylandMary Beth Johnson, M.S.W.DirectorAddiction Technology Transfer CenterNational OfficeUniversity of Missouri—Kansas CityKansas City, MissouriCatherine E. Dube, Ed.D.Independent ConsultantBrown UniversityProvidence, Rhode IslandEduardo Lopez, B.S.Executive ProducerEVS CommunicationsWashington, DCJerry P. Flanzer, D.S.W., LCSW, CACChiefServices Research BranchNational Institute on Drug AbuseBethesda, MarylandHolly A. Massett, Ph.D.Academy for Educational DevelopmentWashington, DCxi
Diane MillerChiefScientific Communications BranchNational Institute on Alcohol Abuseand AlcoholismKensington, MarylandHarry B. Montoya, M.A.President/Chief Executive OfficerHands Across CulturesEspanola, New MexicoRichard K. Ries, M.D.Director/ProfessorOutpatient Mental Health ServicesDual Disorder ProgramsHarborview Medical CenterSeattle, WashingtonGloria M. Rodriguez, D.S.W.Research ScientistDivision of Addiction ServicesNew Jersey Department of Healthand Senior ServicesTrenton, New JerseyEverett Rogers, Ph.D.Center for Communications ProgramsJohns Hopkins UniversityBaltimore, MarylandJean R. Slutsky, P.A., M.S.P.H.Senior Health Policy AnalystAgency for Healthcare Research & QualityRockville, MarylandxiiNedra Klein Weinreich, M.S.PresidentWeinreich CommunicationsCanoga Park, CaliforniaClarissa WittenbergDirectorOffice of Communications and Public LiaisonNational Institute of Mental HealthKensington, MarylandConsulting MembersPaul Purnell, M.A.Social Solutions, L.L.C.Potomac, MarylandScott Ratzan, M.D., M.P.A., M.A.Academy for Educational DevelopmentWashington, DCThomas W. Valente, Ph.D.Director, Master of Public Health ProgramDepartment of Preventive MedicineSchool of MedicineUniversity of Southern CaliforniaAlhambra, CaliforniaPatricia A. Wright, Ed.D.Independent ConsultantBaltimore, MarylandExpert Panel
ForewordThe Substance Abuse and Mental Health Services Administration (SAMHSA) is the agency within the U.S. Department of Health and HumanServices that leads public health efforts to advance the behavioral healthof the nation. SAMHSA’s mission is to reduce the impact of substanceabuse and mental illness on America’s communities.The Treatment Improvement Protocol (TIP) series fulfills SAMHSA’s mission to reduce the impact of substance abuse and mental illness onAmerica's communities by providing evidence-based and best practiceguidance to clinicians, program administrators, and payers. TIPs are theresult of careful consideration of all relevant clinical and health servicesresearch findings, demonstration experience, and implementation requirements. A panel of non-Federal clinical researchers, clinicians, programadministrators, and patient advocates debates and discusses their particular area of expertise until they reach a consensus on best practices. Fieldreviewers then review and critique this panel’s work.The talent, dedication, and hard work that TIPs panelists and reviewersbring to this highly participatory process have helped bridge the gapbetween the promise of research and the needs of practicing clinicians andadministrators to serve, in the most scientifically sound and effective ways,people in need of behavioral health services. We are grateful to all whohave joined with us to contribute to advances in the behavioral healthfield.Pamela S. Hyde, J.D.AdministratorSubstance Abuse and Mental Health Services AdministrationDaryl W. KadeActing DirectorCenter for Substance Abuse TreatmentSubstance Abuse and Mental Health Services Administrationxiii
Executive SummaryThis Treatment Improvement Protocol (TIP) is a revision of TIP 19,Detoxification From Alcohol and Other Drugs (Center for SubstanceAbuse Treatment 1995d). It provides clinicians with updated informa tion and expands on the issues commonly encountered in the delivery ofdetoxification services. Like its predecessor, this TIP was created by apanel of experts (the consensus panel) with diverse experience in detoxi fication services—physicians, psychologists, counselors, nurses, andsocial workers, all with particular expertise to share.This diverse group agreed to the following principles, which served as abasis for the TIP:1. Detoxification, in and of itself, does not constitute complete sub stance abuse treatment.2. The detoxification process consists of three essential components,which should be available to all people seeking treatment: Evaluation Stabilization Fostering patient readiness for and entry into substance abusetreatment3. Detoxification can take place in a wide variety of settings and at a num ber of levels of intensity within these settings. Placement should beappropriate to the patient’s needs.4. All persons requiring treatment for substance use disorders shouldreceive treatment of the same quality and appropriate thoroughnessand should be put into contact with substance abuse treatmentproviders after detoxification.5. Ultimately, insurance coverage for the full range of detoxification ser vices is cost effective.6. Patients seeking detoxification services have diverse cultural and ethnicbackgrounds as well as unique health needs and life situations.Programs offering detoxification should be equipped to tailor treatmentto their client populations.7. A successful detoxification process can be measured, in part, bywhether an individual who is substance dependent enters andremains in some form of substance abuse treatment/rehabilitationafter detoxification.Among the issues covered in this TIP is the importance of detoxificationas one component in the continuum of healthcare services for sub stance related disorders. The TIP reinforces the urgent need for non xv
traditional settings—emergency rooms, medi cal and surgical wards in hospitals, acute careclinics, and others—to be prepared to partici pate in the process of getting the patient whois in need of detoxification services into treat ment as quickly as possible. Furthermore, itpromotes the latest strategies for retainingindividuals in detoxification while alsoencouraging the development of the therapeu tic alliance to promote the patient’s entranceinto substance abuse treatment. The TIP alsoincludes suggestions on addressing psychoso cial issues that may impact detoxificationtreatment, such as providing culturallyappropriate services to the patient popula tion.5. Level IV D: Medically Managed IntensiveInpatient DetoxificationMatching patients to appropriate care repre sents a challenge to detoxification programs.Given the wide variety of settings and theunique needs of the individual patient, estab lishing criteria that take into account all thepossible needs of patients receiving detoxifica tion and treatment services is an extraordi narily complex task. Addiction medicine hassought to develop an efficient system of carethat matches patients’ clinical needs with theappropriate care setting in the least restric tive and most cost effective manner. Patientplacement criteria, such as those publishedby the American Society of AddictionMedicine (ASAM) in the Patient PlacementCriteria, Second Edition, Revised, representan effort to define how care settings may bematched to patient needs and special charac teristics. These criteria—the five “AdultDetoxification” placement levels—define themost broadly accepted standard of care fordetoxification services. The five levels of carearePlacement will depend in part on the sub stance of abuse. The consensus panel suggeststhat for alcohol, sedative hypnotic, and opi oid withdrawal syndromes, hospitalization (orsome form of 24 hour medical care) is oftenthe preferred setting for detoxification, basedon principles of safety and humanitarian con cerns. When hospitalization cannot be pro vided, then a setting that provides a high levelof nursing and medical backup 24 hours aday, 7 days a week is desirable.1. Level I D: Ambulatory DetoxificationWithout Extended Onsite Monitoring2. Level II D: Ambulatory Detoxification WithExtended Onsite Monitoring3. Level II.2 D: Clinically Managed ResidentialDetoxification4. Level III.7 D: Medically MonitoredInpatient DetoxificationxviASAM criteria are being adopted extensivelyon the basis of their face validity, thoughtheir outcome validity has yet to be clinicallyproven. The ASAM guidelines are to beregarded as a work in progress, as theirauthors readily admit. They are an importantset of guidelines that are of great help to clini cians. For administrators, the standards pub lished by such groups as the JointCommission on Accreditation of HealthcareOrganizations and the Commission onAccreditation of Rehabilitation Facilities pro vide guidance for overall program operations.A further challenge for detoxification pro grams is to provide effective linkages to sub stance abuse treatment services. Patientsoften leave detoxification without followup tothe treatment needed to achieve long termabstinence. Each year at least 300,000patients with substance use disorders or acuteintoxication obtain inpatient detoxification ingeneral hospitals, while additional numbersobtain detoxification in other settings. Only20 percent of people discharged from acutecare hospitals receive substance abuse treat ment during that hospitalization. Only 15percent of people who are admitted to adetoxification program through an emergencyroom and then discharged go on to receivetreatment.The consensus panel recognizes that medical ly assisted withdrawal is not always necessaryor desirable. A nonmedical approach can behighly cost effective and provide inexpensiveExecutive Summary
access to treatment for individuals seekingaid. Young individuals in good health, with nohistory of previous withdrawal reactions, maybe well served by management of withdrawalwithout medication. However, personnelsupervising in this setting should be trained toidentify life threatening symptoms and solicithelp through the emergency medical system asneeded.The consensus panel also agreed on severalguidelines for nonmedical detoxification pro grams. Such programs should follow local gov ernmental regulations regarding their licensingand inspection. In addition, it is desirable thatall such programs have an alcohol and drug free environment as well as personnel who arefamiliar with the features of substance usewithdrawal syndromes, have training in basiclife support, and have access to an emergencymedical system that can transport patients toemergency departments and other sites for clin ical care.A major clinical question for detoxification isthe appropriateness of the use of medicationin the management of an individual in with drawal. This can be a difficult matter becauseprotocols have not been firmly establishedthrough scientific studies or evidence basedmethods. Furthermore, the course of with drawal is unpredictable and currently avail able techniques of screening and assessmentdo not predict who will experience life threat ening complications.Although it is the philosophy of some treat ment facilities to discontinue all medications,this course of action is not always in the bestinterest of the patient. Abrupt cessation ofpsychotherapeutic medications may causesevere withdrawal symptoms or the re emer gence of a psychiatric disorder. As a generalrule, therapeutic doses of medication shouldbe continued through any withdrawal if thepatient has been taking the medication as pre scribed. Decisions about discontinuing themedication should be deferred until after theindividual has completed detoxification. If,however, the patient has been abusing theExecutive Summarymedication or the psychiatric condition wasclearly caused by substance use, then therationale for discontinuing the medication isstrengthened. Finally, practitioners shouldconsider withholding medication that lowersthe seizure threshold (e.g., bupropion, con ventional antipsychotics) during the acutealcohol withdrawal period or at least pre scribing a loading dose or scheduled taper ofbenzodiazepine.Further studies are needed to confirm theclinical experience that psychiatric symptoms(including anxiety, depression, and personali ty disorders) respond to specific treatment ofthe addiction. For example, cognitive–behav ioral techniques employed in the 12 Steptreatment approach have been effective in themanagement of anxiety and depression associ ated with addiction. Although challenging,treatment of both addiction and co occurringpsychiatric conditions has proven cost effec tive in some studies.This TIP also provides medical informationon detoxification protocols for specific sub stances as well as considerations for individu als with co occurring medical conditionsincluding mental disorders. While the TIP isnot intended to take the place of medicaltexts, it provides the practitioner with anoverview of common medical complicationsseen in individuals who use substances.Disorders of several systems are discussed insome detail: gastrointestinal (including thegastrointestinal tract, liver, and pancreas),cardiovascular system, hematologic (blood)abnormalities, pulmonary (lung) diseases, dis eases of the central and peripheral nervoussystem, infectious diseases, and special mis cellaneous disorders. The TIP presents a cur sory overview of special conditions, modifica tions in protocols, and the use of detoxifica tion medications in patients with co occurringmedical conditions or mental disorders.Overall treatment of specific conditions is notaddressed unless modification of such treat ment is needed.xvii
The setting in wh
Joy, R.N., CD, CASAC. Manager Alcoholand Drug Abuse Unit Stateof Missouri Department of Mental Health FultonState Hospital Fulton,Missouri. x Consensus Panel. xi. KAP Expert Panel and Federal Government Participants. Barry S. Brown, Ph.D. Adj






![[MS-OFBA]: Office Forms Based Authentication Protocol](/img/3/ms-ofba.jpg)